Ladies, here is a typical scenario of a happily-married couple with two children, who now desire permanent sterilization. They do not want children any more; she does not want a pregnancy now, nor in one year (i.e., the FDA’s definition of “permanent”). She and her husband want no more kids.
What are their options? Bilateral Tubal Ligation (BTL)? What is Tubal Ligation Syndrome? Does she take out her ovaries? Why can’t the man just get a vasectomy? Fifteen percent of men do. One study shows that a man undergoing vasectomy at a young age may lead to a more aggressive form of prostate cancer later in life. Not an option, young men.
For women, starting from the least “invasive,” to the most “invasive” (and not meant as a comprehensive list or as medical advice or treatment; most doctors would say that you need to talk this over with at least 2 doctors), here is a general outline of permanent birth control choices.
Things to remember as you review the possibilities of permanent birth control:
- Speak up and ask questions! These are not easy decisions and the choice you make will impact the remainder of your life. Do not let anyone make this decision for you.
- Understand all of the risks associated with the procedure you choose. Compare those to the risks associated with alternative options, including the option of not having the procedure done.
- Always seek a second opinion; and sometimes third and fourth opinions.
- Use social media to talk to other women who have gone through the procedure.
Bilateral Tubal Ligation (BTL) for Permanent Birth Control
Bilateral tubal ligation or BTL is the most common method of family planning for permanent birth control with up to 33% of married women worldwide opting for this method.
A BTL is best performed during or up to a few couple days after childbirth, when the uterus is still swollen, and the Fallopian tubes are just under the skin. There are many different types, all requiring spinal anesthesia for optimal pain control and patient satisfaction.
Bilateral tubal ligation involves surgery to block the fallopian tubes and prevent the ovum (egg) from being fertilized. BTL can be done by cutting, burning or removing sections of the fallopian tubes or by placing clips on each tube. It is 99% effective after the first year.
Risks Associated with Bilateral Tubal Ligation
Over time, the tubes can reconnect. This happens with 15 – 20% of BTLs performed. When the fallopian tubes reconnect, it is possible for the woman to become pregnant. This can lead to a tubal or ectopic pregnancy.
A tubal/ectopic pregnancy is a life-threatening condition that warrants immediate attention.
With an ectopic pregnancy, the fertilized egg remains in the fallopian tubes rather than implanting in the uterus. It cannot survive in the fallopian tube and without immediate surgery; the mom is at risk for bleeding to death. Emergency surgical removal of ectopic pregnancy is warranted.
Take heart, as you are NOT killing your baby. As an anesthesiologist against abortion, I have had many religious discussions with many concerned women. I assure them that I have never given anesthesia for an elective abortion because I think it goes against the Hippocratic Oath. I have only given anesthesia to SAVE THE LIFE of a mother with a tubal pregnancy. We usually pray before going into the operating room and the anesthesiologist gives sedatives. The patient should have no memory of even being in the operating room.
In addition to the risk of ectopic pregnancy, there are additional side effects and contraindications to consider with this form of permanent birth control. One of the most common ‘side effects’ is a set of symptoms called post-tubal ligation syndrome. The symptoms associated with post-tubal ligation syndrome include: increased menstrual bleeding, decreased libido, fluctuating mental health, and more pronounced PMS, abdominal pain, some leading to hysterectomy, and more. The validity of the symptoms associated this syndrome have been fodder for scientific debate for decades and decades. The research is mixed.
In 2005, Shobeiri et al (2) showed in 112 post-Pomeroy BTL patients vs. ‘normal’ patients that menstrual abnormalities did not differ. However, women in two age categories experienced statistically more uterine bleeding: ages 30 – 39; and ages 40 – 45. In 2011, Moradan et al studied 160 women, finding no changes due to BTL (3).
Although there may be an increased rate of hysterectomy due to increased menstrual bleeding after a BTL, nowhere in the medical literature can a biologic correlation be found as the culprit, except with the decrease in hormones produced after an oophorectomy. However, talk to individual women, glance through Facebook and other social media sites, who have had tubal ligation and developed post-tubal ligation syndrome, and see that these women are hurting and suffering. Their stories should be considered as one contemplates this form of permanent birth control.
For my part, perhaps what we need now is a study that includes an n > 10,000, since the rate of hysterectomies is so high in the United States.
Reversing Bilateral Tubal Ligation
Reversal of BTL requires microsurgery, and a fertility specialist may be consulted. Remember to get 2nd Opinions on any surgery, and take someone with you. It makes the most sense to go to a surgeon who does this frequently, rather than go to a surgeon who does this infrequently.
