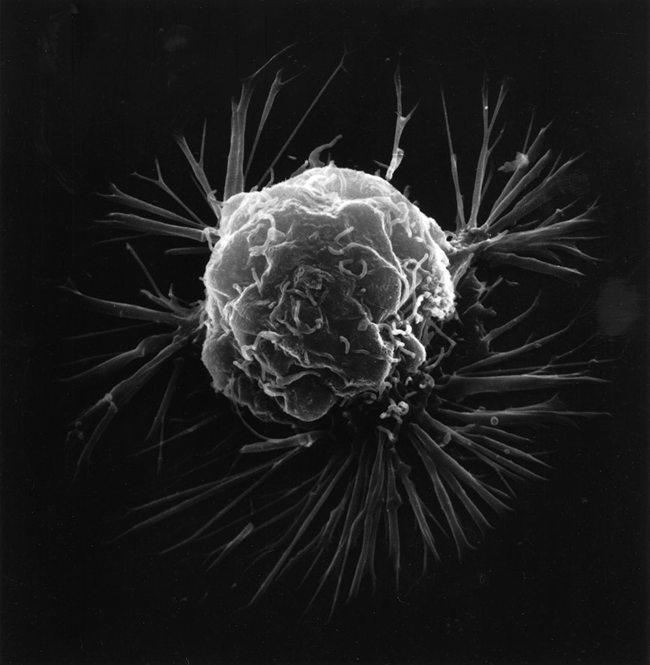
There is ever increasing evidence that energy metabolism is involved in the causation of cancer. A phenomenon known as the Warburg effect has been known for a century and was thought by Warburg to be the cause of cancer. To summarize this effect, normal cells primarily produce energy by the consumption of oxygen in a complex mechanism known as oxidative phosphorylation. This involves the consumption of glucose as fuel. The Warburg effect is because most cancer cells produce energy through a high rate of glucose metabolism by fermentation, even though there is abundant oxygen present. This is a less efficient method of producing energy, an effect that has been much studied but whose mechanism still remains unclear.
In cancer research today, the focus has been primarily on genetic mechanisms and the Warburg effect is considered to be a result derived from these genetic changes rather than the underlying cause. However, energy is vital to normal cell function, so a drop in energy synthesis might be a defect that has a secondary effect on genetically determined mechanisms. Since the vitamin, thiamine, is so closely involved with the metabolism of glucose, it is not surprising that a few researchers have looked at the involvement of this vitamin in relationship to the cause of cancer. For this reason I turned to looking at what medical literature has been published in regard to this and was surprised to find that it was relatively abundant.
Wernicke’s Encephalopathy, Thiamine Deficiency, and Cancer
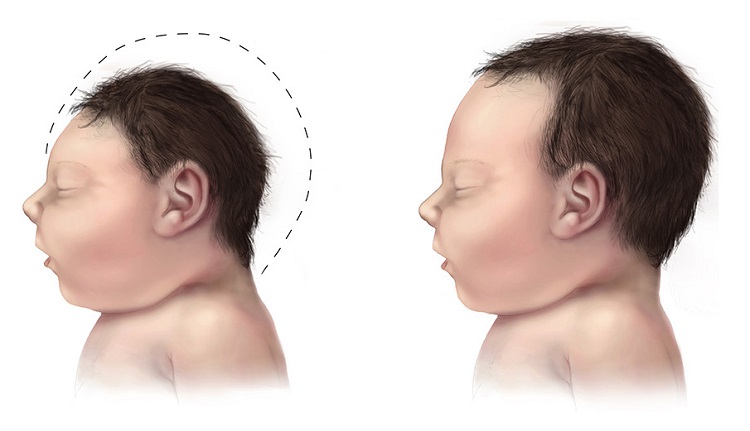
It has long been known that a deficiency of thiamine in part of the brain causes a brain disease that was named after the person who originally described it. This is known as Wernicke encephalopathy (WE). I discovered a manuscript in which 18 patients had developed WE during cancer treatment. Cancers involving blood cells and the gastrointestinal tract were reportedly more common, but poor appetite and weight loss were common risk factors. All of the 18 patients presented with cognitive dysfunction represented by impaired alertness, attention deficit and poor short-term memory. Few of these patients developed the typical symptoms described for the clinical diagnosis of WE, thus making it difficult to recognize the cause of the changes in the patient’s mental status. Of course, the obvious question is whether this is secondary to treatment or whether it is involved as part of the causative mechanism in the cancer. I looked for further evidence.
