Four years ago, I was very ill with disabling digestive symptoms that proved to be a mystery to my doctors and me. I had round-the-clock nausea, vomiting, abdominal pain, and rapid weight loss. It got so bad I lost my job, had to get a feeding tube, and could barely care for my children. My doctors were baffled, but worse, they implied my symptoms were all in my head or from a postpartum syndrome. My family and I, however, knew better.
I refused to give up or settle for a mediocre doctor’s easy way out of blaming the patient for her symptoms. I searched high and low and had to travel halfway across the United States, but I found a doctor who ultimately diagnosed me with Sphincter of Oddi dysfunction (SOD). Though I had a diagnosis, what followed was a series of failed treatments, near death experiences, and treatment-related complications. Today, thankfully, I am doing well.
What is Sphincter of Oddi Dysfunction?
SOD is not easily explained by its title, nor is one definition agreed upon in scientific circles. Essentially, SOD is the result of the biliary and pancreatic sphincters malfunctioning and is most prevalent in women who had their gallbladders removed. The hallmark symptom is pain under the right rib cage that may radiate to the back and shoulder, but nausea is also a frequent complaint. Many women go undiagnosed or untreated due to the fact many GI doctors are ill-equipped to recognize the disease or refuse to believe it exists.
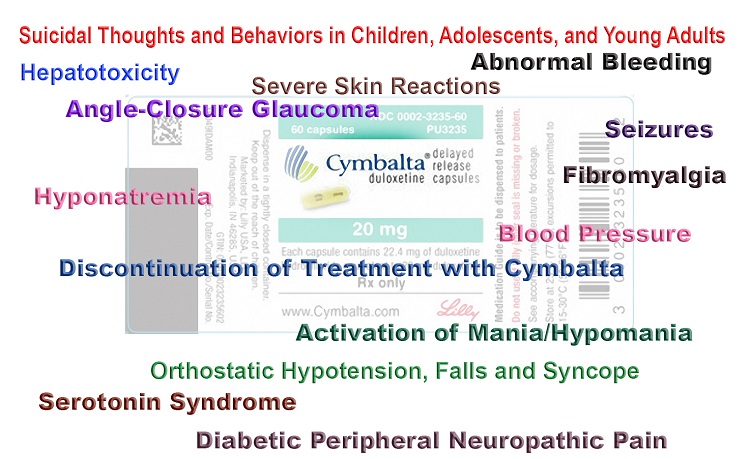
Minimal research has been conducted to find a cure for Sphincter of Oddi dysfunction. It would seem logical to research hormonal effects with SOD since it primarily affects women. However, that would be too logical for today’s gastroenterology researchers. Instead, they focus on research aimed at cutting the sphincter up (sphincterotomy) or antidepressants. Most recent research focuses on trying to disprove SOD as a valid condition, giving GI doctors the green light to abandon their mostly female patients afflicted with this condition. It is impossible to claim the biliary and pancreatic sphincters are the only body part free from dysfunction.
The Birth of a Book
At the beginning of my journey, I found few patient-friendly resources on SOD. The only book about SOD I could find was a textbook written in 1976. I could not even locate a brochure about SOD. All of the information I did happen to find on the Internet was written in research or medical jargon. Luckily, I am fairly intelligent and could decipher the big words and confusing lingo. However, I often thought how terrible it must be for patients having difficulty interpreting it all, who were desperate for information about their condition.
About a year ago, I started writing articles and blogs about SOD, including one published on Hormones Matter. It was clear to me that a book needed to be written about SOD after seeing the numerous comments from readers and number of “hits” each post received. I wished there had been more resources when I was searching for answers. Therefore, I began writing a book.
I wrote and wrote and wrote—day and night. Before I knew it, I had written an actual book, The Sphincter of Oddi Dysfunction Survival Guide. It wasn’t difficult because all of the content I had was in my head, from experience and extensive research. Along the way, I had discovered the most helpful SOD information out there did not exist on a website or in a book. It did not come from my doctors either. The best information I gathered on SOD was from fellow SOD sufferers.
The resulting guide is a compendium of my and other SOD patients’ personal experiences with trying to find a diagnosis, obtain treatment, and develop coping strategies. I also included a good amount of information regarding the science behind SOD, which I tried my best to decipher into laymen’s terms. I also discussed the need for research and for doctors to stop blaming patients for their symptoms.
It is my hope that GI doctors, primary care physicians, naturopaths and functional medicine practitioners will read this book as most need to be educated about this condition. From my experience, SOD patients know more about their disease and treatments than their doctors. We need to change that.
Writing this book reminded me of the old saying, “When life gives you lemons, make lemonade.” I encourage anyone reading this to do the same. You’d be surprised how easy it is to write and publish a book these days.










