A few months ago, I received a book from a doctor who had retired from his specialty in obstetrics and gynecology. It was accompanied by a letter that began as follows, “I am writing to you, because I have found another mortal being who is particularly interested in the biological activities of thiamine. I had previously thought that I was nearly the lone believer in the benevolent effects of thiamine, particularly for the treatment and prophylaxis of the toxemias of pregnancy and its many associated problems”. In this letter, he went on to tell me that he had hired himself out, in his retirement, to the government of the Commonwealth of the Northern Mariana Islands “to improve upon their system of obstetrical care”.
Severe Preeclampsia
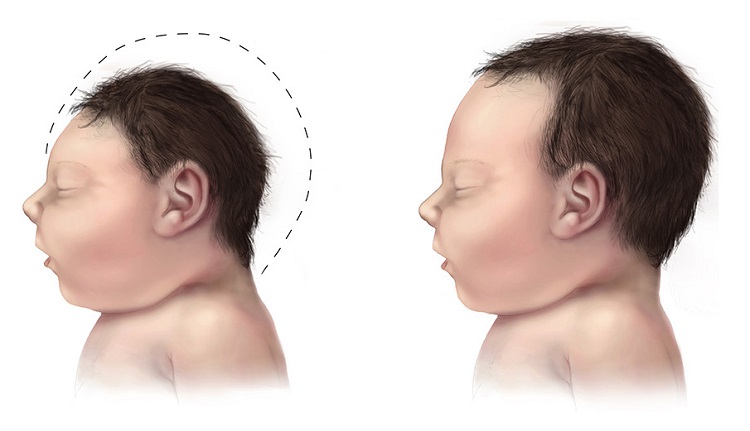
On his first day he attended an introductory meeting with a group of island doctors who were all American Board Certified in their specialties. Their purpose was to introduce him to a patient who was 36 weeks pregnant. He described her as “essentially moribund” with severe preeclampsia, gestational cardiomyopathy, and some separation of the placenta (preeclampsia is the term used for severe pregnancy toxemia and cardiomyopathy is the term used for a sick heart. Separation of the placenta would mean that there would be bleeding into the uterus). She was so sick that she had orthopnea (breathlessness while lying flat on her back. She could only breathe when sitting up in bed, a characteristic of heart failure). Spontaneous labor and delivery, he said, most likely would cause maternal and fetal death and that she would fail to come through a cesarean section. All in all, this was considered by all of the island doctors concerned to be a hopeless case. He suggested that she had beriberi, the vitamin B1 deficiency disease. The letter went on to say “in a private huddle the doctors decided that if the patient died while they were holding me up, they would be found solely guilty, so with anger, sneers and audible comments they told me to go ahead!” He gave the woman 100 mg of thiamine daily in a pill and she was physiologically cured in six days, sleeping flat and hiking the long halls for exercise to shake off her prolonged immobilization. On the seventh day, because of fetal distress, she was subjected to cesarean section, with the delivery of a 3 lbs. 12 oz. baby with a normal Apgar score.
Yes, I know how many will react to this. They will say that this patient was on a tropical island where beriberi was much more likely. This could not happen in America where the science of nutrition is so well known and where all the foods are enriched with vitamins. Also, they might think that the doctor was deluded into thinking that all forms of toxemia were really beriberi and that he had treated this disease rather than toxemia. So the doctor started the clinic patients on prophylactic mega-thiamine for the second and third trimesters, preventing development of every type of toxemia completely, including eclampsia, preeclampsia intra-uterine growth retardation, premature delivery, fetal death, premature rupture of membranes, placenta previa and gestational diabetes, among other possible complications. Again, the reader might well say that these were all patients on a tropical island. Consider however that this doctor had spent his professional lifetime in his attempt to bring healthy babies into the world. He was conversant with all the complications of pregnancy. Did the island doctors fail to recognize beriberi or is toxemia of pregnancy merely a manifestation of thiamine deficiency? Our preconceived idea that each disease is a separate entity with a separate cause and an individualized treatment may very well be completely wrong. If energy metabolism is compromised, the dysfunctional effects will be related to the cells most affected. The symptoms and physical or mental deterioration will be as variable as the distribution of the energy deficit.
There is a lot more to this and I can only suggest that anybody wishing to be pregnant should obtain this book by John B Irwin M.D. “The Natural Way to a Trouble-Free Pregnancy” with the subtitle “The Toxemia-Thiamine Connection”.
It is, of course, mandatory for you to undertake this with the permission and care of your OB/GYN physician if you are pregnant. However, do not expect that the physician will automatically accept the idea. You may have to show him/her the book. As I have said many times in posts on this website, the emerging truth concerning the application of vitamins in the treatment of disease and the preservation of health has not yet reached the collective psyche of the medical profession. It has been hard won by the few pioneers that have begun to practice what is now called Alternative Complementary Medicine. They use few drugs and the results that they get are real.
Of RDAs and Mega-doses
It is quite obvious that you might ask the question, why, if this is so important in the lives and well-being of millions, it is not an acceptable practice in modern medicine by the majority of physicians? The answer is because of the teaching of biochemistry in medical schools. We all have known for many years that thiamine is acquired from the diet. The recommended daily allowance (RDA) is 1 to 1.5 mg. This minute dose acts as what is called a cofactor to many enzymes. Without sufficient cofactor, the enzymes do not function properly. Thus, vitamin deficiency has long been regarded as a situation that requires simple replacement of the cofactor. Therefore, the only dose required is that recommended as the RDA and mega-doses are regarded as being completely useless.
Unfortunately, what has not sufficiently been considered is that an overload of simple carbohydrate empty calories overwhelms the ability of thiamine to process glucose derived from the food. Glucose is used by body cells as fuel and the energy supply that results from it must meet physical and mental demands for maintaining healthy life. The modern diet is grotesquely unnatural and, because of the overload of empty calories the enzymes that are starved of their cofactors, begin to deteriorate. In order to resuscitate them, the cofactors must be used in a pharmacological way to stimulate the respective enzymes back into a healthy state.
Pregnancy Energy Demands are Significant
Pregnancy requires energy for the development of the baby as well as the health of the mother so the demand is greater. Cells will use what is needed of the mega-dose for the resuscitation to take place and will discard the excess in urine. The beauty of this new way of thinking about treatment of disease is that it is non-toxic and harmless. We even know now that some of the diseases, previously thought to be entirely genetic in origin, respond to mega-doses of vitamins. This has opened up a brand-new science called epigenetics that studies the effect of lifestyle and nutrition on genes. Genes are no longer considered to be solely in charge of our health destiny. We each have a responsibility towards the preservation of the blueprint (inheritance) by what we eat and our lifestyles.