I live in a retirement community. In my everyday discussions with fellow residents, I find that the idea of energy metabolism as the “bottom line” of health is almost completely incomprehensible. Since my friends are all well-educated professional people, I came to the conclusion that few people really have an idea about energy. For example, we talk about people who indulge in physical sports being energetic, while people sitting behind a desk are classed as sedentary. What we fail to realize is that mental processes require even more energy than physical processes. Both physically and mentally active people consume energy, so it is obvious that some kind of attempt must be made to talk about energy as it applies to the human body.
Hans Selye and the Stress Response
I will begin by giving an outline of the work that was performed many years ago by a Canadian scientist by the name of Hans Selye. Originally he was a Hungarian medical student. Some of the teaching was done by presenting individual patients to the class of students. The professor would describe the details of the disease for each person. What interested Selye was that the facial expression of each patient appeared to him to be identical. He came to the conclusion that this was the facial expression of suffering, irrespective of the nature of the disease. He referred to this as the patient’s response to what he called “stress”. He decided to study the whole concept of stress. He immigrated to Canada and in Montréal he set up a research unit that came to be called “The Research Institute of Stress”.
Of course, Selye could not study human beings and his experiments were performed on literally thousands of rats. He subjected them to many forms of physical stress and detailed the laboratory and histological results. He found that each animal would begin by mustering the well-researched fight-or-flight reflex. If the stress was continued indefinitely, the metabolic resistance of the animal gradually decayed. He called this ability of the animal to resist stress the “General Adaptation Syndrome” and came to the conclusion that it was driven by some form of energy. If and when the supply of energy was exhausted, he found laboratory changes in blood and tissues that were listed carefully. Although extrapolating this information from animal studies, he ended up by saying that humans were suffering from “diseases of adaptation” and that they were the result of a failure to adapt to the effects of life stresses.
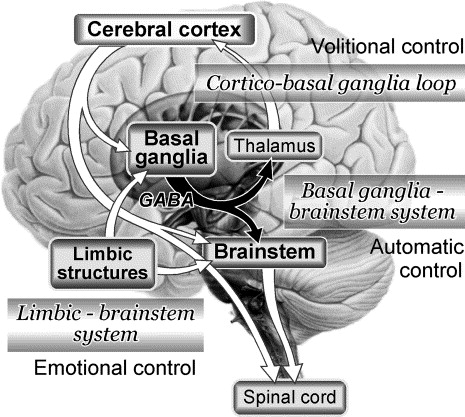
My addition to this is that it would have been better to describe them as “the diseases of maladaptation”, meaning that humans have to have some form of energy to meet life. If there is energy failure, disease will follow. The remarkable thing is that energy production in the human body was virtually unknown in Selye’s time, so his conclusion was a touch of genius. The mechanism by which energy is produced in the cells of the body is now well-known. We know that energy consumption is greatest in the lower part of the brain and the heart, organs that work 24 hours a day throughout life. The lower part of the brain that organizes and controls our adaptive capabilities is particularly energy consuming. So before we begin to think about energy as a driving force, let us consider what we mean by stress and how we adapt to it.
Human Stress: Surviving a Hostile Environment
We all live in an environment that is essentially hostile. We have to adapt to natural changes such as cold, hot, wet and dry. We are surrounded by enemies in the form of microorganisms and when they attack us, we have to set up a complex mechanism of defense. Add to this the possibility of trauma and the complexity of modern civilization, involving business and life decisions. We possess the machinery that enables us to meet these individual stresses, meaning that we are adapting. Health means that we adapt successfully and that is why “diseases of maladaptation” makes a lot of sense. Obviously, the key is that the machinery requires energy.
Energy Metabolism, Physics, and Chemistry
First of all, let us begin by trying to define energy. The dictionary describes it as “a force” and the only way in which we can appreciate its nature is by its effects. It is not a substance that we can see but the effects of light energy enable us to have vision. The old riddle might be mentioned; “Is there a sound in the forest when a tree falls?” The answer is of course that the only way that the resultant energy can be perceived is when it is felt by the human ear. Even that is not the end of the story, because the ear mechanism has to send a message to the brain where the sound is perceived. Thus, there is no sound in the forest when a tree falls. It is the perception of a form of energy, a force that impacts on the ear of any animal endowed with the ability to hear. Energy can be stored electrically in a battery or as heat energy in a hot water bottle, but the inevitable process is that the energy drains away. A hot cup of coffee cools. A battery gives up its stored energy and becomes just “another lump of matter”.
