Every profession has its jargon that enables its practitioners to communicate relatively easily but is incomprehensible to those outside the indicated profession. This is most true in the medical profession, so I am about to explain a disease condition that has become extraordinarily common. I will begin by defining the word dysautonomia. “Dys” is a prefix meaning abnormal and “autonomia” refers to the autonomic nervous system. The autonomic system is the part of the nervous system that controls autonomic functions and behaviors that ensure survival. This includes, heart rate, respiration, digestion, temperature, even libido.
The autonomic system operates largely involuntarily and without conscious consideration. Many people are not aware that we have two types of nervous system. The one that we all understand is called “voluntary”, enabling us to carry out willed actions. This nervous system is controlled by the upper part of the brain known as the cortex, the latest part to be evolved, capable of thought and giving us those human abilities that are unique within the animal kingdom. In contrast, the lower part of the brain controls an involuntary “messenger system” that enables us automatically to adapt to the conditions of environment that we meet on a daily basis throughout life. The messenger system does not think. It acts automatically. The autonomic system is a “three channel system” that sends and receives signals to and from all parts of the body.
The Three Channels of the Autonomic System
The first channel connects with a bunch of glands known as the endocrine system. These are the glands that produce hormones, messengers borne by the blood to the body organs. This is a complex messenger system that adjusts, influences and modifies behavior. The other two channels are known as the sympathetic and parasympathetic systems. Between them, they provide direct communication that enables a given organ to react and participate in the symphony of adaptation. All work in a coordinated manner. Thus, the action of the autonomic nervous system, either by direct communication with an organ or by means of releasing a hormone, activate or deactivate all the organs in the body selectively.
Sympathetic System. This is best thought of as the action stimulating mechanism. Its best known reflex is known as “fight-or-flight”, activated by any form of mental or physical stress or threatened danger. It will accelerate the heart, deactivate the intestine, produce a sense of anxiety or panic, dilate the pupils in the eyes and raise the blood pressure, all things that you desire to happen if you are either fighting or fleeing from an enemy. It is designed for short-term action and consumes energy at an accelerated rate, particularly in the brain. It is important to note that this is a reflex, not a thought process. It is activated by a visual, auditory or tactile stimulus that is interpreted as danger. I think of this as a “stress input” that is answered by either physical or mental action in some form of self-preservation.
Reading a telegram that provides bad news triggers an emotional reflex that does not necessarily require physical action but is an obvious source of stress and the mental response is sympathetic and energy consuming. It may well induce accelerated heart rate, pallor and pupillary dilatation as a modification of a fight-or-flight reflex. Emotions are reflex, engineered by the lower brain and programmed according to the nature of the incoming stimulus perception. This in turn stimulates the thought processes of the higher brain that is capable of modifying the reaction. Sympathetic action of this nature is also activated by the release of adrenaline from its appropriate gland “and gives rise to what is sometimes called the ”adrenaline rush”.
Parasympathetic System. This is best thought of as “the rest-and-be-thankful” mechanism. It will decelerate the heart, activate the intestine, produce a sense of peace, constrict pupils of the eye and lower blood pressure, the very opposite of that produced by the other system. Our primitive ancestor could now roll a stone over the mouth of his cave and carry out the functions of the body after he has escaped from danger. He can now sleep, eat, indulge in bowel activity and experience a sense of peace. This also is not a thought process.
Dysautonomia: Autonomic Chaos
It is obvious that if the sympathetic and parasympathetic systems were activated together there would be chaos. Reflex sympathetic action under normal circumstances is balanced by a withdrawal of the parasympathetic action and vice versa. Thus, for example, accelerated heart rate is partly produced by withdrawal of the parasympathetic at the same time as it is accelerated by the sympathetic. This coordination is computed by the lower part of the brain. Under normal circumstances its action is modified by the upper brain that provides willpower under what might be called “advice and consent”. On the other hand, under urgent necessity, when danger is life threatening, the sympathetic system takes over the action completely, explaining why a soldier in battle may not be consciously aware that he has lost a finger until the action is completed.
If the reflex coordinated mechanism of the autonomic system is lost for any reason, it is referred to as dysautonomia. A medical textbook entitled “Dysautonomia” was edited by Sir Roger Bannister, then a London physician who was the first athlete to run the four-minute mile. The book describes many examples of this condition and deals with the genetic aspect. It never addresses the subject of nutrition, an oversight that introduces the clinical blindness of the modern physician to nutritional deficiency disease. This is in spite of the fact that the best example of dysautonomia is beriberi, long known to be caused by deficiency of thiamine (vitamin B1) by the ingestion of empty carbohydrate calories.
