Last week, I posted yet another story on our Facebook group about how women’s health is ignored and psychologized by the medical profession. It is neither a new topic nor something particularly earth shattering. We post hundreds, if not thousands, of these stories both on our Facebook page and on Hormones Matter itself. Indeed, the entire premise of Hormones Matter is that these narratives matter, that there is truth and wisdom in the patient’s account of her or his health, something that has been lost in modern medicine over the last several decades.
The premise of last week’s article was that we rarely, if ever, believe women when they present health issues, sometimes with deadly consequences.
For decades, studies have shown that women with chronic pain conditions are more likely than men to be wrongly diagnosed with mental health conditions and prescribed psychotropic drugs. When men and women offer similar complaints of pain, women are more likely to be prescribed sedatives instead of pain relieving drugs. Further, a newly released study on women’s mortality rates after heart attack offers this insight, ‘Most physicians are male, and male physicians appear to have trouble treating female patients’.
The author of the article argues that the problem rests on the maleness of the medical profession. She is correct, but there is so much more to the story. While it is true that from the beginning of medicine women were excluded from not only the practice of medicine, but also, in building the current medical knowledge base. It is also true that entire body of knowledge cultivated by female caregivers, midwives and the like was usurped and essentially dismantled as our current model of medicine took over, medicine itself was never designed to ‘listen’ to or believe patients, male or female. From an article I wrote on the topic several years ago:
Historically, listening to patients has had a tenuous position in medicine. Some would argue that it was supplanted long ago by the physician’s all-knowing clinical gaze. The clinical gaze, a term used by French philosopher, Michel Foucault, is the ability to see correctly what is unseen, to bring to light and then describe the hidden truth of disease. It was what allowed the physician to penetrate the illusions of the non-scientific engendered by previous generations (16th – 18th century medicine) and to see the truth of the disease by correctly perceiving the signs and symptoms. The physician’s power of observation, his clinical gaze, aided by technology, gave him a vantage point inaccessible by mere mortals, and thus, incontrovertible.
The clinical gaze anchored modern medicine in a way that no other concept could. It brought with it the power to see truth, but also, to define it. No matter how potentially relevant to disease diagnosis, the patient’s truth or story could never replace the physician’s truth – the truth that was accessible only by him and through the all-knowing clinical gaze.
And so it was for most of the last century and a half, the physician was the arbiter of what was valid, of what could be seen and of what could be known about health and disease. The patient was no more than a body; living or dead, it did not matter. It was the job of the physician to perceive correctly what the body (not necessarily the patient) was showing him and then classify, communicate, and finally, treat appropriately.
What folks who attribute the problems in women’s health solely to the maleness of the specialty fail to recognize is that the foundation upon which modern medicine was built rests entirely on the physician’s ability to ‘see’ the signs of illness in a body and validate those observations correctly via the appropriate measures. If the physician does not perceive the signs of the illness at all, or correctly, or in a manner that can be measured, then necessarily, the symptoms with which the patient presents are not to be believed.
Certainly, there is gender bias. That is obvious. A system of knowledge designed by men, about men and for men, with women and their bodies viewed as aberrations to the normative male body, comes with a deeply ingrained bias. More than that though, the notion of perception as the defining characteristic of medical reality limits significantly what one can and cannot know about any given topic. Consider the age old philosophical riddle posited by George Berkeley and debated by philosophy students for generations:
If a tree falls in a forest and no one is around to hear it, does it make a sound?
At the root of this question is whether awareness predicates existence. According to Berkeley, material reality, for all intents and purposes, does not exist unless it is observed. Thus, awareness predicates existence. In that same regard, medical reality does not exist unless it too is observed by the physician. Even when observed, however, if that observation cannot be validated by some objective test, then the physician is forced to dismiss his original insight and attribute the suffering to some errant ephemera, typically of the psychological nature.
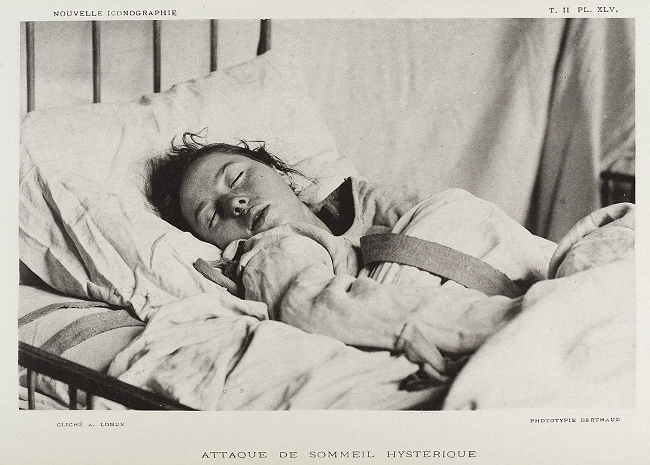
Inasmuch as women’s symptoms were never ‘seen’ in the first place, never investigated, never documented, never even considered really, then it is to be expected that they would not be believed. Women’s health problems just do not exist, in much the same way that the tree falling in the forest does not. They are immaterial, incorporeal, or as Freud suggested, ‘hysterical’. (Admittedly though, Freud listened to female patients. He simply misattributed what he learned to the machinations of the female mind never envisioning a physical culprit for their ailments.) While this in no way excuses the egregious ignorance about women’s health issues that permeates modern medicine, it does shed light on why it exists. It is a consequence of establishing a system of knowledge based solely upon the perceptive abilities of a specific group of individuals. In this case, male physicians, but one could argue, that any system predicated upon perception and perception alone would have similar limitations (see here or here). If awareness predicates or defines existence, then no matter who is in charge, a good chunk of reality, even medical reality, is immaterial, and thus, unimaginable.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Image: Wellcome Collection gallery (2018-03-29): https://wellcomecollection.org/works/h5njm9mw CC-BY-4.0
This article was published originally on January 8, 2019.















Read the many articles on this website
Hello Ms. Marrs. This article does not pertain to me, but I would really appreciate any advice you have for my story, and how to solve my problems.
I wrote my story on another article on this website (https://www.hormonesmatter.com/brain-long-term-lexapro-chemically-induced-tbi/#comment-270718), and I was wondering if you could lend your insight into my case, and what I should have done to solve it, and get properly diagnosed.
The main problems for me as I write this are brain fog, memory loss, nerve problems in the left side of my body, from my face down to my foot, numb emotions/low libido, genital numbness, breathing problems (could be dysautonomia, my brain makes me manually breathe a lot), and sinus dryness. I still get ear ringing every so often, but not nearly as much.
I would appreciate any help you can give. I feel so abandoned. The APRN refused to help me after I got these problems, it feels like malpractice. I’ve seen doctors all year and nobody is able to diagnose me or solve my problems. It’s taken a big toll on my outlook on life.