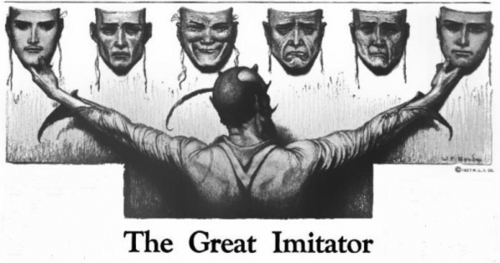
In the 5 years since Dr. Lonsdale and I published our book: Thiamine Deficiency Disease, Dysautonomia, and High Calorie Malnutrition (and 50 years since Dr. Lonsdale first began working with thiamine) recognition of the role of thiamine in health and disease have increased steadily year over year. Sales of the book double each year. Admittedly, the numbers were low and remain low in comparison to other popular topics, but the increase in awareness is heartening. Unfortunately, much of this awareness has not reached the medical profession. We regularly see reports in the medical literature boasting recognition of ‘rare’ cases of thiamine deficiency diseases like beriberi and Wernicke’s. If only physicians knew how common these conditions were and that they are only rare because we are not looking. Insufficient thiamine is Hiding in Plain Sight.
A New Book
In 2020, a UK physician by the name of Jo Dixon published a new book on thiamine deficiency, a personal account of her declining health, her discovery of thiamine, and her efforts to get treatment and spread the word. The book, called The Missing Link in Dementia, A Memoir, documents her journey. Unfortunately, she neither mentions thiamine in the title, the description, or even in the text until halfway through. One would not know the book is about thiamine until one reads it or unless it is recommended, so I will recommend it here. This would be a great starter book for someone beginning their health journey.
She has a second book listed on Amazon, Swimming in Circles that I have not read, but I suspect it details thiamine deficiency in fish in other animal populations.
While I would have preferred her to mention thiamine deficiency in the title or introduction, I found the book quite telling of the lengths one has to go to uncover this deficiency, even as a physician. Her case, unfortunately, is highly typical of what we see in patients everywhere. She had longstanding bowel dysfunction, which limited her ability to eat and maintain nutritional status. She led a busy life as a physician and mother of four children, which put pressure on thiamine stability. Even so, she functioned quite well for a long time. It wasn’t until her health took a severe turn for the worse that thiamine deficiency was recognized. Like others who develop issues with thiamine, she was forced to diagnose herself. No other physician, and she saw many, could provide any answers to her declining health. She had to figure it out herself. She was also forced to treat herself. Fortunately for her, she convinced a physician friend to provide IV thiamine, a protocol that was not accepted by her hospital and one she could not readily provide to other patients when she identified their deficiencies.
All of this is typical. We believe that thiamine deficiency was solved and thus any cases that do appear must be rare (to a tee, most case reports include ‘rare’ in the title or introduction). In reality, they are only rare because we do not look for them. We believe falsely that thiamine deficiency emerges acutely, and while it does in some cases, mostly it sits in the background, quietly and insidiously destroying one’s health. We have cases of high functioning individuals whose health begins to decline and whose thiamine levels are tested as low and should merit treatment but ignored for years as not being pertinent. And those are the lucky ones. Most physicians refuse to test for thiamine.
Thiamine deficiency is easily treatable if recognized early. It becomes more complicated as the years pass, and it is impossible if we never bother to look.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, and like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Photo by Alif Caesar Rizqi Pratama on Unsplash.