Modern lifestyles are countering nature’s intentions to keep us healthy. Since the advent of the Industrial Revolution in the late 18th century, we have migrated from farms to factories and office buildings. Nature intended for us to live and work outdoors in the sun—without sunscreen. Today most of us live and work indoors—often wearing sunscreen, or cosmetics containing sunscreen. By doing so, we have denied our bodies one of the most fundamental sources of health: the ultraviolet B (UVB) rays of the sun that initiate vitamin D protection in our skin.
Compelling scientific evidence over the past century indicates the significant role vitamin D plays in protecting us from developing a wide variety of medical conditions including autism, autoimmune disorders, cancer, cardiovascular disease, diabetes, and thyroid disorders. It is not a coincidence that the prevalence of these diseases has emerged during “modern” times. These medical conditions, many of which are serious, chronic, and life-threatening, frequently result in health, financial, and social burdens to the patients and their families.
What is Multiple Sclerosis?
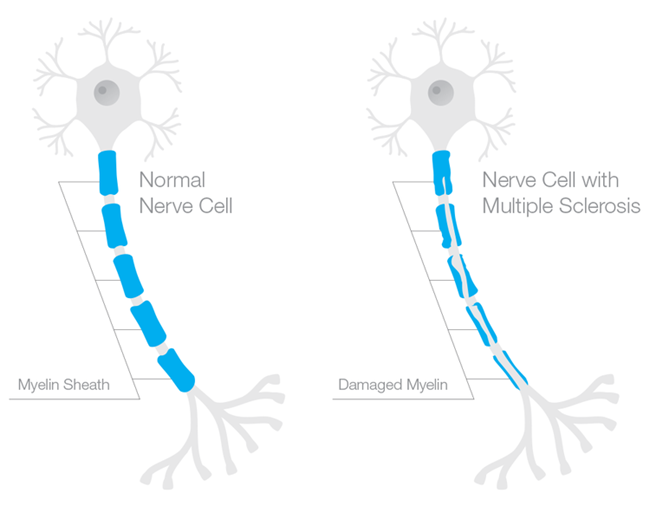
Multiple sclerosis (MS) befits a disease of modern civilization. First identified by French neurologist Jean-Martin Charcot in 1868, MS is a chronic, neurological autoimmune disorder that damages the myelin sheath, the multiple layers of fatty tissue that surround and protect the nerves in the brain, spinal cord, and optic nerves. When the myelin sheath is intact, electrical impulses are carried through the nerves with accuracy and speed. When the myelin sheath is damaged (sclerosis is the scar tissue formed by damaged myelin), the nerves do not conduct electrical impulses normally. The impulses are distorted or interrupted, resulting in a range of symptoms including numbness, blindness, paralysis, and brain damage. MS also can result in death.
Who is at Risk of Developing MS?
Despite the identification of MS almost 150 years ago, MS has no cure. Over 2.5 million people around the world have been diagnosed with MS including about 400,000 Americans. Women are to two to three times more likely to develop MS than men. Although MS is usually diagnosed between the ages of 20 and 50, the disease can strike at any age. In addition, Caucasian women of Northern European descent are more frequently diagnosed with MS than African Americans, Hispanics, and Asians.
As part of the Environmental Risk Factors in MS Study (EnvIMS), researchers at the University of Bergen in Norway sought to understand better the association between MS and sun exposure measures by studying a total of 1,660 MS patients and 3,050 controls from Norway and Italy. The researchers’ findings included significant connections between infrequent summer outdoor activity and sunscreen use and an increased risk of MS. Published in the January 10, 2014 issue of Multiple Sclerosis, the study’s conclusion stated, “Converging evidence from different measures underlines the beneficial effect of sun exposure on MS risk.”
It is not surprising that incidences of MS in the equatorial region occur much less frequently than at the higher latitudes. Epidemiological studies over the past several decades however indicate that women who live at higher latitudes have an increased risk of developing MS. For example, University of Oxford researchers studied MS patterns in Scotland by examining hospital admissions throughout the country between 1997 and 2009. The research team discovered a “highly significant relationship between MS-patient-linked admissions and latitude” across Scotland. This study was published in a 2011 issue of the Public Library of Science (PLoS) One journal.
In addition, a seasonal risk factor also exists for MS. Researchers at Queen Mary University of London conducted a systematic review of data for 151,978 MS patients to ascertain the link between month and location of birth, and the risk of developing MS. They found that babies born in April had the highest risk of development of MS, and infants born in October enjoyed the lowest risk of MS. The researchers also noted a direct correlation between the latitudinal location of expectant mothers and MS risk. The study, published in a 2012 issue of the Journal of Neurology, Neurosurgery, and Psychiatry, suggests the importance of maternal vitamin D supplementation in particular during the winter season.
What Causes MS?
The definitive cause of MS remains unknown but medical research suggests genetic and environmental factors influence one’s risk of developing MS. Interestingly enough, science has demonstrated that vitamin D plays a role in influencing environmental and genetic factors that may affect how likely one is to develop MS.
