Among the many symptoms of vaccine adverse reactions is brain inflammation, often considered idiopathic or of unknown origins. There are a number of potential culprits underlying vaccine related brain inflammation, including the virus vectors, the neurotoxic adjuvants or the cocktail mistakenly presumed inert ingredients that accompany any vaccine. No matter the cause, however, once inflammation is unleashed within the central nervous system, the inflammatory response itself can become self-perpetuating, initiating secondary pathologies that are chronic, progressive and neurodegenerative.
Chronic brain inflammation, like inflammation in the rest of the body, is now considered one of the leading causes of disease. In the brain, chronic inflammation is believed to lead to Alzheimer’s, dementia and Parkinson’s, while chronic inflammation in the body is connected to heart disease, type 2 diabetes, depression and a myriad of autoimmune diseases. At the center of all inflammatory diseases are dysfunctional mitochondria that, as regulators of the cell survival and number of other functions, control immune reactions – inflammation. Mitochondria are highly susceptible to damage from pharmacological and environmental toxicants and inextricably dependent upon dietary nutrients for proper functioning. When toxicants attack mitochondrial pathways and/or nutrient depletion diminishes mitochondrial functioning, mitochondria activate the immune system and spur inflammatory cascades; cascades that can be stopped only if the exposures are removed and the nutrients restored.
In the brain, neural mitochondria and microglia (brain immune cells), regulate inflammation. Like the mitochondria, these microglia are highly dependent upon dietary nutrients. As we have written previously, the B vitamins are particularly important for central nervous system functioning. New research finds that vitamin B6 is a key regulator of brain inflammation.
Vitamin B6 and Brain Inflammation
Vitamin B6 (pyridoxine >peridoxal 5’ – phosphate) is a necessary co-factor in over 100 enzymes. It is critical for the catabolism (breakdown) of the essential amino acid tryptophan. Tryptophan is required for serotonin (well-being and GI motility) and melatonin (the sleep hormone) synthesis. Disturbances in tryptophan catabolism not only lead to disturbances in neurotransmitter activity, but also, can lead to cell death or apoptosis, in vital brain regions, like the hippocampus (learning and memory), basal ganglia (movement, motivation, intention) and in the cerebellum (motor control and balance).
When all is working well, tryptophan serves as a substrate for serotonin and melatonin. Excess tryptophan is degraded resulting in the by-products nictonic acid and nicotinamide adenine dinucleotide (NAD+) – or as most of us recognize, niacin, vitamin B3. Niacin is an essential nutrient in many physiological functions. Loss of niacin metabolism from this pathway can lead to significant disease, including, Pellagra, a disease characterized by scaly skin lesions, delusions and confusion. In addition to a loss of niacin synthesis, when vitamin B6 is deficient and the tryptophan pathway is disturbed, the incomplete degradation of tryptophan produces several metabolites that are neurotoxic, including one called quinolinic acid.
Quinolinic acid is a potent and self-perpetuating neurotoxin when unopposed in the brain. It generates ROS (reactive oxygen species indicative of mitochondrial oxidative stress and damage) and over-activates NMDA glutamate receptors (the brain’s primary excitatory neurotransmitter) to the point of apoptosis (cell death), all the while inhibiting brain astrocytes’ ability to clean up the excess glutamate. Once that cycle becomes initiated, quinolinic acid potentiates its own release and that of other neurotoxins, ensuring continued brain inflammation and damage.
With the appropriate vitamin B6, quinolinic acid is not the final product of tryptophan catabolism, NAD+ or niacin is, and any damage initiated by quinolinic acid as a natural by-product within this pathway is offset by two neuroprotective factors, kynurenine and picolinic acid. Vitamin B6 is critical for the kynurenine aminotransferase and kynurinase enzymes; enzymes that lead to neuroprotective compounds, kynurenine or picolinic acid. Kynurenine blocks the cytotoxic effects of quinolinic acid by blocking the NMDA receptor, making it unavailable to quinolinic acid, while picolinic acid is the primary metal chelator (remover) in the brain (likely critically important in post vaccine reactions). In other words, vitamin B6 controls the balance between inflammation and anti-inflammation within the brain and the body.
How do We Know Vitamin B6 is a Neuroprotectant?
Well, we’ve actually known this since the 1970s (perhaps earlier) when work on the kynurenine pathway began. Somehow though, it wasn’t recognized again until the 1990’s and has only recently become prominent over the last decade as connections between environmental and pharmaceutical toxicants and gut microbiota and mitochondrial damage are revealed.
