I have had some difficulty finishing full research articles during this crisis. In lieu of full articles, and in order to more fully understand some connections, I have been tweeting thoughts and hypotheses – yes, tweeting. Eventually, these snippets will become articles, but in the meantime, I thought I would share them here. I have cleaned them up a bit and added a few links where relevant, but they remain largely as they were posted on Twitter.
Reconsidering Death, Oxygen, and ATP
I was contemplating death last night, not my own per se, but the notion of death. What is death or what constitutes death? And you know what? I still land squarely at the mitochondria.
Oxygen (O2) is fundamental for life and we like to think that its absence constitutes death. While its diminishment sure makes living difficult and its absence makes life impossible, there is something more fundamental required. There is one more step below the necessity of O2.
Without ATP – O2 cannot be used.
Sit with that for a moment.
We can mechanically ventilate and force-feed O2, but if there is insufficient ATP, it will not matter.
The relationship is reciprocal, of course, without O2, there can be no ATP.
But yet still, ATP is key.
Making fueling the mitochondria the single most important thing we can do to prevent death for any disease process, but especially something like COVID.
Unfortunately, virtually every treatment in the medical armament damages mitochondria (yes that includes all pharmaceuticals) – even or perhaps especially – forced ventilation (here, here, here). That is not to say that sometimes meds or mechanical ventilation are not necessary, but only that we could do better if we considered how O2 is used and what is required for O2 saturation beyond just the mechanics.
And that we could do better if we considered the damage drugs do to that process. [For that matter, we should also be considering the damage environmental chemicals do as well.]
For O2 to be used — we need ATP.
For ATP – we need functional mitochondria.
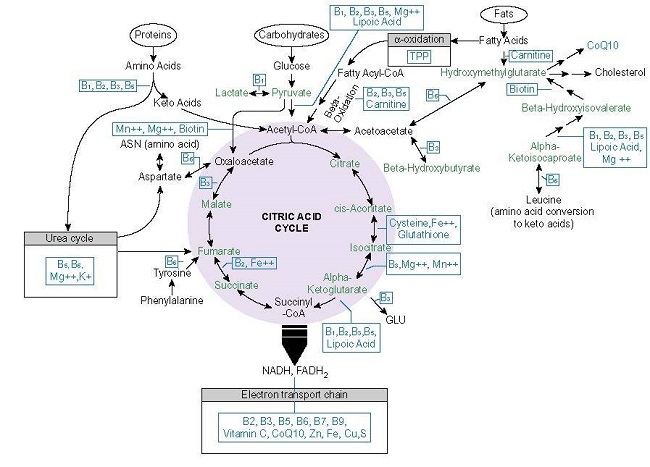
For functional mitochondria – we need micronutrients, thiamine especially. Thiamine drives the mitochondrial processing plant.
Thiamine deficiency — by itself, absent any other variables, causes hypoxia. They call it pseudohypoxia because it doesn’t match our current conceptualization of obstructive hypoxia, but it is hypoxia just the same. The only difference – it originates in the mitochondria.
From a lack of ATP, we get the inability of the mitochondria to utilize the readily available O2, which leads to more hypoxia and a crap ton of other negative sequelae. All of which we are seeing in full relief with COVID patients.
If only there was a simple solution…
Oh, that’s right, there is.
No heroics needed, just give folks IV thiamine, an IV banana bag when they come in, continue until they improve.
If they are still able to eat, throw in some protein, fat, a few carbs, and perhaps, some fat-soluble vitamins (A, D,K, for example).
To reframe – what do mitochondria need to create ATP? Nutrients plus O2.
What do mitochondria need to use O2? ATP.
So what do mitochondria need to ‘breathe’? Nutrients.
Nutrients are the missing piece in the puzzle.
Feed the mitochondria >>> prevent mitochondrial collapse >>> prevent death.
A few articles that influenced my thinking:
- Intracellular ATP is required for mitochondrial apoptotic pathways in isolated hypoxic rat cardiac myocytes.
- Extracellular ATP is a danger signal activating P2X7 receptor in a LPS mediated inflammation (ARDS/ALI).
- Purinergic Signaling in Pulmonary Inflammation.
- Mitochondrial Dysfunction as Substrate for Arrhythmogenic Cardiomyopathy: A Search for New Disease Mechanisms.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.













My 17yo daughter was also recently very ill for 2 weeks with a viral pneumonia – possibly COVID-19. She has a very noticeable reaction to low thiamine emotionally, becoming overwhelmingly sad. After the fever dissipated she told me, crying, that she couldn’t understand why she was better but so miserable. Increasing her dose of thiamine helped within a few days, although she still has low energy and tires quickly.
I know Magnesium is important but she experienced a severe return of anxiety symptoms when she tried adding it, especially waking at night with a racing heart, which thiamine had given her relief from. We tried mg citrate with l-taurine, 136mg-45mg. Is there a better form?
Mag glycinate or taurate perhaps?
