One Fateful Day – And a Journey into the Enigmatic World of Thyroid Related Problems Begins
I remember the day of March 19, 2010 very well. That was the last day I ever went jogging. That was the last day I could have hopped on my bike and ridden 50 miles if I wanted to. That was the last day I ate my favorite breakfast of a 3-egg omelet topped with cheese and veggies, with 3 pieces of whole wheat toast slathered in butter and jam, 3 pancakes on the side, and at least a quart of milk. That was the last day I worked in my profession, brought home a paycheck, and was self sufficient financially. It was the day before I started taking Ciprofloxacin, a fluoroquinolone (FQ) antibiotic, for a simple UTI. And it was the last day I was a normal person with a normal life.
By March 25, 2010 – six days later — I was completely bedridden with severe pain in what felt like every tendon in my body, along with peripheral and central neurological symptoms and other symptoms from the side effects of that drug. These adverse effects are collectively called “Fluoroquinolone Toxicity Syndrome” (FQT), or “floxed” for short. And although I didn’t realize it then, my physical, professional, financial, and personal life as I knew it was over. Within a few days and a few pills, I joined the ranks of the chronically disabled, those with “chronic invisible illnesses”, and “Romney’s 47%”. It’s five long years later, and I still struggle with the aftermath of taking those few pills. I regret every single day since then that I ever even considered a fluoroquinolone antibiotic for a simple UTI.
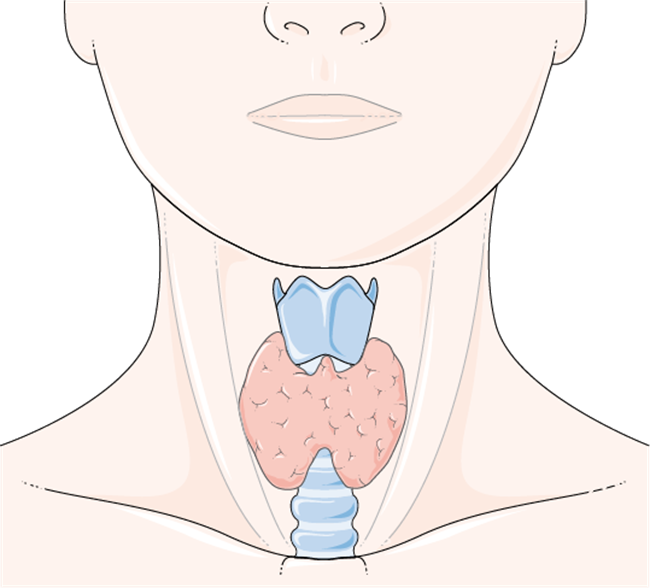
So what does all this have to do with the thyroid gland? Well, like most victims of this toxicity, all my extensive traditional medical testing during the acute phase of the reaction, as well as for the first year and a half after, gave normal or negative results. Astoundingly enough, despite being severely disabled and feeling essentially non-functional, according to the medical profession, I was the picture of health on paper. Until I finally decided to do more than a TSH test to check my thyroid status. That’s when I discovered I had all the anti-thyroid antibodies. And that’s really when my journey into the enigmatic world of “thyroid problems” began in earnest.
Having the antibodies for both Hashimoto’s Thyroid Disease and Grave’s Thyroid Disease makes for an astounding array of symptoms. Many of them appeared to mimic or overlap my symptoms of Fluoroquinolone Toxicity. Naturally, as a result of these observations, and my experiences with these conditions, I started questioning as to how much fluoroquinolone antibiotics caused severe endocrine disruptions, in particular of the thyroid axis.
The Thyroid Fluoroquinolone Epidemic: Where Is the Research?
