Whether a hysterectomy will affect sexual function is a common concern amongst women considering the surgery, as well it should be. Sex is a vital part of life and the loss of sexual function can be devastating. Whether and how hysterectomy affects sexual function is not very clear, however, and depends upon a number of variables, not the least of which is sexual function pre-hysterectomy, and particularly, pre-gynecologic problems. In many cases, women have a hysterectomy to rectify conditions associated with heavy bleeding and/or excessive pain like fibroids, endometriosis, adenomyosis and cysts. Reducing pain and bleeding should positively affect sexual frequency; however, effects on function may vary. Hysterectomy can diminish sexual function either directly because of the disconnection of the nerves and blood vessels that supply sexual energy or indirectly via the loss of critical hormones when or if the ovaries are removed or cease to function. And for many women, those with endometriosis, the hysterectomy itself provides only temporary relief from the disease process.
When evaluating the possibility of having a hysterectomy relative to sexual function outcomes, there are a few things women must consider.
Understanding the “Anatomy” of Sexual Function
According to Masters and Johnson, there are four phases of sexual response – Excitement, Plateau, Orgasm, and Resolution.
Sensation to any body part requires proper nerve conduction and adequate blood flow. Many nerves, blood vessels, and ligaments are severed to remove the uterus. The uterus and its ligaments themselves are rich sources of blood supply. As a result, sensation to the vagina, clitoris, labia, and nipples can be diminished by hysterectomy. This loss of sensation can hamper sexual function.
The Excitement phase is triggered by sexual stimuli, either physical or psychological. The stimuli triggers increased blood flow (vasocongestion) to the genitalia. With a blood vessel and nerve network altered by hysterectomy, this process may be hampered.
Contractions of the uterus are listed as a part of the Orgasm phase. So without a uterus, orgasm is not complete. Hence, it would make sense that orgasm is negatively impacted by hysterectomy, ovary removal or not. I have read, however, that some women do not experience uterine orgasm. So for them, a hysterectomy may not affect their orgasms.
My Personal Experience Post Hysterectomy
I realized very quickly after my hysterectomy that my libido, arousal, and ability to orgasm were broken. A steamy sex scene in a novel or movie or a hot looking guy no longer elicited sexual feelings. And the thought of sex was repulsive. That was a very sad day for me and I still mourn the loss of my intact sexuality. Some may question whether these changes are really due to the loss of my uterus or more so from the loss of my ovaries. When my hormone replacement was inadequate, the thought of sex was repulsive. However, I did have occasional orgasms but they were difficult to achieve and very infrequent as well as disappointing compared to before hysterectomy. Before my surgery, I had a good libido and an intense uterine orgasm every time I had intercourse. I have been on a good hormone regimen for over 6 years now. Sex is no longer repulsive but I do not have a libido or feel sexual in any way. Arousal takes much longer and orgasms are still weaker than before hysterectomy, do not always happen, and rarely occur during intercourse. Testosterone did not improve libido or arousal nor improve orgasm frequency or quality. Nipple sensation has been absent since surgery. These losses to my sexuality have affected my marriage relationship as well as social and professional relationships as I lack what I would call “sexual energy” and confidence.
Other Possible Sexual Sequelae Post Hysterectomy
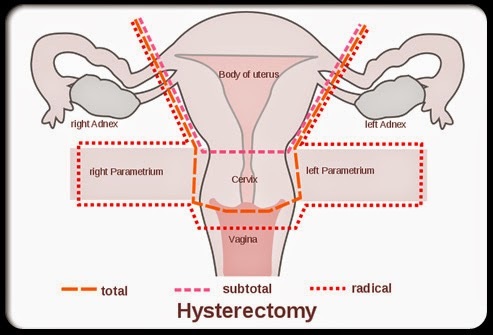
Removing the Cervix. The changes to the vagina after hysterectomy can further hamper sexual function. The removal of the cervix (the lower part of the uterus) requires that the vagina be shortened and sutured shut. This is called the vaginal cuff. The shortened vagina can present problems with deep penetration. Also, the vaginal cuff sutures can tear (dehiscence) which is a serious medical problem, although this is rare. Retaining the cervix eliminates these concerns and may preserve some of the nerves and sensation. During sex, the tip of the penis is “grabbed” by the cervix enhancing the man’s pleasure. However, even if the cervix is retained, this “grabbing” sensation may not occur without the uterine contractions.
Reduced Lubrication. Many women report diminished vaginal lubrication post-hysterectomy even when ovaries are not removed. Lubrication is critical for sexual activity as well as sensation. When the ovaries are removed or fail from the loss of blood flow, lubrication is lost and the vagina atrophies making sex painful. Over time, the vagina may prolapse as it no longer has the uterine ligaments to anchor it. Changes to bladder, bowel, and vagina position and function post-hysterectomy can likewise affect sexual function and satisfaction. A falling vagina and urgency and incontinence are certainly not sexy!
Body Changes. The hysterectomy induced changes to a woman’s figure which include a thick, shortened midsection and protruding belly are another source of sexual dysfunction and anxiety. Appearance changes from hormonal effects such as hair thinning, graying, and texture changes, skin dryness and aging (including loss of plumpness and pinkness in the genitalia), and loss of muscle mass and tone can also negatively impact sexuality. I have written about the anatomical and skeletal effects of hysterectomy here and here.