Hi, I am interested in purchasing your book, I dont have a diagnosis yet, however I do have elevated liver enzymes and the URQ pain, similar to that of what I had before cholecystectomy. I also had acute pancreatitis and they never figured out why. I have a whole slew of digestive issues still and chronic fatigue. I am wondering if the book or you have any insight on whether it would be common with this condition to also have a very high vitamin b12 level?
where can you get the book? my mom has had SOD III for 15+ years and is suffering terribly with chronic and acute pancreatitus. i would love to get this for her!
Just ordered your book. No diagnosis but I’m having the same pains and slightly elevated liver enzyme but only 1 enzyme. Had my gallbladder removed in 2011 no pain all good then after one baby 2015 was horrible. Pain almost daily then weekly. My “specialist” doesn’t believe in SOD and my text results all show normal. My question to Brooke is where do you go for help? I’m in Canada our health care is free but waiting for anything takes months if not years. I’m 31 looking at weekly pain is a scary thought
Yup… gallbladder out when I was 21. For 22 years I suffered On and off with excruciating abdominal pain in and out of the hospitals
hundreds and hundreds of times blood tests normal MRI was normal CT scans normal endoscopies normal – I probably seen you over 60 gastroenterologists during that time and eventually I was told it was in my head..
Many years later I got lucky in the hospital again with that same excruciating pain crying my eyes out finally my liver enzymes and pancreatic enzymes are highly elevated they told me to stop drinking alcohol never drink alcohol my entire life finally a doctor diagnosed me with sphincter of Odie disorder… nobody knew about it no one heard about it people are clueless about it I was the freaking weirdo with sphincter of Odie disorder what the hell was that ?
Now I’m 52 years old and sphincter of Odie want to get is bothering me . Years ago it was ballooned out and it helped for a long time however I’m not doing that again I’m afraid of pancreatitis…Still having pain…
It sucks it stinks and sometimes I want to scream!?????????
Brooke,
Thank you so much for writing this. I have just been diagnosed with SOD, last week, and I am extremely new to the term and the dysfunction. In the last 6 weeks, I have been to the ER 3x and have seen countless specialists. I have had nausea, vomiting, terrible abdominal pain, not being able to hold food down, etc. It’s been pure misery. I have missed so many days of work. It’s been mentally and physically exhausting and the Dr’s there for a while did not seem to take me seriously. I was seen for a colonoscopy and endoscopy and they did not find anything. This same episode happened about 10 years ago..I was in and out of the ER for 6 months with a failed diagnosis. Although, it’s nice to finally have some answers, I have a lot to learn about this dysfunction. I am going to keep up with your blogs going forward. Have you been able to determine what foods trigger this or what things make the pain better or makes it subside? Right now I’m on a few meds that seem to be helping….
Thanks again!
In my book I have a chapter on diet and trigger foods. I recommend you check it out: http://www.sodae.org/sod-book.html. I am so sorry this is happening to you. SOD is just awful, mostly because of the way medical professionals treat us. I hope you find one who is compassionate and helpful. Glad you found some meds that help. That is a good sign. Read my book and explore the natural remedies chapter. Take care.
Thank you for writing this book. I’ve been sick since December of 2001 with severe abdominal pain, nausea, vomiting, and diarrhea. I was diagnosed with colitis in 2005. In 2009 I was diagnosed with pancreatitis. In 2011 I had to have an appendectomy. In 2013 I had my gallbladder out. In 2013 I was suspected to have Crohn’s, I had some blood work done to see if I had Crohns or ulcerative colitis and the blood work came back showing it was Crohns. I then had a colonoscopy and the Dr could not find any Inflammatory Bowel Disease but started treating me for it because I was presenting with all of the symptoms. I wasn’t getting any better and I went through test after test and I was getting told it was all in my head and I needed to see a Psychiatrist, although I did show to have chronic pancreatitis in the head of my pancreas after a biopsy. I could not keep anything down for an entire month and was not getting any help from my local doctors. So I sought out a hospital in Beverly Hills called Cedars Sinai and an expert in SOD named Dr Simon Lo. A friend of mine was having similar issues and he helped her. This Dr was the most knowledgeable Dr I’d ever seen. He did an ERCP and found that I have papillary stenosis did a sphincterotomy placed a stint in my common bile duct and one in my pancreatic duct and placed a feeding tube. I’ve had the feeding tube for two years on August 17 2016. I’m still craving knowledge about the disease.
I am so sorry you have sick with all these digestive ailments. You must be a very strong woman! I hope you enjoy the book and gain helpful information. One thing I regret about the book is not writing more about when I had the feeding tube. It brought a whole host of issues and I frequently ended up in the ER or hospital to fix it. I also had to try several different formulas. I kept telling my doctor I thought my headaches were from a casein protein sensitivity. They refused to listen but sure as heck when they changed to a whey formulation with no casein, my headaches stopped! I hope the ERCP brings you lasting relief. Be careful if you get acute pancreatitis with ERCPs because the more times you get AP the more damage it does to your sensitive pancreas. Try the natural remedies, diet, and medications. Good luck!