There is a lot of published research available showing how damaging the FQ’s are too many different body systems and cellular processes, but almost none of it includes the thyroid system or the endocrine system in general. I suspect that someday, studies will be published showing the association between fluoroquinolones and thyroid abnormalities. Until then, it will be up to patients themselves to try and figure out if this association exists for themselves. In my case, my suspicions were further strengthened when I found that thyroid hormone medications, both T4 and T3, dramatically and profoundly affected all my floxing symptoms. Even more interesting to me, iodine alone did the same. I also found it interesting that a significant number of flox victims reported hormonal disruptions of all types post flox, such as with sex hormones, adrenal hormones, thyroid hormones, dysglycemias presumably in association with insulin hormone, and Vitamin D, which is also considered a hormone. This was also true of me after I was floxed. Eventually, I created a website* summarizing my observations, experiences, interpretations, and hypotheses on these possible correlations.
I had several intentions in creating the website, and one of them is to start the conversation about this potential link between fluoroquinolones and thyroid related problems, hopefully leading to unbiased studies and research in this area. I believe it is sorely needed. According to the U.S. Preventive Services Task Force Clinical Guidelines:
“The annual number of dispensed prescriptions of levothyroxine sodium in the United States increased by 42% over a 5-year period, from 50 million in 2006 to 71 million in 2010. In 2013, there were more than 23 million new prescriptions and refills for a single name brand of thyroid hormone in the United States, making it the most commonly prescribed drug in the country.”
This implies there are a lot of “thyroid problems” out there. According to several news investigations airing across the country, the FQ antibiotics are one of the top five drugs prescribed in the US each year. In our current day and age, we are bombarded by many substances which are known or suspected endocrine disrupters, including affecting the thyroid system. Could the epidemic of FQ usage be contributing to the epidemic of thyroid-related problems resulting in patients receiving thyroid medication for life? It would not surprise me if this were the case. I hope association studies, along with causation studies, will be done someday. Until then, those of us with thyroid disorders are on our own in looking at FQ antibiotic usage history and questioning this association for ourselves.
In my case, it was pretty clear cut that the acute symptoms I experienced right after starting the antibiotic were actually caused, or at a minimum, triggered by the antibiotic. My flox symptoms were pretty classic for these reactions all around, and there is plenty of research, as well as anecdotal stories, to substantiate this. But were my symptoms also “thyroid related”? In other words, did the antibiotic affect my thyroid system, either primarily and directly, or secondarily through a “cascade effect”, and at least some of these floxing symptoms I experienced were actually “thyrotoxic” symptoms as well? I think the answer is yes. These are the issues that I explore in my website, and I will briefly present here.
Tendon Pain and Ruptures: A Link between FQ Antibiotics and Endocrine Disorders?
One of the most well known adverse effects of FQ antibiotics are tendon problems. Most flox victims will experience some level of tendon pain at some point in time during their flox reaction. Regardless of what other symptoms occur with FQT, the severe tendon pain that can occur, sometimes with resultant ruptures, is distinctive, idiosyncratic, and unique to FQ antibiotic use alone. It is a hallmark of FQT. So much so, that an FDA “Black Box Warning” about it exists for all fluoroquinolone antibiotics.
It turns out there just aren’t a whole lot of things in life, either natural or synthetic, that can cause sudden spontaneous tendon ruptures or severe tendon pain and tendinopathies –but all of the endocrine disorders can. This includes: hyperadrenocorticism (cortisol), diabetes (insulin), parathyroid disorders (calcium/PTH/Vitamin D), hyper and hypothyroidism (tyrosine/iodine/thyroid hormone), hyper/hypo sex hormones (estrogens/testosterone), and probably other steroid and sex hormones and their metabolites as well (see references). A specific genetic metabolism disorder of tyrosine, which is a major component of thyroid hormones, can also cause spontaneous tendon rupture later in life as a first manifestation of this disorder. Many rheumatic diseases also often have an associated, if not underlying, endocrine component (especially thyroid related). Additionally, conditions that at first glance appear to be unrelated, such as chronic renal failure, often have a high association with endocrinopathies, in particular, parathyroid hormone abnormalities. The parathyroid glands are intimately associated with the thyroid gland via proximity alone; if thyroid gland architecture is destroyed, presumably these glands could be affected too.
