Two of the most commonly asked questions I face as someone with Lyme disease is “when were you bitten by a tick?” and “when did you get Lyme?” To be honest, while I have my suspicions, I really have no idea. Many people are surprised to hear that the majority of people with Lyme disease never recall being bitten by a tick. The bullseye type rash that people assume is the hallmark of Lyme symptoms also doesn’t occur in many of us with Lyme, hence why we have no idea when we first contracted the disease.
Early History
I was an active child and a competitive swimmer. By high school, I was swimming at the state and national level. I was in great shape with great health, or so I thought, and had no obvious reason to be experiencing any medical abnormalities. However, over my freshman year in high school, I started experiencing widespread joint pain. Because I was in such good health and swimming and training up to four hours per day, it came as a surprise to my parents, coaches, and doctors when I was experiencing such pain. During this time, I did get tested for Lyme by my pediatrician. While he was fine testing for rheumatoid arthritis and lupus, we had to beg him to test for a Lyme test, even though it was common in our area. It was years later when we learned that traditional doctors typically do not test for or treat Lyme disease.
My test showed that I had one positive band of Lyme. He said that this was not enough for a diagnosis, and I was sent home without any answers. My sophomore year of high school, the joint pain continued and even began to get a bit worse. I went to a rheumatologist at the Children’s Hospital of Philadelphia and was diagnosed with Amplified Musculoskeletal Pain Syndrome, also known as AMPS. Their main treatment plan was exercise, which, with swimming, I was already doing. There wasn’t much else that could be done, but by junior year it seemed like I had grown out of AMPS. Whether it was really AMPS or had it been Lyme disease all along, I have no idea.
College Dorm Flu Masked My Infections – Until My Vocal Cords Went Haywire
My freshman year of college living in a dorm I was sick constantly. I missed several of my college swim meets from contracting the adenovirus, developing severe swimmer’s ear, and coming down with strep throat and bronchitis. Another strange thing I began to notice was that I was having low grade fevers nearly every day. I got tested for the mono virus, as many college students are, at one point or another, but the test came back negative. With the constant infections, along with many headaches and slight fatigue, a blood test showed that I had an underlying Epstein Barr virus from prior contraction. I do think they missed mono, and I can’t help but wonder if Lyme played a role.
During my sophomore year of college, I began the swimming season feeling strong until I developed a nasty virus along with a bad cough within the first few weeks of the semester. Luckily, the virus died down, however the cough never went away. The cough became worse as I swam and I was led to assume I had developed sports-induced asthma. I just couldn’t get in a good full breath. During fall break, I went to an allergy and asthma specialist. When I told her I couldn’t fully breathe in, she pointed out that with asthma, you typically have trouble breathing out. She performed a rhinoscopy, where they stick a camera in your nose down into your throat, and examined my vocal cords on a very fuzzy screen before diagnosing me with vocal cord dysfunction. This was a difficult diagnosis because it was hard to explain to friends and family. It is not commonly known, and somewhat misunderstood. People genuinely had no idea that when I was breathing in, my vocal cords were spasming closed. The only thing I could link this to was the virus I had a month prior.
It took months of my vocal cord dysfunction being taken lightly or just blatantly disbelieved until I went to an otolaryngology specialist in New York City. The specialist performed a rhinoscopy as well, but recorded everything on a crystal clear screen. He was able to visibly show my parents that my vocal cords were, in fact, spasming closed when I breathed in. My parents have since admitted they didn’t fully believe me until that appointment. The recommended treatment was Botox. This meant that I had to go into the city every few months to get Botox injected into my vocal cords. Eventually, the doctor recommended surgery because folds of tissue were leaning into my airway over my vocal cords, a condition known as laryngomalacia, making my vocal cord dysfunction worse. I got surgery and continued with my Botox appointments and my vocal cord dysfunction finally calmed down a bit. Again, here I had suspicions that this was related to Lyme disease as well. My first Lyme specialist commented that vocal cord dysfunction could have been a result of the disease. After hearing Shania Twain’s story about how Lyme disease affected her vocal cords, my suspicions were stronger, but, again, I will never know for sure.
