Over the last several weeks I have been the beneficiary of a fair amount of synchronicity; seemingly random introductions to interesting people and research connections from disparate sources. Not the least of which was a recent introduction to the concept of lactate doublets. What the heck are lactate doublets? I had no idea and I am certain most of you reading this do not know either. Well, it turns out lactate doublets may be a missing piece in the diagnostic puzzles that present post medication and vaccine adverse reactions. Let me explain, but first a bit of background.
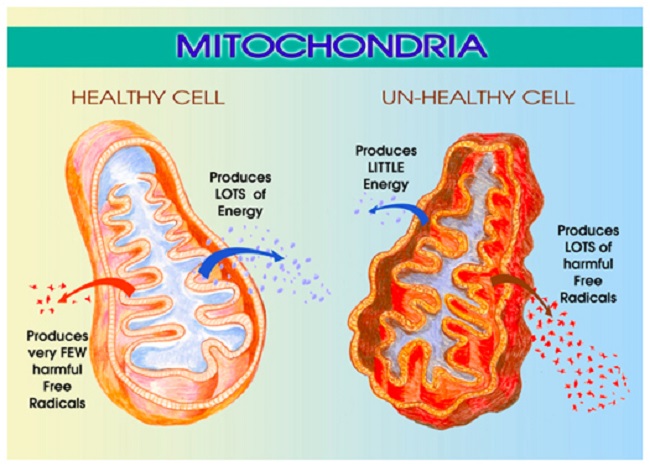
Mitochondrial Dysfunction
If you’ve followed Hormones Matter for any length of time, you know that we cover complicated diseases and medication and vaccine reactions. Inevitably, these reactions include neurological and neuromuscular symptoms that, almost to tee, fail to show up on standard diagnostic testing. This is particularly troubling when the symptoms include seizures, migraines, tremors, ataxias, neuropathies, dysautonomias and other obvious signs of nervous system damage.
We’ve attributed many of these cases to mitochondrial damage and subsequent dysfunction but testing for damage has proved problematic in most cases. While genetic disorders of mitochondrial dysfunction are reasonably well documented, the more dynamic, environmental and even epigenetic functional changes suspected in toxin, medication or vaccine induced mitochondrial disease are neither well documented nor easily recognized. With no easy testing, folks whose mitochondria are functionally or operational deficient, suffer needlessly and chronically. So when I read the report about lactate doublets as evidence of mitochondrial dysfunction in autism, I was intrigued. And, since I had just attended a talk on the mechanics of measuring basal metabolic rate as indicator of mitochondrial respiration e.g. mitochondrial functioning, I was doubly intrigued. Could we use these measures as pre-screening tools for mitochondrial damage in health and disease? After all, what could be more fundamental to overall health and cellular energetics than aerobic and anaerobic metabolism? Identify problems with energy metabolism and there’s a good chance something is hinky in mitochondria land.
The Wonders of Lactate
For those of you who are athletes, lactic acid and lactate are familiar topics. For those who are not athletes, consider the last time you exercised rigorously and that point at which the demand for oxygen and fuel for your muscles out-paced your body’s ability to adapt and provide that fuel. What happened? Your muscles began to fatigue, you slowed down, you may have begun to hyperventilate and eventually you hit the wall, exhausted.
If you’re an athlete, a large part of your training involves moving that exhaustion threshold, that wall, further and further away. You train to increase muscle strength – anaerobic capacity, cardiopulmonary functioning- aerobic capacity and the tolerance for pain. Lactate production and utilization is the key to training and athletic success. In the common vernacular, lactate is incorrectly referred to as lactic acid. They are two different molecules. Lactic acid is precursor to lactate and lactate is both a substrate and a product of anaerobic metabolism. Lactate is currency for energy metabolism between cells, tissues and organs. The point at which lactate production outstrips its utilization as fuel or energy is one of the first steps of fatigue in healthy, athletic individuals. In not so healthy individuals and many disease processes, excess lactate can be a marker for mitochondrial dysfunction. In not so healthy individuals where the mitochondria are functioning sub-optimally, that feeling of hitting the exercise wall, is continuous with normal activity.
Lactate and Mitochondria
Over the last several months we’ve discussed mitochondrial ATP production on a number of occasions, mostly in relation to the aerobic process of the energy production that converts glucose (sugars) to adenosine triphosphate (ATP), the cellular energy that fuels our existence. This process requires large amounts of oxygen and numerous chemical co-factors, thiamine being one of the more major among them. Diminish oxygen levels or one of the necessary co-factors and energy/ATP production is reduced.
Not to worry yet, we have a backup or secondary ATP production cycle involving lactate. Here glucose is converted to compound called pyruvate which then is either shuttled into the mitochondria to produce ATP or it remains in either the extracellular or intracellular cytosolic (cell fluid) space and is converted to lactic acid and then to lactate. The pyruvate>lactate path is anaerobic. That is, it does not require oxygen. The heart, kidneys and liver prefer lactate for fuel and rely heavily on anaerobic metabolism. In our exercise model, anaerobic metabolism and increasing lactate production parallel increasing exercise intensity, though it is less efficient. In comparison to aerobic metabolism that produces 38 mol of ATP, the anaerobic pyruvate>lactate path produces only 2 mol ATP.