Possibly also a CA/Mg combo. An imbalance between the two and affect some folks -myself included. I use Cal/Mag 2:1 from pure encapsulations. It’s a 3 dose regimen but I only take 1 per/day. I react to mag alone as well. I also use a chelated zinc/copper combo because I need the zinc and ca/mg/zinc work together.
Rachel – I do well with magnesium, but badly with all forms of citrate (I’m not entirely sure why). Transdermal mag chloride might be another option to try.
Yes I agree it should also be used preventatively and also afterwards. I now give it to my son every day and I have taken it for several years. I have my 86-year-old mother, who lives in central London, on vitamins C and D and zinc. I think I will add thiamine to the mix too. I am glad your mother recovered. Which nutrients, other than thiamine, did you give her?
Yes, on the preventative. She had been on thiamin since the sepsis as well as a mg, vitamin D and multi. We doubled her normal thiamine dose when she became ill. Added vitamin A, zinc and copper, 2-3 grams of vitamin C per day when she was ill. Also used NAC for the first time, which may have helped with her lung function, that or the vitamin A. I am not sure. She has since stopped taking NAC because it makes her feel nauseous. She still has a residual cough though. I suspect that will linger for a while but otherwise, she is doing well.
I have heard that NAC can be effective, but have never used it. I sometimes worry about taxing the liver too much, especially when people are weak… I also gave vitamin A. Anyway, thank you – I’m very reassured to have heard your point of view and experience!
Yeah, I was wary of it too and hesitant to use it, but I knew we were on our own and if she progressed to need hospitalization, she would probably not make it. I was determined to keep her out of the hospital at all costs.
It seemed to help during the height of her illness and she didn’t report any reactions to it until she began to recover. I used the lowest dose too – 500mg. Some folks suggest a much higher dose.
One other thing I did and do every time she becomes ill, is to keep her protein levels up. Like most older folks and like anyone who is ill, she doesn’t want to eat. Protein is critical to prevent muscle catabolism which will drive metabolic dysfunction. So protein drinks are a part the protocol whenever she is ill. That and I make sure every bite/swallow of food is as nutritionally dense as I can make it.
Yes I agree protein is super important before, during and after. I also read that the virus tanks potassium levels and, as my son was having violent night sweats and prone to electrolyte imbalance as it is, I gave him an electrolyte solution during and afterwards while recuperating. Also, this is possibly beneficial as potassium thins mucous? I am a little unclear as to whether the potassium loss is due to the effects of the virus itself, or the high fever…
Great article nonetheless. Dr Paul Marik or EVMS uses thiamine in bis Covid-19 protocol (https://drive.google.com/file/d/1xMlgEte6jgEzuTeB2W5zQIy_KlEzWWbH/view).
My 17-year-old son recently had the virus and I gave him high dose vitamin C, D3, zinc and thiamine and he recovered within a week.
I am familiar with protocol. My only problem with it is that he waits until the symptoms progress to add the thiamine. I think it should be used from the beginning as with other nutrients, the first sign of symptoms. I am glad your son recovered. I used nutrients, thiamine top among them, to get my 76 year old mother with pre-existing conditions through this. It took a bit longer though – 2.5 weeks. First week was horrible, she was quite ill, but throughout, her energy remained observably stable, which I took as a sign that her body was successfully fighting it. About 5 years prior, also used nutrients – IV in that case, to help her beat sepsis.
Chandler, thank you for these musings – very helpful even without being the normal kind of article. Are you able to share what brand of multi your mother uses? I’m looking for a decent multi (for my similar-aged mother, as it happens) but am struggling to find something that I think is any good.
This may be of no relevance in her situation, but post-viral residual coughs in my household (not COVID) have at least sometimes been caused by increased need for either molybdenum or manganese, and have cleared up straight away by giving more of one of those minerals. I know there are a couple of studies on PubMed suggesting that manganese increases thiamine pyrophosphate (as opposed to free thiamine) levels, and I believe that Mo deficiency might negatively affect thiamine levels by leading to elevated levels of sulfite – so it could conceivably be that there is an interaction going on there.
https://www.ncbi.nlm.nih.gov/pubmed/7376556
I can’t find the abstract for the other study; it might have been this one, but I’m not entirely sure:
https://www.ncbi.nlm.nih.gov/pubmed/13951062
I will look into to those minerals. It is so difficult to maintain my mother’s vitamin and mineral stores, she doesn’t eat very well, that I wouldn’t be surprised if there aren’t other deficiencies floating around. As far as multi-vitamin, you’ll laugh, but with her I have to use the airborne fizzies. She hates taking ‘pills’, is particular about taste, and has great difficulty swallowing big vitamins, so liquid is what we have to do. Those are not the best quality, but she will tolerate the taste of those and the gummies. Too much sugar as far as I am concerned, but I do what I can within the constraints of her willingness to do any of this. I use a brand called Whole Earth & Sea, Women’s 50+ multivitamin, myself, if that helps.
Thank you very much for taking the time to reply, Chandler: much appreciated.