Everyone knows that we need oxygen to live. Few know or care what the body does with it. Although everyone knows that it is extracted from the air by the lungs and carried by the blood to body tissues, it is left to scientists to understand what happens to it in the 50 to 100 trillion cells that make up an adult human body. The reaction that makes it possible for oxygen to maintain life is called oxidation. This reaction takes place in the mitochondria and produces energy that is used by each cell to carry out its program of function. Perhaps we can understand this better by using an analogy.
Car Engines and Human Engines: Each Need Fuel
A car uses gasoline as a fuel. It is ignited by a spark plug that causes a controlled explosion in a cylinder. This drives a piston that passes the energy through a series of mechanical levers known collectively as the transmission. It is the conversion of chemical energy in gasoline to what Newton called kinetic energy that enables the car to move. The machine that does this is an engine. Perhaps it stretches the imagination to state that the body works on exactly the same principles. It is the details that make the difference. Oxidation is the equivalent of explosion in the cylinder. In other words, it is combustion. Now we have to compare it to the relatively simple mechanism of explosion.
First, combustion is merely the union of oxygen with a fuel. If we do not carry the reaction out in some controlled way, the energy is dissipated as heat into the surrounding air. In a car, the cylinder encloses the combustion and forces the energy into the transmission. In the body it is controlled in a much more complex way. Yes, heat is produced and is used to make us “warm blooded creatures” but there is no noise, fire or smoke as in the car engine. The energy is guided through an ingenious series of chemical reactions in what we might term “the engines of the cell”.
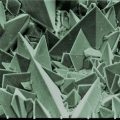
Mitochondria: The Engines in Our Cells
Each cell has a whole series of “engines” called mitochondria and it is in these organelles where oxidation occurs. A mitochondrion is so small that its structure can only be seen with the aid of an electron microscope and yet it is in each of the millions of cellular mitochondria where energy is produced for the use of each cell to perform its designed function. The usual fuel for this is glucose and it is not surprising that people have concluded that the consumption of sugar provides “quick energy”.
Good Sugar and Bad Sugar: Mitochondria Know the Difference
When sugar is ingested in its proper form, meaning as it is found in nature, it is stored in the liver and muscles as glycogen, a complex substance built up by sticking glucose molecules together, making something that looks like a miniature tree. As fuel is required, the glycogen is broken down and released as glucose into the blood. This requires an enzyme and there is an inborn error of metabolism where this enzyme is missing. The affected infant is found to have an enlarged liver stuffed with glycogen, together with low blood sugar, a situation that is not compatible with life and the patient dies in infancy.
Blood glucose is absorbed from the blood into cells under the influence of insulin and then goes into an ingenious “pipeline” that processes it. The beginning of this process requires a number of B group vitamins. There is a well known nutritional disease known as beriberi where the carbohydrate load is too great for this action to occur efficiently. It is now known that vitamin B1 is insufficient to meet the caloric demand and is the key to understanding the disease and how it is treated, a discovery that took many years to unravel.
Let us look again at the simpler method by which gasoline is ignited in a car. An electrically energized spark plug is used to ignite the fuel as it is passed into the cylinder by carefully controlled mechanisms. Some people will remember that cars once had a gadget called a choke, used for starting the cold engine. This allowed gasoline to flow into the cylinder with a relative deficiency of air, the so-called “rich” mixture. When the engine was warm the choke was automatically removed and the mixture weakened by allowing more air and less gas into the cylinder. If the choke mechanism stuck, there would be an excess of black smoke issuing from the exhaust pipe and the engine would not run properly. The smoke represents the hydrocarbons in gas that have not been ignited and a simple equation shows us why:
Fuel + Oxygen + Catalyst = Energy
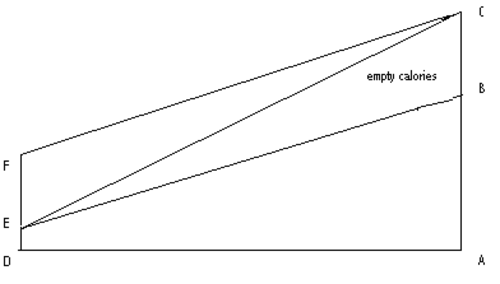
The Figure shows the ratio of calories to B vitamins in a healthy diet. The line AB represents the calorie intake (protein, fat and carbohydrate) and the line ED the vitamin intake that enables its efficient processing. If the line AB is extended to C (line AC) without the increase in vitamin intake, the triangle BCE represents “empty calories” equivalent to a “choked engine”. The remedy is obvious: we can extend line DE to F, thus restoring the ratio as in line FC, reduce the calories back to line AB, or meet each other half way (not shown).
Beriberi: Bad Sugar and Empty Calories
Beriberi is caused by consuming empty calories (triangle BCE), where the line AC represents carbohydrate calories and ED the corresponding ingestion of vitamin B 1. (thiamin). The disease, throughout history, has been primarily in Eastern countries where the diet has been white rice based, particularly in times of greater affluence. This is because the grain in rice is starch and the cusp contains the necessary vitamins. When the Chinese peasants became more affluent they would take their rice to a rice mill where white rice was produced by removing the cusps. This was because it looked better when served to their friends, thus demonstrating their new found affluence. Outbreaks of beriberi were always associated with an increase in consumption of white rice.
What is the lesson to be learned from this in our modern age where diseases like beriberi have been thought to be of only historical interest? Think of the enormous load of simple carbohydrate consumed by millions in the U.S. Everything supplied by the food industry is sweetened or it would not sell. White bread (the equivalent of white rice), cookies, pastry in general, ice cream, soft drinks, desserts, tomato ketchup——— the list goes on and on! Even the vitamin enrichment indicated on the label is insufficient. Obesity, often associated with inflammatory disease, is affecting millions. Our health bills are threatening us with national bankruptcy and we wonder why we are being “hit” with so many diseases and health catastrophies. Pockets are being lined with money made from a variety of reducing diets and pills.
Diet is Everything: Feed your Mitochondria
That is why I have a standard answer to every query that I get about diet. Eat only nature made food and the less that it is handled by mankind the better. The balance of calories and vitamins is automatically produced. If the food had not been available when life started on Earth animal evolution could not have occurred and we would never have survived. Granted, unfortunately with population explosion, fresh food of this nature is expensive and we have all given up back yard gardening The First Lady has shown the example. Will we take a “leaf from her book” and acknowledge that a lot of our health is in our own hands.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Image by Sumanley xulx from Pixabay.