I took a fluoroquinolone antibiotic and developed severe, systemic tendon pain, Type 2 Diabetes, and two Autoimmune Thyroid Disorders. A legitimate question could be: Are fluoroquinolone antibiotics severe endocrine disrupters, which, among other symptoms, can result in tendon pain, tendinopathies, and tendon rupture?
I then found that the thyroid hormone medications T4 and T3, as well as iodine alone, profoundly affected my tendon pain and other symptoms, capable of making these symptoms dramatically better — or much worse. This, too, seemed to support the argument that the fluoroquinolones had somehow damaged my thyroid system, as supplying exogenous hormone in the form of medication now could make such dramatic differences in my symptoms.
One of my hypotheses is that people with healthy and normally functioning thyroid glands or other endocrine systems can probably withstand these dramatic changes in the hormonal axes that may be occurring while on the FQ – at least, up to a point. For people who don’t react at all to these drugs, they probably never even feel the fluctuations, as their hormonal axes can automatically adjust rapidly. But I would suspect that anyone with any underlying genetic predisposition, or possibly harboring a subclinical, latent, or silent endocrinopathy might be “pushed over the edge” into full blown clinical pathology. This is actually what I think may have happened with me, even though I had no overt indications of any kind of thyroid or endocrine disorder prior to taking the Cipro.
Additional Links To Consider Relating Fluoroquinolones to Thyroid System Damage
I don’t profess to even begin to know the millions of ways fluoroquinolones could possibly exert their damaging effects on the thyroid or endocrine system in general. However, that didn’t stop me from thinking about this problem. As I said, I hope research studies will be initiated in this area sooner than later. In the meantime, I came up with several mechanisms of FQ-Induced Thyroid Pathology to consider as possibilities, to narrow down the search. Additional unintentional targets of fluoroquinolones that I considered could have thyroid-related repercussions included targets such as mitochondria, acetylcholine, steroid receptors and hormone response elements and their common pathways, selenium dependent enzymes and proteins, halogenated peroxidase enzymes, iodine receptors located on most or all cells as well as on the thyroid gland, and more. I think one of the more interesting observations is the fact that new fluoroquinolone derivatives are now being considered for use as “tyrosine kinase inhibitors” (TKI’s). TKI’s are relatively recent chemotherapy drugs developed to fight cancer – and one of their adverse effects appears to affect the thyroid system with some rather alarmingly high statistics. From my perspective, there appeared to be striking similarities between thyroid abnormalities occurring with TKI’s and the thyroid abnormalities I suspect may occur with the FQ’s.
Fluoroquinolone Antibiotics: Consider the Risks
Thyroid disorders, especially autoimmune based ones, are no joke. Autoimmune Thyroid Disorders are not simply disorders of the thyroid gland; in my opinion, they are systemic disorders, affecting many or all of the cells and tissues in the body, which is why there can be such widespread and potentially devastating symptoms. There are numerous environmental stressors that contribute to thyroid disease and endocrine disease, and the fluoroquinolone antibiotics may be one of them. Fluoroquinolones exert many damaging effects, and if they are damaging the thyroid axis directly or indirectly via a cascade effect, actually causing anti-thyroid antibody production, or even if they are triggering or unmasking a subclinical or silent condition in susceptible patients to an active pathological condition, this is of serious concern – or it should be. A “silent” condition means just that – you don’t know you have that predisposition. I can say from my own experience that taking a fluoroquinolone antibiotic is a hell of a way to find out. It is Pharma’s responsibility to provide adequate warnings and risks of this possibility, and the medical profession’s responsibility to make sure adequate testing rules out these antibodies along with other potential risk factors, before prescribing a fluoroquinolone antibiotic. Sadly, neither of these things is happening right now. Until it does, I think anyone considering taking a fluoroquinolone antibiotic for a simple infection, such as uncomplicated UTI or sinusitis, should be aware of the risk factors and possible alternatives.
