In a number of posts on this website I have mentioned the technical term “oxidative metabolism” in relationship to thiamine. I have tried to explain it by analogy, using the consumption of gasoline in a car. Gasoline is mixed with oxygen and ignited by a spark. In the human body glucose is the equivalent of gasoline and thiamine is the equivalent of the spark. This case tells us that thiamine has other effects of equal importance.
Many years ago, I learned of a naturally occurring derivative of thiamine that had been discovered in garlic. It had a more powerful clinical action than the original thiamine from which it had been derived. The Japanese investigators who discovered it had done many experiments with both animal studies and human subjects, with some remarkable results. For example, they had found that mice could be partially protected from cyanide poisoning by treating them with this derivative before the cyanide was given. It had been synthesized and is used in Japan as a prescription item (Alinamin) in many different diseases. I became intrigued by its potential and since it was totally unrecognized in the United States, I applied to the FDA for an Independent Investigator License (IND) that was granted to me in 1973. Because it has a long and complicated chemical name I shall call it TTFD. I used it in treating many patients, usually with great benefit and never saw the slightest sign of toxicity.
Reye’s Syndrome, the Flu, and Thiamine
In order to introduce its potential, I am going to describe the case of an 18-month-old girl who was admitted to our hospital with Reye’s syndrome. Some people reading this will remember that this disease kept cropping up in association with epidemics of “flu”. Many of the children died and although it has now been discovered that it was due to aspirin given to the child to bring down the fever, at the time that I treated this case, this fact was not known.
The infant was admitted to the hospital in a coma which had begun 48 hours previously with repeated vomiting. The initial treatment was given by neurologists, using exchange blood transfusion and as in other cases, was a complete failure. The coma deepened rapidly. Pupils became fixed and dilated and she was judged to be in a terminal state. The respirator that had been used to keep her alive was withdrawn. One week after her admission there was no change in her condition. She was deeply comatose and all treatment other than normal life support was withdrawn. In short, her case was considered to be hopeless.
High Dose Thiamine (TTFD) for Reye’s Syndrome?
Because from that point on the treatment was to be experimental, I obtained full consent from the parents. I gave 100 mg of TTFD by nasogastric tube every four hours and 150 mg by intravenous injection, a total of 750 mg in 24 hours. This was repeated daily. When you consider that the daily intake of thiamine under normal healthy circumstances is 1 to 1.5 mg a day, this was truly a humungous dose. Please understand that this is not vitamin replacement. It is clearly the use of a vitamin as a drug.
The first thing that happened was the lip vermilion became bright red, whereas it had previously been dusky, the color of deoxygenated blood. There was healthy flushing of the cheeks. Two days later there was some spontaneous movement of the limbs, her pupils responded to light and she developed a cough reflex. After one week the daily dose of intravenous TTFD was discontinued and the oral dose decreased to 300 mg a day. After nine days from the beginning of this treatment TTFD was decreased to 150 mg a day.
On the 15th day, eye contact could be established and she responded to sounds but was still unconscious, a state known as coma vigilum. Subsequently she began to take Jell-O from a spoon and began to show primitive crying responses. By the 21st day she was able to chew and could support her own weight with help. She began to walk with her hand held and self feeding began. Speech returned and gradually improved. She was discharged from hospital one month after this treatment had been started. The TTFD was continued at the same dose and three months later she was clinically well, although muscular tone was diminished. Not surprisingly, as she grew there was evidence of some permanent damage.
Thiamine, the Mitochondria and Oxygen
We now have reason to believe that Reye’s syndrome is mitochondrial in nature. Mitochondria are organelles within our cells that generate energy from oxidative metabolism. In this disease the mitochondria are affected in that part of the brain that maintains life. The return of lip vermilion and flushed cheeks was the first indication that oxygen was being picked up by the blood in the child’s lungs and conveyed to the tissues. The return of function in the brain indicated that oxidative metabolism had been restored. Hemoglobin is a protein that coats our red cells and combines with oxygen in the lungs to become what is called oxyhemoglobin. It is bright red in color and that is why oxygenated arterial blood is bright red. When arterial blood gets to the tissues, it delivers the oxygen to the cells and the hemoglobin loses its red color, becoming bluish, the color of venous blood and the color of hemoglobin after it has delivered the oxygen. The first indication of this transformation was the change in the color of the lips and the appearance of flushed cheeks.
Thiamine, Oxidative Metabolism and Reye’s Syndrome
The administration of TTFD to this child had resulted in the formation of oxyhemoglobin, enabling the delivery of oxygen to the brain. Because function increased we also have to assume that the oxygen was unloaded to the cells that needed the oxygen. It also explains why the low concentrations of oxygen in arterial blood and high concentrations in venous blood were recognized by early investigators in beriberi. This is important new information because it indicates that thiamine has some effect on the ability of hemoglobin to pick up oxygen and even deliver it.
In 2004, Japanese scientists showed that the injection of a compound similar to TTFD could actually increase the concentration of oxyhemoglobin. This ability has never been recognized for the chemical functions of thiamine and TTFD has an action that is identical to that of thiamine. It forces us to wonder whether TTFD might be a benefit to those people with bluish lips and poor color attributed to heart disease and other situations labeled with the term cyanosis (deoxygenated blood). Using it at the time of hospital admission would probably have prevented permanent damage.
Reference
- Ishimaru T, et al. Hemodynamic response of the frontal cortex elicited by intravenous thiamine propyl disulfide administration. Chem. senses 2004;29(3):247-51.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
This post was published originally on Hormones Matter on March 16, 2016.
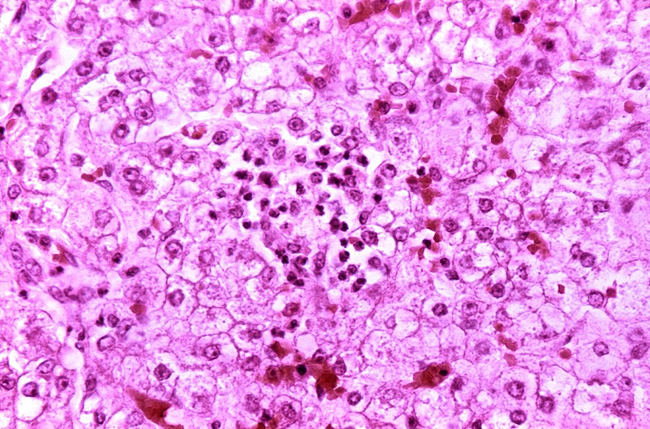
Photo: Histopathology of Reye’s syndrome, liver Histopathology of autopsy liver from child who died of Reye’s syndrome. Hepatocytes are pale-staining due to intracellular fat droplets via Wikipedia and the Centers for Disease Control and Prevention‘s Public Health Image Library.