Looking For a Zebra: Fatigue, Tachycardia, and Hypertension
I took a year off of school for a few different reasons, some of them being medical. I was still experiencing low grade fevers constantly, fatigue, tachycardia, and hypertension. I was still very active, going to OrangeTheory Fitness classes a few times a week, along with lifting weights and swimming. Currently, I can barely walk my dog and my exercise consists of physical therapy. A few times, I went to OrangeTheory Fitness with my mom, and when I looked up at my name on the screen, I saw the number 212, which I thought was my score (I thought I was winning), but my mom realized it was actually my heart rate. At another point during this year, my blood pressure was in the 200s over the 200s. I went to an endocrinologist for my fevers, fatigue, and the general feeling that something was very off. She told me I was on so many psychiatric medications that they were making me “sound slow,” and that I just had fever of unknown origin. She also said that she was going to visit her family in India and could bring me back herbal supplements for the fever of unknown origin.
That being said, I did have severe anxiety at the time and was dealing with post-traumatic stress disorder. I had no idea what this meant at the time, but my psychiatrist told me to go to my primary care doctor and tell him “we’re looking for a zebra,” and even a pheochromocytoma. I saw several doctors that year, each who ordered different types of blood work. One doctor was so unsure what was happening that she ordered twenty two vials of blood. Yet, I was still left without any answers.
And Then Came Covid
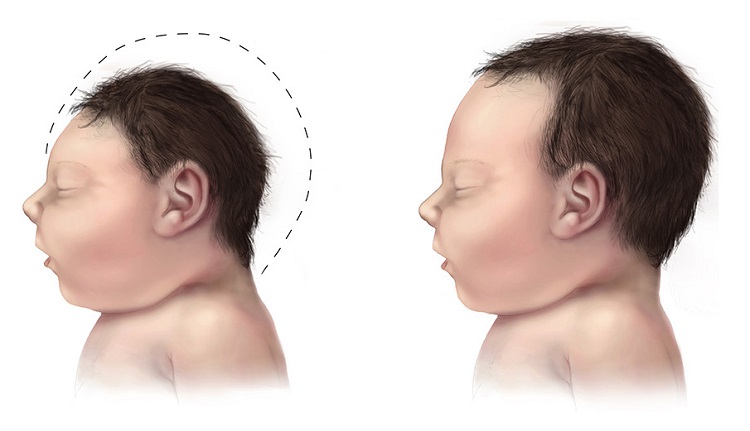
After my mental health and anxiety had not improved with medication and therapy, my mom felt there still had to be an underlying issue. This is when she found and took me to a Lyme specialist in the fall of 2019, who immediately diagnosed me with Lyme disease and bartonella, and later, mast cell activation syndrome (MCAS). Physically, my symptoms were manageable. However, I contracted the first strain of COVID-19 in May of 2020, and my life has never been the same. Within the next few months, I started experiencing joint pain, severe migraines, vertigo, severe fatigue, and continued mental health issues. I even had to drop all of my classes in the fall semester of 2020 because I missed nearly two weeks of school from having a fourteen day long migraine. I began developing neurological and cognitive issues, such as trouble focusing and thinking and I had with memory. I switched to a different Lyme specialist, and this time I even tested CDC positive, which is more uncommon than not in those with Lyme. I started yet again another regimen of antibiotics and herbs. I spent most of that year couch ridden, sleeping much of the day, and constantly in hot Epsom salt baths to ease the joint and muscle pain. It felt like my mind and body were completely outside of my control, almost like my autonomy was taken from me. I was on several combinations of antibiotics until I eventually switched doctors again. This new physician was recommended by my Lyme literate dietitian, and was extremely knowledgeable of complex cases. I still see her to this day.
The next year I went back to school part time, only taking two classes each semester. Before the fall semester, I was diagnosed with babesia, and a few months into the semester I was diagnosed with hypothyroidism. These diagnoses often come together in the case of Lyme disease, but a new diagnosis is always a lot to take in. In class, I would forget what I was saying mid-sentence, which made me self-conscious and hesitant to participate. I struggled to balance the fatigue, physical pain, and brain fog with school. Yet, I successfully completed those two semesters.
Medication-Induced Pancreatitis
Finally, my senior year began: Fall of 2022. I was still attending part-time, but was now taking three classes as well as a lab each semester. In late September, early October I started having these acute episodes of severe pain in my upper abdomen that spread to my back. Because I have been medically gaslit so many times and I also have a high pain tolerance, I was nervous to go to the doctor. These episodes felt like I should have been in the emergency room, but because they only lasted an hour I was afraid to go to the hospital in fear that they would brush me off as a young female having stomach aches. I dealt with the pain for almost four weeks before I finally went to a doctor.