Surgical Methods for Tubal Ligation
- Bipolar Coagulation: cauterizes portions of the fallopian tubes
- Monopolar Coagulation: same as (A) + radiating current for more damage + cutting the tubes at the end
- Fimbriectomy: takes a part of the fallopian tube that is closest to the ovaries, preventing the tube from accepting an egg, and therefore from fertilization
- Irving Procedure: two ties are placed at a length on one fallopian tube; then the tube is cut between the ties, and sewn to the back of the uterus
- Tubal Clip: metal tubal clips made by Fishie(R), or Hulka (R): smashes the Fallopian tube shut, so the egg does not pass from the ovary to the uterus
- Tubal Ring: with a silastic Band or Tubal Ring, the Fallopian tube is doubled up and then surgically placed to clamp it shut
- Pomeroy Tubal Ligation: often referred to as having the Fallopian tube “cut, tied, and burned”
- ESSURE(R) Tubal Ligation*: Nickel-plated and fiber coils are screwed into each Fallopian tube through the vagina, under spinal anesthesia or pelvic block. An immune response is desired, causing inflammation and scar tissue, blocking the tube from receiving sperm. The FDA states that “permanent,” specifically with Essure(R), is “one year or more.” Controversy surrounds this metal device implant, which has been known to lead to side effects in individual patients (including but not limited to): breakage of coils into pieces; tubal pregnancies; perforation (i.e., poking a hole through) of the coils through the fallopian tubes; perforation of the uterus or colon; infants born with the coil going through the upper ear; colonic-vaginal fissure (a space or track leading from the colon to the uterus, whereby E.Coli stool can be passed through the vagina); hives; abdominal pain; back pain; hysterectomy, and more. For more information about Essure, see my article on Hormones Matter.
- Adiana Tubal Ligation: It is very interesting to note that Adiana Tubal Ligation is no longer used, due to a 2012 lawsuit and judgement announced by Conceptus(R) (the developer of Essure(R) procedure), against Hologic, Inc. (4).
Hysterectomy (LAP- HYS) for Permanent Birth Control
In the USA, women over age 45 have a 40% chance of having a hysterectomy. At 70 years of age, 70% have had a hysterectomy. One study showed 50% of hysterectomies were unnecessary upon 2nd Opinion; the other found that 90% were unnecessary.
Usually, the procedure is done as a laparoscopic procedure, where little slits in the abdomen are used to push in CO2 gas, blow up the belly, and insert instruments to cut and chop the uterus out. The risks of general anesthesia include vomiting, aspiration pneumonia, death, tooth chips or tooth breaks, heart attacks, and a multitude of complications. Your specific risk factors should also be explained to you in common language. Plan to have “referred” shoulder pain to your scapula; and to wear jogging pants for weeks before your belly shrinks down to size.
Hysterectomy with Morcellation
In addition to the risks of hysterectomy and anesthesia, the morcellator adds additional risks. The morcellator is almost like a vacuum machine that follows the ‘carpet’ of the uterus in a line, while water is slurped over it. It essentially turns the uterus into one long piece to remove it. The problem with morcellation is that it spreads potentially diseased tissue throughout the abdominal cavity.
It is impossible to know if the fibroids or other uterine growths common among women undergoing hysterectomy are cancerous or otherwise diseased prior to surgery. When the morcellator is used, the risk of spreading cancer increases. What once was Stage I (baby) cancer is now Stage IV (monster) cancer all because the surgeon whizzed that morcellator throughout the abdominal cavity. For more information about problems with morcellation, read (5) and (6). The odds of having an undetected cancer may be 1:350. A newly published cohort study of 41,777 women shows there may be a link wherein younger women are less apt to have an underlying cancer before a myomectomy to remove fibroids with the morcellator, and keep the uterus intact (7). Elderly women may be at highest risk for a precancerous or a uterine cancer to be found.
Hysterectomy: What to do about the Ovaries
When considering a hysterectomy either for permanent birth control or for health issues, it is important to understand the role of the ovaries in women’s health. Some physicians will push for the prophylactic removal the ovaries under the auspices of protecting women against ovarian cancer (risk = 1.7%). The argument often includes a ‘we’ll be in there anyway; we might as well remove them’. This is not an acceptable rational for oophorectomy/ovary removal.
“Ovarian conservation” refers to the view that the ovaries belong in the pelvis, and are not to be taken out during a hysterectomy, if possible. There are risk factors for ovarian cancer in my book, so you assess your own risk at home. When considering hysterectomy with or without ovary removal, remember that this is an individual decision for each woman.