The connection between lactate and mitochondrial functioning was only recently discovered and remains hotly debated. For a long time, it was believed that lactate remained outside the mitochondrion. Now, evidence suggests that mitochondria can convert lactate to ATP and that lactate is shuttled in and out of mitochondria to be used when needed. Based upon this possibility, measuring lactate either alone or in combination with respirometry measures may provide an indirect marker of mitochondrial functioning. Here’s where it gets interesting.
Body and Brain Lactate
Lactate is a fuel used readily in the body. Lactate levels change relative to metabolic needs (exertion and stressors) and efficiencies (oxygen usage, co-factor availability). Exercise physiologist have been measuring lactate and other indicators of metabolic functioning and path (aerobic versus anaerobic) for decades using a variety of respirometry tools, from breathing apparatus to blood tests and tissue biopsies. In a grossly oversimplified manner, the extent to which one produces and utilizes lactate during training indicates one’s overall fitness. Could we use some of those same tools, the less invasive ones, to provide a broad indicator of mitochondrial health? Yes, we can.
Indeed, those same aerobic/anaerobic processes that occur in our body occur in the brain. Even though the brain is a huge consumer of glucose as its preferred fuel, recent evidence suggests that it also produces and consumes lactate in parallel to the body during exercise and other stressors. Beyond just the production of lactate in brain trauma, where oxygen and glucose are depleted rapidly and chronically, brain lactate levels appear to correspond with shifts in aerobic/anaerobic metabolism.
My thought, and what began this entire adventure, couldn’t measures of aerobic/anaerobic metabolism be adapted to compare healthy mitochondrial functioning versus non-healthy mitochondrial functioning? Wouldn’t a skew towards anaerobic metabolism and excess lactate, especially during rest and low exertion, indicate, at least broadly, mitochondrial damage? The answer is yes; measures of respirometry, along with body and brain lactate could broadly indicate mitochondrial functioning.
But wait, there’s more. Instead of tissue biopsies, and perhaps even instead of the blood tests, researchers have figured out how to image lactate metabolism within the brain and presumably the body. Enter the lactate doublet.
Imaging Lactate with Magnetic Resonance Spectroscopy
Magnetic resonance spectroscopy (MRS) is like a magnetic resonance imaging (MRI) except that instead of simply taking pictures of the tissue, through a myriad of complicated calculations, the MRS measures the relative concentrations of specific metabolites in the brain and other tissues. The MRS can measure lactate metabolism in the brain and researchers around the world have begun to look at brain lactate as markers of different disease process, like autism, aging and brain injury. It is not without technical difficulties (machine calibration is complicated) and controversy, especially around the clinical interpretation, but I surmise it will open up a whole new area of diagnostic possibilities once the early glitches are worked out.
What is a Lactate Doublet?
The lactate molecule has two, weakly coupled, signals or resonances. When viewed on the MRS the lactate doublet presents as a double peak in the signal algorithm.
Lactate Doublets in Cerebral Mitochondrial Dysfunction
The presence of lactate can be diagnostic of specific types of brain tumor or stroke. Since lactate is elevated in mitochondrial disease, evidence of lactate doublets from MRS, even when MRI imaging shows no irregularities, can point to cerebral mitochondrial dysfunction. More specifically, in patients with genetic mitochondriopathies researchers have been able to delineate the regional differences in brain lactate corresponding to the neurological and clinical symptomotology associated with each mitochondriopathy. As was indicated previously, lactate doublets have been recognized in autism, aging (although mechanisms remain contended) and other mitochondrial disease processes.
Using MRS and Respirometry to Detect Post Medication or Vaccine Induces Mitochondrial Damage
Dynamic and functional changes to mitochondria are emerging as culprits in the more complicated adverse reactions we observe post medication and post vaccine. Recognizing the potential for mitochondrial damage post reaction is difficult, especially those impacting the nervous system. Conventional MRI’s and other imaging tests rarely detect visible lesions that can be attributable to clinical symptoms and standard blood tests are often normal, leaving the doctor and the patient without recourse. In advance of genetic testing and the measurement of each co-factor required for proper mitochondrial functioning, respirometry and MRS could be used to identify potential deficits in mitochondrial functioning. Measuring respiratory efficiency and lactate production and usage efficiency could be an easily detectable marker to rule in or out mitochondrial dysfunction. Those results could then be used to determine the need for additional testing that would identify more specific causes of mitochondrial dysfunction.










I’ve experienced lactic acid in my thighs after minimal exercise , this started about 10 years ago and got to it’s worse 4 years ago. Although i have improved the situation over the past 4 years (intense burning when standing for more than a minute) to the starts of burning after 5-6 unweighted squats, the issue is not resolved.
I’ve been taking allithiamine 350mg for 4 months but I’ve not yet noticed any improved in terms of muscle function.
Is there any tests to work out if it’s a lack of oxygen , disfuctioning mitochondria or what the root cause is?