As it turns out, I had pancreatitis. I had to go on a mostly liquid diet for two weeks, stop taking my antibiotics and other supplements for Lyme, as doctors believed it was drug induced, with the culprit suspected to be rifampin, or the combination of too many other medications and supplements. I had been on various psych meds for years. Initially they were prescribed for severe anxiety and panic attacks and when I began to get sick, it only worsened. Among the medications I have been prescribed and used are several SSRIs/SNRIs (Prozac, Zoloft, Lexapro, Luvox, and Effexor). I have used sleeping medications such as Prazosin, Seroquel, and trazodone, as well as a tricyclic antidepressant, some benzodiazepines, Wellbutrin, Buspar, hydroxyzine, and different ADHD medications (Concerta, Ritalin, Vyvanse, Adderall, Straterra).
While pancreatitis mostly resolved, my Lyme started to continue to progress. I was having many more neurological and cognitive symptoms, my whole body was tremoring nearly every day, and I knew that we had to take action before the Lyme and coinfections progressed any further. I went back on antibiotics at the beginning of the spring semester, but had many Herxheimer reactions. I was out of it and sweating with fevers in class, all while also managing an internship. Within a few months my tremors became much better, indicating that the antibiotics were working. It was a long and stressful year, but I graduated Magna Cum Laude after having periods of extreme sickness where I questioned whether I would ever graduate.
Right now I’m on Anafranil, Buspar, Trazodone, Hydroxyzine, and Valium. As for Lyme and coinfections, I’m on clarithromycin, Tinidaloze, Valtrex, Mepron, methylene blue, (recently started), low dose Naltrexone, liposomal oil of cinnamon clove and oregano, cryptolepis, Researched Nutritionals MycP, phosphatidylcholine, vit D and C, omegas, ATP360 and CoQ10 for mitochondrial dysfunction (my doctor has suspected mitochondrial death/dysfunction after having COVID the first time, followed by long covid). I’m on a whole bunch of other supplements too to support my immune system, help with mast cell activation/histamines, digestion, brain function, etc. I’m taking between 50-70 pills per day with a few liquids mixed in there. I’m also on thyroid Armour for hypothyroidism as well as migraine medications and Zofran.
Chronic Illness Limbo: Neither Disabled Nor Able Bodied
Something that healthy people may not think about is having to choose your battles in terms of symptoms and treatments. For example, I started methylene blue shortly after graduation. Methylene blue, which is a medical dye, is a relatively newer, yet promising treatment for Lyme disease, but it is a monoamine oxidase inhibitor (MAOI). This means it can interact with psychiatric medications, and, therefore, I had to go off of all of my ADHD medications. The combination of an MAOI and a serotonergic ADHD medication can lead to both serotonin syndrome and a hypertensive crisis. The idea is that over time and with building up the dosage of the methylene blue it will minimize brain fog, a huge Lyme symptom, and help to treat ADHD symptoms. However, it takes quite a while to build up to an adequate dosage of methylene blue, and it also takes some time for it to actually show effects and improvements. Methylene blue treatment has been a bit brutal here and there with Herxheimer reactions.
One of the most daunting and frustrating things about Lyme disease, especially when it becomes chronic, is that there is rarely a trajectory or expected timeline to start feeling better or to reach remission. I’m currently still trying to find my way to remission, but cannot say I am close. Lyme Disease has turned my life upside down. At this point in my life, I thought I would be living up my twenties with either having already started graduate school or a big girl job. Something that people with Lyme disease, and those with other chronic illnesses as well, deal with on a regular basis is not being able to keep up with productivity culture leading to feelings of failure, laziness, or character flaws. Chronic illness is isolating, and, for many, it may feel like there is no place in society for us when we’re neither fully able bodied nor fully disabled. Instead of living up my twenties, I spend most days with my parents and my dog, I rarely drink alcohol or go out with friends, as it is difficult to maintain friendships when chronically ill. I am still trying to find a place to fit into society post bachelor’s degree, without a master’s or doctoral degree. I feel resentful of all of the doctors who misdiagnosed me or gaslit me, letting me go longer and longer undiagnosed, and therefore, untreated, allowing the Lyme to progress. However, I have found friends in the chronic illness community that, even though we have a variety of illnesses and different symptoms, understand the common struggles of chronic illness.
If you suspect you have Lyme, the best thing you can do is go to a Lyme literate doctor in your area, whose names and locations are usually spread through word of mouth due to the politicization of Lyme Disease, which can lead to possible repercussions for doctors who treat Lyme without CDC positive tests, which, like I said earlier, are inaccurate and are not often used as a basis for diagnosis.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, and like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.