Hypoxia and Pseudo-hypoxia in Dysautonomia
The word hypoxia refers to lack of oxygen. Its most devastating effect is in the brain and particularly the lower brain that never sleeps. This is because the cells in that part of the brain have a heavy requirement for oxygen. As we all know, oxygen is delivered to all the 70 to 100 trillion body cells by the bloodstream and they consume it in the synthesis of energy. This consumption of oxygen is in turn dependent on the presence of thiamine and other vitamins. A deficiency of thiamine therefore produces the same clinical effect as hypoxia. For this reason, its deficiency causes what is sometimes known as pseudo-hypoxia (pseudo meaning false).
Since the lower brain controls the autonomic nervous system, we can now see how thiamine deficiency results in dysautonomia. Of course, as we all know, a complete lack of oxygen means death. We are here discussing the effects of a mild to moderate hypoxia or pseudo-hypoxia. The so-called TIA (transient ischemic attack) is an example of hypoxia because of a temporary failure of blood delivery to the brain. In most cases it is probably a brief contraction in the muscular wall of a major artery resulting in constriction of the artery. The irony is that I believe a common mechanism for TIA may involve arterial artery spasm from magnesium deficiency. It might well be obviated by taking a supplement of magnesium as a preventive. Thiamine and magnesium deficiency both produce the same effect by preventing the consumption of oxygen, thus stopping energy synthesis: hence the term pseudo.
Clinical Effects of Pseudo-hypoxia
There are many papers published in the medical literature in which a particular disease (for example lung cancer) is associated with dysautonomia. Each one of these manuscripts offers a case report in which the cause of this interesting but baffling association is unknown. My hypothesis is that pseudo-hypoxia gives rise to the dysautonomia whose symptoms are not recognized for what they represent, are ignored, or treated symptomatically and lead eventually to more cellular damage within a body organ that becomes an organic disease. If recognized in the early stages, diet correction and a few supplementary vitamins are all that is needed. If not, it is hypothesized that symptoms increase and reflect irreparable cellular damage. The constellation of symptoms is then referred to as disease A or B, e.g. Parkinson’s or Alzheimer’s.
It has now been shown that a common condition called “panic attacks” can be induced in a patient by the inhalation of air enriched with about 30% carbon dioxide, producing hypoxia. Therefore, this condition has nothing to do with Freudian psychology. It is a purely biochemical phenomenon, induced by hypoxia or pseudo-hypoxia. I recently met a friend with a story that I hear repeatedly. He was suddenly overcome by faintness while at work. It was associated with dizziness, lack of control and unconsciousness. He was conveyed by ambulance to the nearest emergency room where all the tests were negative and he was allowed to go home. Almost automatically this is referred to as psychosomatic disease as though the unfortunate patient is imagining or even inventing the obvious brain caused symptoms. There is little doubt that this represents a temporary period of hypoxia or pseudo-hypoxia that is extremely threatening to the individual for his or her future, since it indicates a state in the brain that can result in a recurrence, perhaps of greater severity.
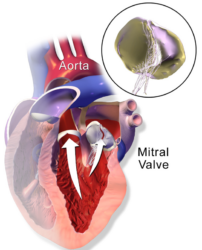
I learned later that this friend had received heart surgery many years before this incident. Since the primary organs affected by the pseudo-hypoxia of beriberi are the brain, the nervous system and the heart, perhaps pseudo-hypoxia was the underlying cause of the heart problem that led to surgery. I doubt that it was ever considered. The trouble is that I cannot tell a friend that perhaps all he has to do is to take a few vitamin supplements. He simply would not believe me. My credibility would be lost, possibly with the loss of friendship and my proffered advice, like the proverbial seed falling on stony ground. The concept is “outside the box” and does not conform to the medical model that exists in the minds of all of us.
What is particularly important to understand is that mild to moderate hypoxia or pseudo-hypoxia is itself a form of stress and triggers the fight-or-flight reflex. This is quite logical since a decreased oxygen concentration is dangerous and even life-threatening. Under these conditions the lower brain is more easily activated and the resulting action fails to heed the advice and consent provided by the upper brain. Thus, a child or adolescent consuming empty calories, will be thiamine deficient and his brain susceptible to periods of pseudo-hypoxia, particularly when experiencing other energy demanding stressors. The hypoxia will affect autonomic regulation, which will manifest in a number of seemingly unrelated symptoms, that include digestive issues, attentional deficits, unexplained aches and pains and perhaps most notably in children, behavioral difficulties represented by extreme emotional lability. The easiest way to produce pseudo-hypoxia is by the widespread consumption of carbohydrate and fatty foods (e.g. doughnuts) representing empty calories, so commonly associated with the consumption of high sugar content beverages. Sugary foods are not only devoid necessary nutrients, but the sugar itself forces what thiamine stores that exist out of the cells. Could high calorie malnutrition be responsible for some of the otherwise inexplicable violence reported almost daily in the news media? It is biochemically possible. Perhaps an easier question to answer, could thiamine deficiency and the resultant hypoxia be responsible for the myriad of autonomically controlled systems currently labeled dysautonomia? Possibly.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Image creating using Canva AI.
This article was published originally on February 13, 2017.