For example, if a stone is rolled up a hill, its natural tendency would be to roll down the hill again. Whatever force is being used to roll the stone up the hill is known as “potential energy”. In other words, there has to be a constant supply of energy as long as the stone is moving up a gradient against gravity. When it reaches the top, we say that the potential energy is being stored in the stone. It is the equivalent of electricity being stored in a battery. The “potential energy”, however, requires an electrical force to “electrify” the battery. The potential energy in the stone can be released by allowing it to roll down the hill and Newton called this kind of energy “kinetic” (the use of a force to produce movement). The force that is being used is of course the effect of gravity and the stone becomes stationary when it gets to the bottom of the hill. The use of gravity as the source of energy is simply wasted, but note that gravity has not changed. It is still available for use. Let us take a simple example of this energy being used for a purpose. Suppose that there is a wall at the bottom of the hill and a farmer wishes to create a gate. In a fanciful way he could use the stone to create a gap in the wall. The gap in the wall is the observable mark of the effect produced by consumption of kinetic energy.
The body consists of between 70 and 100 trillion cells, each of which has a special function. Each is a one-celled organism in its own right and in order to perform their function they need a constant supply of energy. This is developed by complex body chemistry. The “engines” in each cell are called mitochondria and one of their many different functions is to synthesize energy. The energy that is developed is stored in a chemical substance known as adenosine triphosphate (ATP) and in order to understand this a little more, perhaps we should think of the Newtonian analogy for comparison. The Newtonian hill is replaced by an electronic gradient and the stone by the chemical ATP
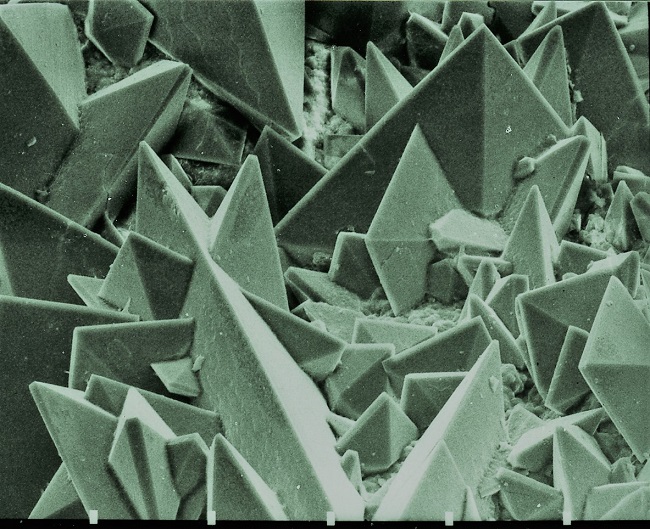
Of Mitochondria and ATP
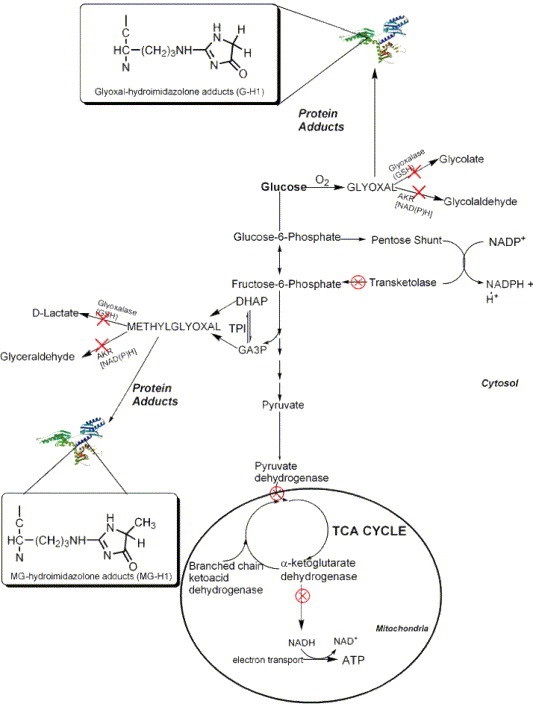
Cellular energy is produced in the mitochondria by oxidative metabolism. This simply means that a fuel (glucose) combines with oxygen but, like any fuel, it has to be ignited. The best way to analogize that is to say that thiamine can be compared with a spark plug that ignites gasoline in a car. It “ignites” glucose. The resultant energy is used to add a phosphate molecule to adenosine three times to make ATP (the electronic gradient). We have “rolled an electronic stone up an electronic hill”. As the adenosine donates phosphate molecules, it becomes adenosine monophosphate (AMP) that must be “rolled uphill again”. As it is “rolling down the electronic hill”, it is transferring energy. Therefore, ATP can be thought of as an energy currency. Note that there must be a continuous supply of fuel (food) that must contain the equivalent of a spark plug (thiamine) in order to maintain an energy supply with maximum efficiency.