A landmark study at the University of Oxford, published in a 2009 issue of Public Library of Science (PLoS) Genetics, examined how genes and the environment interact in MS. A gene variant called HLA-DRB*1501 is associated with an increased risk of developing MS. The research team discovered how vitamin D influences the HLA-DRB*1501 gene variant. As we know, the amount of vitamin D synthesized by UVB sunlight exposure fluctuates from season to season. Therefore, women who give birth during the spring, carry the HLA-DRB*1501 gene variant, and have low vitamin D levels are more likely to produce children with a higher risk of developing MS.
The study’s author Dr. Sreeram Ramagopalan suggested that adequate vitamin D3 supplementation during pregnancies may decrease the risk of children developing MS in later life. The combination of carrying the HLA-DRB*1501 gene variant and lacking adequate vitamin D levels may impair the ability of the thymus, an immune system organ, to delete rogue T cells, a type of white blood cells, that play an important role in maximizing the immune cells. The rogue cells would attack the body, causing demyelination of the central nervous system.
How Can Vitamin D Protect Against MS?
MS is a neurological autoimmune disorder. Scientific research over the past few decades solidifies the connection between vitamin D and autoimmunity. Vitamin D plays an integral role in the regulation of the adaptive immune system.
Adequate vitamin D in our bodies can protect us from autoimmunity because adaptive immune cells contain vitamin D receptors (VDRs). These receptors are attached to the surface of the adaptive immune system’s antibodies and sensitized lymphocytes. When the VDRs receive adequate amounts of vitamin D, they enable the adaptive immune system to function properly by attacking new and previous invaders.
When the VDRs attached to the adaptive immune system’s cells do not contain sufficient vitamin D to attack invaders, autoimmunity may kick in, causing the death of healthy immune cells. Thus, vitamin D deficiency can contribute to the development of autoimmune disorders such as MS.
How Can Vitamin D Treat MS?
The scientific community is delivering hope to MS patients by investigating vitamin D intake as a treatment for the disease. Research suggests that higher vitamin D levels are associated with reduced disease activity in MS sufferers.
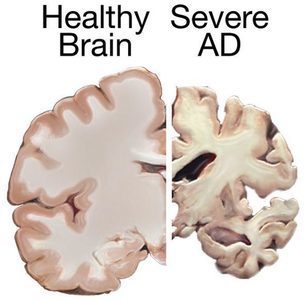
Dr. Alberto Ascherio of Harvard University’s School of Public Health and colleagues recently concluded that vitamin D appears to be connected with MS disease activity and progression in patients who experienced an initial episode suggestive of MS and were treated with interferon β-1b. The researchers found that 20 ng/mL-increases of vitamin D levels within the first 12 months of experiencing an initial episode predicted a 57 percent lower rate of new active lesions as well as a lower risk of relapse. In addition, the results included a 25 percent decrease in annual T2 brain lesion volume and a 0.41 percent lower yearly loss in brain volume over four years. The Harvard study was electronically published on January 20, 2014 in JAMA Neurology.
According to a study published in a 2012 issue of the Annals of Neurology, a University of California, San Francisco research team examined 469 male and female MS patients over five years to ascertain how vitamin D affected disease progression. The researchers discovered that for each increase of 10 ng/mL in vitamin D levels, the MS patients benefited from a corresponding 15 percent decrease in new brain lesions as well as a 32 percent lower risk in inflammation of the myelin sheath.
A Finnish study, published in a 2012 issue of the Journal of Neurology, Neurosurgery, and Psychiatry, concluded that vitamin D3 supplementation significantly reduced the number of brain lesions in MS patients undergoing interferon β-1b treatment.
Paving a Way to Better Health and Quality of Life
Adequate vitamin D levels in our body may indeed protect us from developing MS. If you have experienced a possible initial episode or have been diagnosed with MS, please consider how vitamin D3 supplementation may decrease the severity of your symptoms.
We must take ownership of our health by understanding the importance of vitamin D as well as other micronutrients. Why wait years, or decades, to garner the results of further studies and clinical trials to define the exact relationship between vitamin D status and MS. We can be proactive by taking daily vitamin D3 supplements and enjoying moderate sunlight exposure to increase our vitamin D levels.
It is imperative to take enough vitamin D so this essential nutrient will be stored in your cells to help regulate your immune system. The greater your vitamin D level (easily obtained from a simple blood test called 25(OH) vitamin D), the more likely you will benefit from a stronger immune system that will protect your body’s cells from attacking one another.
No one wants to endure the health, financial, and social burdens of a chronic debilitating disease. By empowering yourself with adequate vitamin D, you may not only reap lots of health benefits but enjoy a better quality of life.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
To Learn More
Image credit: Stephanie021299, CC BY-SA 4.0, via Wikimedia Commons
This post was published here originally on March 4, 2014.
Copyright © 2014 by Susan Rex Ryan. All rights reserved.