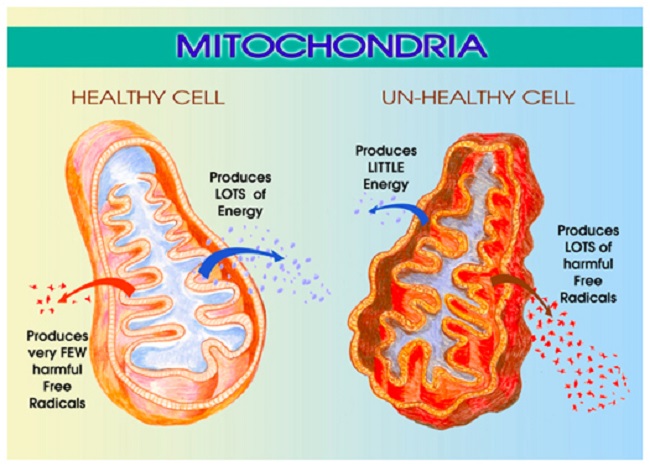
When we conserve the ovaries, hormone synthesis and secretion to continue. Ovaries can secrete hormones like estradiol, progesterone, and testosterone for up to 15 years after a hysterectomy, so ladies, they are NOT just decorations. The ovaries are an endocrine system in their own right. They protect against bone injury, fractured hips, memory loss, heart disease (America’s #1 killer), and more.
However, even with ovarian conservation, hormone issues arise. When the ovaries lose communication with the uterus as it disappears, the biofeedback loops between the uterus and the ovaries are lost. Ladies, we are living shorter lifespans for the first time in history. Men, on the other hand, are gaining lifespans. So put down that fried chicken and eat a salad. And keep your ovaries, if you can. 2nd opinion, again.
Hysterectomy with Oophorectomy (Ovariectomy; LAP-HYS with Oophorectomy)
OK, so your surgeon says you have to have “it all” taken out: uterus, both Fallopian Tubes, and both ovaries. You are at high risk for ovarian cancer, confirmed by a 2nd Opinion. After the surgery, you will be in full-on, surgical menopause, overnight.
With oophorectomy, you will be in surgical, menopausal “shock.” You don’t get 10 – 15 years for the ovaries to gradually lose their ability to secrete hormones. Nope. Just jump in a cold pool. “Surgical shock” involves hair loss, hot flashes, pain during intercourse, memory loss, depression and guilt, irritability, inability to sleep with sometimes severe insomnia, lashing out at your loved ones, decreased libido, among other symptoms. So check out the situation yourself; this is a monumental decision, not a small one. Find your Risk Factors for ovarian cancer in my book, and check off where you are. In my opinion, you should not get an oophorectomy unless you are at risk of ovarian cancer.
For me? No thanks. I’m keeping my ovaries. What if we removed testicles in men prophylactically? Do you think they would SPEAK UP? So ladies, just SPEAK UP!
Permanent Birth Control for Men: Vasectomy
One permanent birth option lays the burden upon men. Vasectomy is the surgical procedure that ties and seals the male vas deferentia, preventing sperm from reaching ejaculate, effectively preventing insemination. It is a popular method, with 15% of American men undergoing vasectomy. Its effectiveness is near 100% after a brief period of time. However, it is not without side effects. The most concerning is a correlation between vasectomy and prostate cancer. Prostate cancer is the second most common cause of death in American men, making this a Public Health issue.
Researchers here studied over 49,000 men for 24 years or less. 6,023 cases were diagnosed as prostate cancer, with 811 lethal cases. One fourth of all men had a vasectomy. Overall, the risk for men with a vasectomy having prostate cancer later on was 10%. And it wasn’t low-risk prostate cancer that was the association; it was an advanced risk of (20%) and lethal (19%), respectfully. Of men who had a regular PSA checked, a 56% chance of lethal prostate cancer was found, especially if the vasectomy was performed at a younger age (8).
To summarize this study, out of 49, 405 men studied over 24 years, 16 in 1,000 men were found to have lethal prostate cancer. Although statistically significant, it only translated to a “relatively small increase in absolute difference” for risk of prostate cancer.
There are also concerns about an increased risk of dementia in later life for men who have had a vasectomy. Though this and other risks have been disputed. So, the decision is a personal one to be discussed with the patient and a 2nd Opinion physician, weighing the risks and benefits.
The Final Decision Rests with You and Yours
Whatever you decide, do the research first and make a decision that you are comfortable with. If have already undergone permanent sterilization and suffer side effects affecting quality of life, you are not alone. Speak up and speak out so that other women can make their decisions with all of the evidence in front of them.