The loss of any one of a huge number of components in food that work in a team relationship with thiamine, lowers the energy maximum. That is why thiamine deficiency has been earmarked as the major cause of a disease called beriberi that has haunted mankind for thousands of years. Its deficiency particularly affects the lower part of the brain and the heart because of their huge energy demand. Since the lower brain contains the control mechanisms that enable us to adapt to the environment, as depicted above, it is easy to see that we would be maladapted if there is energy deficiency, just as Selye predicted. In fact, one of his students was able to produce a failure of the General Adaptation Syndrome by making his experimental animals thiamine deficient. It also suggests that a lot of heart and brain disease is really nothing more than energy deficiency that could be easily treated in its early stages. If the energy deficiency is allowed to continue indefinitely because of our failure to recognize the implications, it would not be surprising that changes in structure would develop and produce organic disease.
Health and Disease in the Context of Energy
With this concept in view, the present disease model looks antiquated. There are only three factors to be considered. The first one is obviously our genetic inheritance. If it is perfect, all it requires is energy to drive it. However, DNA is probably never perfect in its formation. It may not be imperfect enough to cause disease in its own right, but a slight imperfection would constitute what I call “genetic risk”, causing disease in association with a stressor such as an otherwise mild infection or trauma.
Suppose that a given patient died from an infection (think of the 2018 flu).The present medical model would place the blame on the pathogenic virulence of the virus without considering whether malnutrition played a part by failing to produce sufficient energy for the complex immune response. Therefore, the second factor to be considered is the perfection of the fuel supply and that obviously comes from the quality of nutrition. Stress (the viral attack or non-lethal trauma) becomes the third consideration, since we have shown that an adequate energy supply is required for adapting on a day-to-day basis. There is even a new science called epigenetics in which it has been shown that nutrient components can be used to upgrade genetic mistakes in DNA. A fanciful interpretation of these three factors, genetics, nutrition and stress can be portrayed by the use of Boolean algebra. This is a mathematical representation as interlocking circles. The area of each circle can be easily assessed, marking their relative importance. The interlocking area between any two of the three circles and that of the three circles together completes the picture. It becomes easy to perceive how a prolonged period of stress can impact health. The present flu epidemic may be an example of the Three Circles of Health in operation, explaining why some people have only a mild illness while others die. Could the appalling nutrition in America play a part?
Why Thiamine
The pain produced by a heart attack has always been a mystery in explaining why and how it occurs. The answer of course is that pain is always felt by sensory apparatus in the brain. The brain is able to identify the source of the signal as coming from the heart but cannot interpret the reason. I am suggesting that in some cases, the heart is having difficulties from energy deficiency and notifying the brain. A coronary thrombosis would introduce local energy deficiency, but other methods of producing energy deficiency would apply. It is logical to assume also that brain disease is a manifestation of cellular energy deficiency. That is why I had found that so many children referred to me for various mental conditions responded to megadoses of thiamine. It is also why I had found that so much emotional disease was related to diet and not to poor parenthood.
I recently came across a patient that I had seen many years ago when he was a child. He had a diagnosis of Tourette’s syndrome, made elsewhere. I treated him with megadoses of thiamine and his symptoms resolved completely. Medical skepticism would answer this by calling it a placebo effect, but since this effect is well-known, it must have a mechanism. For many years I have believed that therapeutic nutrition “turns on” this effect by enhancing cellular energy. A small group of physicians known as “Alternative Medicine Practitioners” use water-soluble vitamins, given intravenously, irrespective of the acceptable clinical diagnosis. For example, I remember a young woman who came to see me with a diagnosis of “Thrombocytopenic Purpura”. This disease is a loss of cellular elements known as platelets and it had resisted orthodox treatment for years. I gave her a series of intravenous injections of water soluble vitamins with complete resolution of the problem. I must end by stating that healing is a function of the body. The only way that a healer can be justifiably recognized is by supplying the body with the ingredients that it requires to carry out the healing process. Perhaps spontaneous healing, as for example initiated by religious belief, is an ability to muster those ingredients that are present, but hitherto unused.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
This article was published originally on February 14, 2018.













 Indeed, there have been many relapses over the years, where her health declines significantly and requires extended periods of recovery. Nevertheless, she is able to recover and that is remarkable.
Indeed, there have been many relapses over the years, where her health declines significantly and requires extended periods of recovery. Nevertheless, she is able to recover and that is remarkable.