Inaccurate theories about how and why endometriosis develops are widely accepted by medical practitioners, despite much evidence against them. Acceptance of these theories leads to the perpetuation of medical therapies that do not work. It is important to understand the origins of endometriosis in order to move forward and develop effective treatments for this devastating disease.
Endometriosis and Sampson’s Theory
Endometriosis is defined as the presence of endometrium-like tissue outside of the uterine cavity. Many medical practitioners and lay press oversimplify this to state that endometriosis occurs when the lining of the uterus is found outside the uterine cavity. However, there are many publications enumerating the differences between endometriosis lesions and the endometrium found inside the uterus. Evidence for this goes back at least to 1981, and possibly earlier, and research into these differences is still ongoing. However, the common perception that endometriosis is merely endometrium outside of the uterus persists.
One prominently cited theory as to how endometriosis develops is known as Sampson’s theory. This theory suggests that retrograde menstruation, menstrual blood flowing backwards (away from the uterus) through the Fallopian tubes towards the pelvic cavity, deposits fragments of endometrium into the pelvis, which can then implant and grow into lesions.
There are numerous problems with this theory. First of all, there is no evidence that endometrial cells in the peritoneal fluid can attach to the lining of the pelvis (the peritoneum), and in addition, endometrial cells are not commonly present in peritoneal fluid. Furthermore, as stated earlier, there are many differences between the endometrium inside the uterus, and endometriosis lesions. In addition, 90 percent of women have retrograde menstruation, but only approximately 10 percent have endometriosis. Sampson’s theory cannot explain the presence of this disease in fetuses, in men, and in girls who have symptoms with the onset of puberty or even prior to puberty. And it cannot explain the presence of endometriosis in areas outside of the pelvis, such as the lungs and skin.
Alternate Theories – A Fetal Component
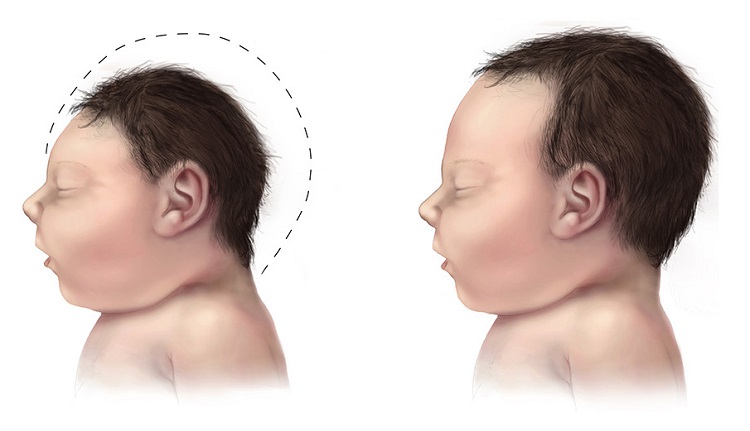
Alternate theories that fit better with the available evidence have been proposed, including metaplasia (changing of one cell type into another cell type), developmental defects (also known as Mullerianosis), genetic factors and environmental factors. However, no single theory has been proven to be correct, and most likely a combination of various influences contribute to the development of the disease. According to the current evidence, there is most likely some embryological component. The theory of Mullerianosis explains the development of endometriosis as endometrial tissue that was misplaced during fetal development, that later develops into endometriosis lesions. Evidence in support of this comes from the fact that endometriosis has been found in female fetuses with the same incidence as in women, about 10 percent.
The Persistence of Sampson’s Theory – A Safety Net for Inadequate Treatment
Why has Sampson’s theory continued to be so persistent despite all the evidence to the contrary? First, no alternative theory has been sufficiently proven enough to displace it, although certainly enough evidence against it exists that it ought to be displaced. Second, most doctors who treat endometriosis do not specialize in the disease, and the science behind its development is probably not something they have much interest in.
It is damaging to endometriosis patients to have Sampson’s theory continue to be accepted despite evidence to the contrary. It gives gynecologists a reason not to strive for complete removal of the disease from all organs, because there’s no point in trying to remove all of it, if it will just be re-implanted with the next period. Sampson’s theory provides justification for the high recurrence rates observed from surgeons who do not specialize in treating endometriosis.
However, surgeons who specialize in it, who carefully excise all disease, have shown that it is possible to have low recurrence rates following complete excision. This requires not only the knowledge of all the possible visual appearances of endometriosis, but the surgical ability to excise disease from areas most gynecologists cannot, such as bladder, ureters, intestines, or diaphragm.
Sampson’s Theory and Medications that Prevent Menstruation
Acceptance of Sampson’s theory gives pharmaceutical companies an excellent tool to convince doctors to prescribe medications that prevent menstruation. If Sampson’s theory is correct, then any hormonal treatment that stops women’s periods will treat endometriosis. Several drugs that are currently on the market can stop periods—Lupron and similar drugs, by inducing a menopausal state, and birth control pills, used continuously. However, as would be expected, since Sampson’s theory is not correct, these medications have never cured endometriosis. Some patients may experience temporary relief of symptoms, especially when the symptoms are primarily connected to having periods, but hormonal medical therapies do not treat the underlying disease.
The Origins of Disease Matter
Though debating disease origins may seem like an arcane point, not relevant to most endometriosis patients on a daily basis, it is highly relevant because it is so linked to the inadequate and ineffective treatment most patients receive. In order to truly move forward and make progress in how this disease is treated, wider recognition of Sampson’s theory as fatally flawed must occur. If endometriosis is present in the fetus, then it is an entirely different disease than one of retrograde menstruation. Understanding this is critical for better treatments options.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
lunar caustic, CC BY-SA 2.0, via Wikimedia Commons.
This article was published originally on October 2013.