We cannot change the past, but we shall change the future. Our mothers wanted things to be better for us than they were for themselves…and what do we want? We want things to be better for our daughters and their daughters, too. I have a daughter. I wrote a book covering all these issues (and more) for her, because everyone thought I was going to die.
At a recent doctor’s appointment, the receptionist smiled at me not because she remembered me, but because I was still alive. My work, my book (9) is my legacy to my daughter, and therefore to you.
Still bedridden after 9 years, I am fighting to change the course of women’s healthcare. How much more can YOU do? Aim high. Persevere. And make me proud.
References
- Wikipedia: Tubal Ligation. http://en.wikipedia.org/wiki/Tubal_ligation. Last reviewed March 7, 2015.
- Mehri Jafari shobeiri and Simin AtashKholii. The risk of menstrual abnormalities after tubal sterilization: a case control study BMC Womens Health 2005 Online May 2. doi: 10.1186/1472-6874-5-5
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1112604/ Last reviewed March 7, 2015.
- Sanam Moradanand Raheb Gorbani.. Is Previous Tubal Ligation a Risk Factor for Hysterectomy because of Abnormal Uterine Bleeding? Oman Med J. 2012 Jul; 27(4): 326-328. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3464743/ Last reviewed March 7, 2015.
- Nasdaq GlobeNewswire. Conceptus ® Announces Settlement of Patent Infringement Lawsuit with Hologic. Source: Conceptus, Inc. http://globenewswire.com/news-release/2012/04/30/474765/253823/en/Conceptus-R-Announces-Settlement-of-Patent-Infringement-Lawsuit-With-Hologic.html April 20, 2012. Last reviewed March 7, 2015.
- Matthew Bin Han Ong. Harvard Physician, Whose Cancer was Spread through Morcellation, Seeks to Revamp FDA Regulation of Medical Devices. The Cancer Letter. July 3, 2014. http://www.cancerletter.com/articles/20140704_1 Last reviewed March 17, 2015.
- Amy Orciari Herman. Cancer Risks from Uterine Morcellation Examined. NEJM Journal Watch. February 7, 2014. http://www.jwatch.org/fw108455/2014/02/07/cancer-risks-uterine-morcellation-examined Last reviewed March 17, 2015.
- Wright JD, et al. Use of Electric Power Morcellation and the Prevalence of Underlying Cancer in Women who Undergo Myomectomy. JAMA Oncology February 19, 2015. http://oncology.jamanetwork.com/article.aspx?articleid=2118570 Last reviewed March 17, 2015.
- Mohammad Minhaj Siddiqui, Kathryn M. Wilson, Mara M. Epstein, Jennifer R. Rider, Neil E. Martin, Meir J. Stampfer, Edward L. Giovannucci and Lorelei A. Mucci Vasectomy and Risk of Aggressive Prostate Cancer: A 24-Year Follow-Up Study. Journal of Clinical Oncology; Published online before print July 7, 2014, http://medicalxpress.com/news/2014-07-vasectomy-aggressive-prostate-cancer.html doi: 10.1200/JCO.2013.54.8446. Last reviewed March 7, 2015.
- Margaret Aranda, M.D. Archives of the Vagina: A Journey through Time. Tate Publishing, 2014. https://www.tatepublishing.com/bookstore/book.php?w=978-1-62854-116-8 Last reviewed March 18, 2015.













I had read that 1 in 3 women has a hysterectomy by age 60 and 1 in 2 by age 72 with 78% of women ages 45-64 having ovaries removed at the time of hysterectomy. Your article says “In the USA, women over age 45 have a 40% chance of having a hysterectomy. At 70 years of age, 70% have had a hysterectomy.” The 70% by age 70 sounds awfully high but I am not all that shocked by this figure based on what I have discovered about the gross overuse and profitability of hysterectomy with only 2% done for cancer. Where did you get these statistics?
Regardless of the exact figures, hysterectomy and oophorectomy (ovary removal) are grossly overused surgeries and, in almost all cases, do more harm than good.
Since no one (including ACOG who has said that 70% of hysterectomies are unnecessary) is doing anything to rein in the abusers or force informed consent, we have to educate others about the lifelong, non-reproductive functions of the uterus and ovaries. Any procedure (hysterectomy, oophorectomy, tubal sterilization, endometrial ablation) that disrupts the normal function of this system / these organs can cause permanent problems. My article here talks about ablation and how it may be more of a hysterectomy trap than alternative – http://www.hormonesmatter.com/endometrial-ablation-hysterectomy-alternative-or-trap/. I recall a woman being told by a doctor that ablation should not be done on women under age 50!