Based on what I’ve learned in the past several years, I believe anyone with pre-existing endocrinopathies of any type (whether they’re known or not), to be at increased risk for these adverse reactions. I also believe that anyone who has experienced any kind of flox reaction has now gotten a warning sign, and is at increased risk of developing an overt or clinical endocrinopathy as a result of being floxed at any time after. One of the few supportive pieces of evidence for this hypothesis is buried in Table 3, Page 136 of a Mayo clinic paper here. Note the at risk population includes people with autoimmune or endocrine disorders (diabetes, thyroid, parathyroid) and steroid usage (ie, Prednisone, inhalers, anabolic steroids, etc.).
The best approach, of course, is to stay away from these drugs altogether if at all possible. In my opinion based on my own experience, developing a lifelong severe thyroid disorder – or any other disorder — to solve a short term problem such as an uncomplicated infection with a fluoroquinolone antibiotic, isn’t worth the risk.
References and Resources
- Musculoskeletal Complications of Fluoroquinolones: Guidelines and Precautions for Usage in the Athletic Population
- The Risk of Fluoroquinolone-Induced Tendinopathy and Tendon Rupture: What Does The Clinician Need to Know?
- Spontaneous rupture of Achilles tendon: missed presentation of Cushing’s syndrome.
- Spontaneous rupture of Achilles tendon and Cushing’s disease. Case report.
- Incidence and predictors of hospitalization for tendon rupture in type 2 diabetes: the Fremantle diabetes study.
- Musculoskeletal Complications of Diabetes
- Biomechanical Properties of Achilles Tendon in Diabetic vs. Non-diabetic Patients.
- Spontaneous and serial rupture of both Achilles tendons associated with secondary hyperparathyroidism in a patient receiving long-term hemodialysis.
- Simultaneous chronic rupture of quadriceps tendon and contra-lateral patellar tendon in a patient affected by tertiary hyperparatiroidism.
- The level of vitamin D in the serum correlates with fatty degeneration of the muscles of the rotator cuff.
- Parathyroid disease.
- Primary hyperparathyroidism due to atypical parathyroid adenoma presenting with peroneus brevis tendon rupture.
- Thyroid hormones and tendon: current views and future perspectives. Concise review.
- Thyroid hormones increase collagen I and cartilage oligomeric matrix protein (COMP) expression in vitro human tenocytes.
- Suspected role of ofloxacin in a case of arthalgia, myalgia, and multiple tendinopathy. (Inhaled steroids and moderate hypothyroidism precipitating factors).
- Could Low Total and Free Testosterone Levels be risk factor for Achilles Tendon Ruptures in Males.
- Pathological rupture of the distal biceps tendon after long-term androgen substitution.
- Effect of estrogen on tendon collagen synthesis, tendon structural characteristics, and biomechanical properties in postmenopausal women.
- Female Athletes with Higher Estrogen Levels May Have Higher Injury Risk.
- Effect of administration of oral contraceptives in vivo on collagen synthesis in tendon and muscle connective tissue in young women.
- Successive ruptures of patellar and Achilles tendons. Anabolic steroids in competitive sports.
- Spontaneous rupture of the anterior cruciate ligament after anabolic steroids.
- Spontaneous rupture of the extensor pollicis longus tendon after anabolic steroids.
- Spontaneous tendon ruptures in alkaptonuria.
- Rheumatic manifestations of endocrine disease.
- The endocrine system and connective tissue disorders.
- Same Disease, Different Symptoms: It’s all in the Mitochondria.
- Your Mighty Mitochondria.
- Department of Health and Human Services Public Health Service Food and Drug Administration Center for Drug Evaluation and Research Office of Surveillance and Epidemiology Pharmacovigilance Review. (References provided for mitochondrial toxicity within the document).
Share Your Story
If you have been injured by a fluoroquinolone antibiotic, please share your story. Send us a note here, for more information.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Laboratoires Servier, CC BY-SA 3.0, via Wikimedia Commons
*The website is no longer available.
This post was published originally on Hormones Matter on May 7, 2015; links have been updated where appropriate.