My 18 year old son has ASD and has had a seizure disorder since he was 6 years old. He has tried virtually all anti-epileptic drugs. Either the side effects were unbearable, they made his seizures worse, or had no effect on his seizures. He was diagnosed with Eosinophilic Esophagitis. He is underweight and of short stature, and always has been. Mitochondrial tests show that complex II is working at 26% capacity. He is also autistic. He has tested positive for folate receptor antibody.
Over the years he has done several rounds of antibiotics, including Flagyl, which I have since learned that it significantly depletes the body of thiamine. He has also taken several rounds of Diflucan, Azithromycin, Vancomycin, Augmentin, Amox for various issues including candida, clostridia, gram negative gut bacteria, etc.
He is currently on Lamictal and just started Briviact for seizures. The Briviact causes anger and aggression issues. He currently deals with OCD tendencies. He was recently found to have bone density of 2.8 standard deviations below normal. This falls in the range of osteoporosis, but he has not been diagnosed with it because of his age.
He eats fresh and a lot of dried fruit, meats, raw and cooked greens, white rice, lots of cooked veggies, eggs. He also takes Lipothiamine 100 mg/day, Magnesium 550 mg, a multi-vitamin, calcium, vitamin D, and K, all at the direction of his doctors.
Childbirth and Infancy
M was born on July 9th 2005 7lbs 9oz. He was full-term. I had high blood pressure at 41 weeks and labor was induced. He would not drop into position and he became distressed and so was delivered via cesarean while I was under general anesthesia.
He spent 4 days in the NICU because he aspirated meconium and would not latch to feed. While in the NICU, he was administered antibiotics. He was formula-fed, not breast-fed.
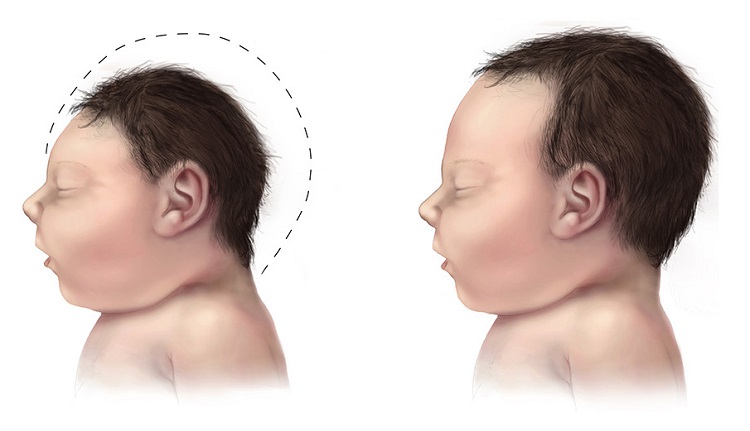
As an infant, the large size of his head was somewhat of a concern for the pediatrician. He was administered vaccinations according to the CDC guidelines for the first 12 months. He had infantile spasms off and on. He spiked a fever for every vaccination. Tylenol was administered. He received 3 doses of flu vaccine, accidentally, within 3 months.
He did not sleep well, and still doesn’t.
Initially, he was very precocious. As an infant, he would put puzzles together that were for much older children. He would complete sorting activities that were well beyond his age range. He did not babble and eye-contact was fleeting.
After his 18 month vaccination, he lost just about everything within 2 weeks. After these vaccinations, he couldn’t do his puzzles, bring food to his mouth, smile, couldn’t stand to be read to when he previously loved to be read to. He also developed a sensitivity to light and sound and cried a lot.
At 24 months, he was diagnosed with profound autism.
PANDAS/PANS and Eosinophilic Esophagitis
At age 10 years, he abruptly lost skills again and it was thought he had PANDAS/PANS as he had several strep infections treated with antibiotics. He did a several month long courses of Augmentin or Azithromycin to treat PANDAS/PANS. He had a severe trauma at age 11. He was horrifically abused by a school employee.
He has always been of short-stature nearing 5th percentile for height, and slightly overweight for his age, until age 14 when he started having symptoms of Eosinophilic Esophagitis. He was diagnosed with EoE at 15 and has struggled to keep his weight high enough as he dealt with the intense pain, fatigue, and esophagus issues with this condition. He is currently taking Dupixent for his Eosinophilic Esophagitis as the PPI and Budesonide slurry were not addressing the issues. So far Dupixent is allowing him to eat. His diet remains very restricted due to having so many trigger foods and he has almost no appetite.
He eats a lot of dried and fresh fruit. He loves greens, raw and cooked. He also eats meat, white rice noodles. He eats mostly an organic diet. He does occasionally enjoy candy.
Seizures
He developed seizures at age 6. These were controlled for a while on Depakote, but the side effects of Depakote were too much for him and so we had to stop. His seizures are now not controlled. He has 1-2 tonic-clonic seizures per week, plus several staring spells all throughout the day. Recent EEG showed abnormal spikes and discharges in the frontal and temporal lobes. It indicated his seizures involved many places on his brain. Brain surgery was being considered for seizures at this time, but ruled out as an option due to the nature of his seizures.
He has failed several other seizure meds including Vimpat, Zonegran, Aptiom, Topamax, Onfi, and others. He is currently on Lamotrigine and Epidiolex for his seizures. He also takes trazadone and gabapentin for sleep, although these do not consistently help him sleep. He is so consumed by fatigue and can hardly get out of bed even to walk across the room. With tons of encouragement he can do brief periods of school work. The meds cause him to lose focus and become frustrated. He seems to almost always be lost in a fog and unable to participate in basic conversations without losing focus or becoming too exhausted to continue. Each seizure will cause him to be in bed for 2-3 days. He has fallen many times going into a seizure and is now afraid to leave the safety of his bedroom. He will come out, but rarely.
He has intermittent issues with nystagmus. He had a bad case of COVID 2 years ago, which caused clusters of seizures and constant nystagmus.
He has an exaggerated startle response.
Despite It All
M is a sweet young man. He is brilliant. He loves animals. He tells everyone he sees that he is so happy to see them. He is working with a local legislator on how to improve rights for non-speaking people, especially in the court room. He is completing all of his high school courses at home with straight A’s and he is a published poet.
He does not speak, but he communicates by pointing to letters on an alphabet board. This is a skill that took him years to learn. He communicates at an age-appropriate level or higher. He is working, slowly, toward a standard high school diploma.
Postscript
Based upon what I have learned from this website, I discussed thiamine with our physician. It turns out, she heard Dr. Lonsdale speak years ago. She recommended 50mg of Lipothiamine. The entire time he was taking it, he had no seizures. I was not sure that it was thiamine or the meds until we ran out for about a week. The seizures returned, but as soon as we resumed the Lipothiamine, they disappeared again. He has been taking it again and now it has been 2 weeks without seizures. I don’t want to get my hopes up, but it could definitely be a piece of the puzzle. Are there others out there with similar experiences?
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Image by Gerd Altmann from Pixabay.