Breast Cancer and Thiamine Homeostasis
A group of researchers set out to try to find whether there was a difference in thiamine homeostasis (its overall place in body chemistry) in breast cancer cells as compared with normal breast tissue. Without going into the scientific details, they concluded that their findings demonstrated an adaptive response by breast cancer cells to increase cellular availability of thiamine, thus demonstrating its importance to those cells. To explore further the relationship of thiamine in breast cancer, female breast cancer genetically susceptible mice were exposed to 4 diets that varied in fat and thiamine content. The scientific discussion is complex but the authors concluded that there was a potential role for dietary thiamine and an interaction between thiamine and fat in breast cancer progression. This may be important since thiamine has recently been found to be involved in the metabolism of some fats. The findings of a study support the protective effects of thiamine, folate, riboflavin and vitamin B6 against breast cancer in general.
A compound by the name of dichloroacetate has been found to kill cancer cells in breast, brain, and lung cancers in rats, while not harming healthy cells. The anti-cancer effects of this drug have been reviewed. Without indicating the scientific aspects of the study, the authors noted that their findings, together with limited clinical results, suggest that there is a potentially fruitful area for clinical trials with some tumors. A study suggested that high-dose thiamine reduces cancer cell proliferation by a mechanism similar to that described for dichloroacetate.
Surgery, Thiamine Deficiency, and Wernicke’s Encephalopathy
Cancer patients submitted to gastrointestinal surgery are at risk for thiamine deficiency and WE. They often remain undiagnosed and untreated and WE may become manifest several months after hospital discharge. The authors stated that “even in the absence of symptoms of thiamine deficiency the use of prophylactic thiamine supplementation should be taken into consideration, as the consequences of misdiagnosis can be severe “.
With Cancer Genetic Research Dominates
A well-known proverb states that “there is never smoke without fire”. The questions raised in this post suggest that there is indeed “smoke”. There are several obvious reasons why the “smoke” is not being recognized sufficiently to jump start major research. The first reason is that it has been concluded that the Warburg effect is secondary to genetic cause. Genetic issues have therefore become virtually the exclusive approach. However, the available literature suggests that nutritional issues may have an epigenetic (how genes are affected by nutrients and lifestyle) relationship with genetic activity.
I would like to suggest a third issue, the impact of stress. A definition of stress states that it is a mental or physical force requiring brain/body defensive interaction, requiring an individual to adapt to the existing situation. It makes little difference whether the stress is mental or physical. It is the brain that has to conduct the orchestrated reactions. Chronic long-term mental stress is just as debilitating as prolonged physical illness or severe trauma. The reasoning is derived from the work of Hans Selye. For those unfamiliar with this research, Selye stressed rats physically by many different types of assault. It is probable that his cruel experiments, performed over many years, made the recognition of his work much less acceptable. Nevertheless, he was able to determine that physically stressed animals went through several stages of resistance that he called the General Adaptation Syndrome (GAS). These stages were repetitive from animal to animal and were reflected by laboratory changes in tissues and blood similar to those seen in human disease. Selye’s most interesting conclusion was that a great deal of energy was required in order to meet the physiological needs of resistance and that it was a failure of this energy synthesis that caused final collapse. Skelton, one of Selye’s students, was able to induce the GAS by making an animal thiamine deficient, thus demonstrating a relationship with energy metabolism. Selye offered the statement that human diseases were “diseases of adaptation”. His conclusion was more remarkable since little was known during his time concerning the synthesis of energy in the human body. Much more is known now, making Selye’s work more plausible.
Preventing Illness
We cannot avoid the situations of life that give rise to chronic long-term mental stress. If our ability to handle them successfully depends on pristine nutrition, it obviously entails self-discipline as possibly our strongest preventive method. Physical stress may be lethal in its own right but nonlethal injury demands brain activity in coordinating the adaptive defense and is thus just as dependent on brain function. We now know that consumption of energy is greatest in the heart and brain so perhaps it is not surprising that heart and brain disease are so common.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Unknown photographer, Public domain, via Wikimedia Commons.
This article was published originally on September 17, 2018.