In the recent news, it was announced that Key West, Florida will ban the use of sunscreens. This reflects how photosensitizers like oxybenzone in sunscreens can alter redox balance (the production and removal of reactive oxygen species) to inflict severe oxidative stress resulting in widespread DNA damage in living organisms like coral reefs. The world has lost close to half of its coral reefs in the past 30 years. It is estimated that close to 90% of all coral reefs will be dead by the year 2050. In last week’s post, I wrote about the potential connection between the coral reef die offs, electromagnetic radiation and vitamin C. This week, I would like explore what happens when we add sunscreen to the mix. As we will see, sunscreen stresses an already stressed organism by increasing the accumulation of free radicals, reactive oxygen species or ROS. The chemicals in sunscreen negatively skew what is called the redox balance e.g. the balance between oxidation and reduction. The net result of which is an accumulation of ROS. Interestingly enough, as I described in the previous article, vitamin C buffers that response. The problem, as with human health, nutrient status in these organisms has been depleted.
Coral Reef Health
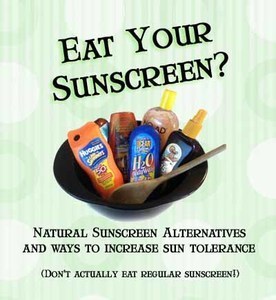
Coral reefs have been dying as a result of sunscreens in their environment due to the way oxybenzone works. Oxybenzone has been found to cause DNA lesions in coral reefs, and the damage was found to be higher with increased sunlight. You would think that is a contradiction because sunlight is supposed to be beneficial to all living organisms. What you may not be aware of is all photoreactions can generate a lot of oxidative stress, which if uncontrolled, will eventually lead to DNA damage and cell death. Our bodies have an exquisite redox system in place to control photochemical reactions. But what about coral reefs?
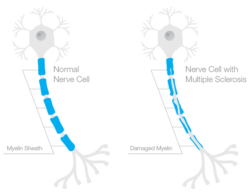
Oxybenzone, also known as BP-3 or benzophenone-3, belongs to a class of photoreactive ketones called benzophenones. Oxybenzone is able to absorb UVB in addition to blocking UVA, hence its use in sunscreens. However, being photoreactive means when this ketone is activated by high powered light frequencies in the UVB range, it will form a highly reactive triplet-state radical that will conjugate with other molecules around it. The part that makes oxybenzone even more dangerous as a photoreactive agent is that it does not undergo decomposition to an inactive form if it does not couple to target molecules. Instead, it degrades from the photo-excited state back to its initial state, so it can be once again photolyzed to an active state. Benzophenone will stay active until the free radical is quenched by free radical scavengers to stop the cycle.
What quenches free radical scavengers? Vitamin C has been shown to quench free radicals generated by benzophenones. Scientists has recently discovered that coral reefs have the ability to produce vitamin C . We also know that ascorbic acid content in coral reef could have been depleted due to environmental stress factors, including that of man made electromagnetic radiation. What happens when there is not enough ascorbate to quench photoreactions of oxybenzone? Dangerous free radicals like superoxide, hydrogen peroxide and hydroxyl radicals will be formed .
Photoreactors like oxybenzone are dangerous because they generate ROS when activated by light. It is interesting to note that one study found benzophenone induced extensive necrosis in coral under light exposure, but the same compound in darkness induced autophagy and autophagic cell death. There is no doubt that an organism’s redox balance is critical to its survival against oxidative stress, under both light and dark conditions.
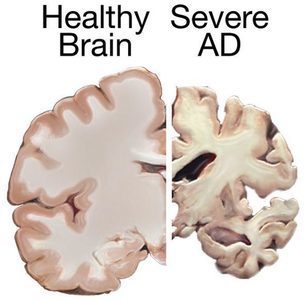
Electromagnetic radiation causes diseases in humans by generating oxidative stress, knocking our protective redox system out of balance, in the same way as oxybenzone creates ROS leading to DNA damage that eventually kills coral reefs.
Improving your redox is probably the most important thing one can do to improve health across the board. Like the coral reefs, the human organism requires adequate nutrients to facilitate these processes. How does our redox system really work to defend us against EMR and photoreactive compounds like oxybenzones and drugs like fluoroquinolones, or even endogenous photosentizers like melanin, lipofuscin, and retinals? How does vitamin C protect us from DNA damage by improving redox? I will tackle these subjects in subsequent articles. For now, however, consider what redox really means and how you can improve it in my latest article, which is also the sequel to the Birefringence article.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
This article was published originally on February 25, 2019.