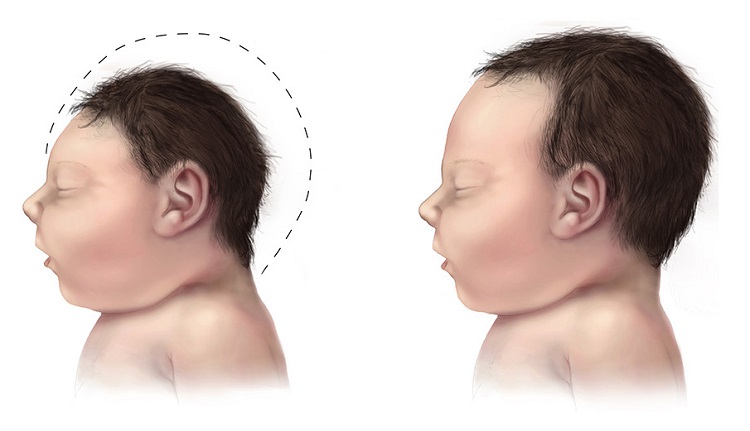
Several studies have emerged over the last decade showing the importance of vitamin B6 (and other B vitamins) in systemic and brain inflammation. Defects in vitamin B6 metabolism are linked to seizure disorders resistant to traditional anticonvulsants but remediable with Vitamin B6. Vitamin B6 reduces brain atrophy in Alzheimer’s patients. Low vitamin B6 is believed to play a key role in the oxidative stress associated with Huntington’s disease. One of the more interesting studies involves preventing the hippocampal apoptosis associated with bacterial meningitis using vitamin B6.
Bacterial meningitis is a life threatening disease associated with high mortality and morbidity. Of those patients who survive, up to 50% suffer serious neurological impairment including: hearing loss, seizures, cognitive decrements and sensory-motor deficits. The bacteria attack cortical and hippocampal regions of the brain. Hippocampal cell death is associated with learning and memory deficits. In an experimental version of bacterial meningitis with rodents, researchers tested whether vitamin B6 supplementation could prevent the hippocampal apoptosis by moderating the tryptophan pathway towards the B6-dependent kynurenine and picolinic metabolites versus the neurotoxic quinolinic acid. They were successful. Vitamin B6 supplementation reduced brain inflammation and hippocampal apoptosis by up-regulating the neuroprotective factors controlled by the tryptophan – kynurenine pathway. An impressive result reached simply via vitamin supplementation.
Final Thoughts
Tryptophan metabolism and the kynurenine pathway are implicated in disease processes where inflammation is prominent. Vitamin B6 may be critical to maintaining the appropriate balance between inflammatory and anti-inflammatory immune reactions. With modern nutritional deficits (high calorie, low nutrient foods), commercial agricultural practices (glyphosate doused crops are nutrient poor), estrogenic medications and environmental exposures (estrogens inhibit vitamin B6), it entirely conceivable that many of us are vitamin B6 deficient and, as a result, functioning with a constant level of inflammation. Vitamin B6 supplementation, along with the other B vitamins might be warranted.
For those individuals suffering from brain inflammation mediated by disease, medication or vaccine adverse reactions, vitamin B6 might just reduce the inflammation cascades and improve quality of life. Given its direct impact on tryptophan metabolism, vitamin B6 ought to be considered critical for brain health.











Thanks for the information, impeccable! ♡
Dear Dr. Marrs and Dr. Lonsdale,
I found this post to be intriguing. I take high doses of B6 & Zinc together with two less essential nutrients for the treatment of putative “Pyroluria”. I know there is debate as to whether this is a real condition, what I can say is that when I found the optimal dosages of b6 and p5p it had a very positive effect.
I’ve recently have become convinced that inflammation is inextricably intertwined with my physical issues and have been researching how to reduce it. Among many other things, I came across PQQ and a study showing that it significantly reduced CRP (45%) and notablely reduced IL6 as well in a short period of time.
https://www.sciencedirect.com/science/article/pii/S0955286313001599?via%3Dihub
At first, I dismissed the study as too good to be true and wondered if the results are really indicative of reduced systemic inflammation or if the PQQ somehow caused a lower crp/il6 response without reducing systemic inflammation (i.e. PQQ somehow chemically affecting those markers only ) which would not necessarily be a good thing as it could give one a false sense of security regarding their inflammation status. After being reminded that the root of inflammation is primarily mitochondrial dysfunction I thought twice.
I am not a biochemist so I have no idea if such a thing is possible and thought I would bounce this question off of you.
Thank You!
Do high serum B6 levels matter? Does a serum level reflect CNS level B6? Should a person avoid B6 if their serum level is high?
What might be a good direction to look if I don’t tolerate b6 or p5p (don’t tolerate most supps each in dif ways). Seems like it may be a glutamate type reaction, headche, fog, achy. Lots of glutamate issues. Tested high in kryptopyrolles. Process stress very poorly. I might do better with foods containing it. I only need very small amounts of most things. Mom and grandma had Alzheimer’s, stroke, dimentia. I have lot of methylation defects. Any thoughts or other articles may help, or a suggested practitioner. Thanks!