Emotional Changes. Many hysterectomized women with whom I have communicated report a loss of feeling connected to others including their loved ones. At first I thought the loss of my romantic and maternal feelings was solely attributed to the loss of my ovaries (despite taking estrogen). But after hearing from other women who still had functioning ovaries and reported the same feelings, I realized that maybe our uterus is what makes us loving and social beings. A renowned gynecologist on a talk show a few years after my hysterectomy referred to the uterus as “a woman’s heart center.” And for women love and sex are very much intertwined.
Hysterectomy and Sexual Function
Why is it that so many dismiss sexual problems post-hysterectomy as psychological? If a man has his prostate and/or testicles removed or penis shortened (heaven forbid!), sexual problems are attributed to the loss or surgical alteration of his SEX organ(s). So why would it be any different for women?
Although there have been some studies on sexual function after hysterectomy, I have not been able to make much sense out of them. It seems that most use a benchmark of (impaired) sexual function shortly before hysterectomy when gynecologic problems impede sexual activity and function versus prior to the gynecologic problems that are the reason for the hysterectomy. This observational study compared sexual pleasure, activity, and problems by type of hysterectomy at 6 months post-operative. It concluded that “sexual pleasure significantly improved in all patients, independent of the type of hysterectomy.” However, it also concluded that “the prevalence of one or more bothersome sexual problems six months after vaginal hysterectomy, subtotal abdominal hysterectomy, and total abdominal hysterectomy was 43% (38/89), 41% (31/76), and 39% (57/145), respectively.” With these high rates of “bothersome sexual problems” I cannot imagine how this could have been an improvement. However, if the benchmark was based on the time frame when pre-operative heavy bleeding, discomfort, or pain impaired sexual activity and function, then it would certainly be possible for sexual function to improve post-operatively. That does not mean it was an improvement over NORMAL sexual function (pre-gynecologic problems).
This Boston University School of Medicine article discusses post-hysterectomy sexual dysfunction. It says,
“Desire, arousal, orgasm and pain disorders may all be seen post-hysterectomy…..Internal orgasms are often changed significantly after hysterectomy. This is observed in part due to the inability to have rhythmic contractions of uterine muscles without the uterus present. Also, internal orgasms are changed after hysterectomy due to injury to the nerves which pass near the cervix. Surgeons should try to spare these nerves, but efforts to spare them are limited at the present. The result is that after hysterectomy, many women lose the ability to have an internal orgasm.”
Changing the Mindset: Removing a Woman’s Sex Organs Impairs Sexual Function
First and foremost, we need to stop referring to women’s sex organs as reproductive organs since they have vital, lifelong functions far beyond reproduction. In addition to the sexual functions, these include endocrine/hormonal, bladder and pelvic floor and anatomical and skeletal as detailed in my articles and the HERS Foundation’s video.
Secondly, women need to be more open about the effects hysterectomy has had on their health and quality of life, sexual and otherwise. It seems that some do not connect their problems with the surgery and many others choose not to talk about it. Before surgery, we are likely to believe that hysterectomy is fairly harmless since it is such a common surgery (second to c-section). No surgery is harmless. One that removes a woman’s sexual organs cannot help but cause problems with sexual function.
Some other factors that may be in play are that women seem to value their sex lives less than men. We tend to shortchange ourselves in other areas as well, putting others’ needs ahead of our own. Women of older generations were taught to trust and obey authority figures. So we typically trust our doctors and follow their recommendations. We are particularly vulnerable with gynecologists as we tend to have a long history with them through annual well woman checkups and pregnancies and deliveries. We are easy prey for hysterectomy marketing.
Clearly, there are far too many women being harmed by unwarranted hysterectomies and castrations. According to this 2000 study, 76% of hysterectomies do not meet ACOG criteria. Yet the rates have not declined and the use of robotics seems to be fueling even more hysterectomies with promises of quicker recoveries. Hysterectomies are big business with revenues rolling in to the tune of over $16 billion annually. With so much money at stake, we cannot count on the medical establishment to restrain themselves. It is up to us to spread the word.
Does Hysterectomy Affect Sexual Function?
Yes, it does. How can it not, given the nature of the surgical procedure? Whether the effects are generally more negative or positive is not clear. It largely depends on the reason for the hysterectomy including the severity and prolonged nature of those gynecologic problems. There is very little research and even less consideration or conversation regarding women’s pre- and post- hysterectomy sexual functioning. That is something we can change together by sharing our stories and communicating our needs.
Additional Resources
I highly recommend the non-profit HERS Foundation’s video “Female Anatomy: the Functions of the Female Organs.” It taught me most of what I know about the consequences of hysterectomy and/or ovary removal (castration). When I first discovered the video, some of it did not make sense. But as more time elapsed, the changes became clearer. My body and life have changed in ways I never could have imagined. I only wish I had found the video prior to my unwarranted hysterectomy.
We Need Your Help
Hormones Matter needs funding now. Our research funding was cut recently and because of our commitment to independent health research and journalism unbiased by commercial interests we allow minimal advertising on the site. That means all funding must come from you, our readers. Don’t let Hormones Matter die.
Yes, I’d like to support Hormones Matter.
This article was published originally on April 10, 2014.




