I came across this article , when I was hectically searching web for elevated quinolinic acid in urine. My 19 yr. old son who is suffering from autism was recently tested for urine OAT. His KYN acid is 0.0 , while QUIN acid is on higher side.On serum amino acid test, he is deficient of L-tryptophan and L-tyrosine is on higher side. The OAT also shows that HVA is on higher side while VMA is on lower side.To reduce his aggressive behaviour , we supplement nearly 1g L-tryptophan per day. Even though his violent behaviour gets reduced with L-tryptophan, he does not sleep adequately. His sleep reduces in proportion with L-tryptophan supplementation. To me it appears that elevated Quinolinic acid may be the reason behind disturbed sleep. If I stop L-tryptophan , his periodic violent behaviour ( once in a week) returns but then sleeps more than required. Supplemental vit B6 of 50 mg/day may not be adequate. Any suggestion from anybody ? Thanks
Hi Vivek,
Unfortunately, I am just a researcher and have no clinical experience and so I cannot offer any clinical advice. I do suggest, however, you also read some of our many articles on thiamine, vitamin B1. That too is implicated in this pathway and others and may be of use for your son.
Thank you very much for your reply. Among several other abnormalities, the urine OAT also showed elevated L-lactate. After a little bit of research and from the experience of parents having autistic kids, we started supplementing Thiamine, Vitamin B1,100mg with 100mg benfotiamine per day divided twice. He was immediate responder for this combination. We are very happy for this intervention. His frequent non stop walking for several hours stopped within a day. Frequent blood testing and urine testing and subsequent intervention, we have helped our son immensely and we will continue to do so. Information provided by researcher like you is of immense help to us in the battle against our sons autism. We will continue to share our attempts with other parents.
Vivek, if you’d like to share what you have learned and what you are still yet trying to figure out in a blog post, that would be so helpful for me and other researchers as well other parents and patients. I find that parents and patients tend to know much more about some of the intricacies of these complicated health conditions then most physicians and many researchers. We learn much from these types of posts. Please consider it.
low dose niacin does help curb quionoleic acid production. our kid has CBS mutation and high dose vitamin b6 is suspect. We use both low dose b6, niacin and folinic acid.
Thank you for this helpful article. Very insightful with references. What are your thoughts on B3 in Niacinamide Riboside form to reduce quinolinic acid?
Thank you Dr. Marrs for explaining the ‘why’ for B6-my son, now adult son, was dx with regressive autism, pdd @ 20 months-he is now 32. Dr Bernard Rimland was the advisor I followed for autistic nutrient guidelines. He recommended B6/mag. as a therapy. I followed this in ratio to weight throughout my son’s earlier years and had slacked off during his early 20’s when he presented with new and rather dysfunctional behaviors. At this point he was given pharmaceuticals (atyp anti psychs and lithium), which he takes to this day… but I’ve regained my focus and am tapering his doses and moving toward bio-physical supplements. I also was dx with lyme in 2011, did the standard 22 d antibiotic course(chronic with this spirochete)-so I am beginning the B6 therapy as well as my son. I’m so happy you explained the why of brain inflammation. I like to know why a thing occurs not just that it’s been diagnosed.
Juliette
The post on vitamin B6 is highly technical and must be rather difficult for some readers to understand. It makes it very clear that the biochemistry of a single vitamin is extraordinarily complex. As a physician I have often been asked what appears to be a simple question ” what is vitamin (A, B, C, D, magnesium, calcium Etc) good for)? The question is based on the present medical model. This model states that each disease, or even a symptom (Parkinson’s, Alzheimer,etc.) has a specific cause and a specific treatment. The pharmaceutical industry depends on this model as research seeks to find a ” wonder drug” for each disease. Vitamin B6 is but one member of a complex team of vitamins and minerals, known collectively as non-caloric nutrients. The function of each cell in the body depends on genetically determined enzymes that include a vital group involved in the synthesis of energy. They, in turn, are dependent on vitamins and minerals as cofactors. The enzymes gradually decay without them and that is why nutrition is so important. Because the brain is the most metabolically active tissue in the body, its energy requirement is huge. It is therefore hardly surprising that chemical changes in brain cells can result in changes in behavior. A high calorie intake without the vitamins produces changes in that behavior, a form of malnutrition that is quite different from that of starvation. The affected individual becomes much more emotionally irritable and the autonomic nervous system becomes erratic and dysfunctional. That is why I have repeatedly suggested that high calorie malnutrition may be responsible for some cases of irrational behavior, extending even to violence. It is high time that the model for disease be revised. To understand biochemistry and its relationship to fuel consumption should be the medicine of the future.