I am sharing my health story in the hopes that someone can offer assistance. I had stage 4 endometriosis for years before it was diagnosed. On top of that, I have had reactions in antibiotics, including fluoroquinolones and was given Lupron. Each drug destroyed more of my health. I am currently bedridden, in pain and unable to function. I have lost hearing in my right ear, have Sjögren’s syndrome, Hashimoto’s, adrenal insufficiency, hypokalemia, electrolyte imbalances, IBS, MCS, Ocular migraines and recently, have been diagnosed with dysautonomia. My body feels like it is disintegrating. We believe that everything is related, that I have mitochondrial issues at the root of these illnesses, but to date, no one has been able to put the pieces together. With the help of my husband, I have put together my health history. We are looking for input.
Early Warning Signs
1985: late summer, I was hit by car while riding bicycle. I was banged up really bad and definitely had head injury.
1998: started feeling off, not sure yet at this point still very young
2001: birth of my first daughter. I developed severe preeclampsia and had an emergency C-section three days later. My daughter was 6 weeks early and spent two weeks in the intensive care unit.
2002-2003: I felt off at times and did go to GP on several occasions. I had pain shot to my back. I am not sure what it was but it took the pain away. I also kept saying just didn’t feel well. I felt off but nothing was found.
2005: the birth of our son and second C-section. I was on bed rest last three months of the pregnancy. I was given an antibiotic for some reason. I do not remember. I had a reaction to it and turned orange. The doctor gave me something else to counter the effects of the antibiotic and my color returned to normal. It was a normal birth.
2006-2007: I was still in pain. The pain moved to the abdominal area. I developed bowel issues, had and ovarian cyst. I saw gastrointestinal physician who did scans and found a thickening of the lining of uterus. He referred us back to the gynecologist who did D&C in 2007 and said I had very minuscule amount of endometriosis.
2008- 2009: still seeing OB for pelvic pain, also seeing multiple other doctors including a neurologist, internist, and surgeon. Everyone kept saying same thing: ‘Your fine. It’s in your head.” They wanted to put me on mood enhancers. I tried lorazepam and felt terrible on it, so I stopped after two weeks.
The Lupron Disaster
September 2009: I started doing Lupron injections from gynecologist. She was very forceful with me and stated “if you don’t do these injections I can’t help you.” She said it was the only way they could know if the pain was below the belly or above. I agreed reluctantly, but at that time still thought my doctors had their best interests in me. After the first injection, my doctor called at home on a Saturday to see how I was feeling. I responded I was already in pain, but it has now quadrupled and I feel like an old person. Every bone in my body hurt. I couldn’t believe the amount of pain I was in. She said I had to get all 6 injections if it were to be able to help me.
At that time, my husband because of work only went to a few of my appointments. I soon began to have him go with me because I felt I was getting the run around.
Hearing Loss Post-Lupron: Let’s Add Fluoroquinolones and Steroids to the Mix
2010: the last injection was in February. I began to lose my hair. I had memory loss, stabbing and taser sensations in head. I was still getting pains in abdomen area. In September, I went in for ear pain. The ENT said it looked like a scratch, so he gave me fluoroquinolone drops. I had also taken other fluoroquinolone antibiotics for yeast infections earlier in the year. In October, I had sudden sensorineural hearing loss in the right ear. Within an hour, I called my husband told him my hearing was acting weird. I went totally deaf in my right ear, 8 months after my last injection of Lupron. My local ENT immediately gave me a shot of cortisone (I was able to still walk and drive). It all went crazy when my ENT put me on a large dose of oral prednisone for 14 days. Everything in my body went nuts. I was rolling out of bed, holding on to the walls to help me walk. I totally lost my balance. The oral prednisone really did a number on my head. I had done genetic testing through 23andMe and our doctor upload the report to a reader called Opus23. It said that I should never take prednisone.
I went to Stanford Medical and saw top ENT and received three cortisone injections into the right ear drum. Had a 50/50 chance for recovery and for me it didn’t work. I left Stanford with them telling me they still don’t have all the answers yet when it comes to sudden hearing loss. They thought it was some sort of viral infection that attacked the ear drum and deafened the ear. After the hearing loss. I had three ER visits. This is when I first started having low potassium. I felt like I was about to pass out. I was still driving at this time, I didn’t know what to think.
2011 -2012: I began seeing a naturopathic physician. I also did a trip down to LA to the House Ear clinic to see some specialist regarding her hearing loss. They couldn’t help either. I left my current OB and started seeing the physician who was filling in. I ended up doing a partial hysterectomy with her after finding a growth at one of my numerous ER visits that year. I was still working and a full-time mommy, while dealing with massive pain in my lower abdomen and now starting to deal with multiple autoimmune diseases including: Sjögren’s syndrome, Hashimoto’s, adrenal insufficiency. In addition, a lot of my minerals and vitamins were off at that time. I suspect this was beginning of my dysautonomia. I also began seeing an endometriosis specialist at Stanford.
Was it Endometriosis All Along?
2013: On January 31st, I had laparoscopic surgery to clear the endometriosis. I had stage 4 endometriosis which took my appendix. The physician said my body was littered with endometriosis. He even checked up in my heart cavity to make sure no endometriosis had made its way up to the heart. Before the surgery, I was talking with the anesthesiologist and telling him about my hearing loss and my low potassium. That is when he stopped the surgery and I had to take a stress test. We left and went to Palo Alto heart center and did a stress test I fasted for 24 hours and then they had me go do a stress test on a treadmill on an empty stomach. I did it no problem and went back to the surgery center. That is when they did the laparoscopic surgery and found stage 4 endometriosis.
Also, I want to point out that we didn’t find out until much later that during the course of the endometriosis surgery, they had left surgical clips and suturing material in me. We discovered this at one of our many ER visits. The OR report from our doctor says nothing about these things being left inside of me. I believe this is an additional pain I have on top of the other complications in my abdomen area. Nothing like having a wad of surgical clips throughout my abdomen and suturing material left inside my already struggling body. We are trying to get these removed, but no surgeon will take my case.
Mitochondrial Damage and Autonomic Disintegration
April that year, I had another ER visit. I lost all bodily functions. My potassium was severely low. I would go to the ER in 2013 many more times.
2014: I had to stop working totally this year. I tried to come back and assist a friend of mine just being her loan officer assistant but the neurological pains and crazy foggy brain I was experiencing was just too much. Something that was so easy for me years earlier, I was now having trouble just doing basic loan officer task at this point. Strange neurological pains were becoming a normal. I stopped driving this year also. It was just getting to scary for me to continue. I continued to go to ER for multiple visits
2014- 2017: I went to the ER over 50 times for various reasons: heart pains, chest pains, shooting stabbing pains throughout my entire body. I almost always had low potassium. Over these years, we spent our life savings and pulled out a $100,000 from my husband’s 401k, which we spent on various treatment plans. We have traveled as far away to Philadelphia looking for answers. We even gutted our house when we were told at one time it must be mold that is killing me. We lived in a borrowed 5th wheel while my husband put our house back together. There have been numerous days where I felt I couldn’t go on one more minute. I felt like death was right around the corner.
In 2015 one of our doctors after reading my genetic report thought he found a breakthrough with a patient that had hypokalemia and Sjogren’s syndrome. He provided me a copy of the study they did on a girl with very similar symptoms to mine. He had our local compounding pharmacy mix a solution called Shohl’s. I took the solution after my doctor assured me I would be ok. Well, I tried it almost within in minutes I was convulsing and went into tachycardia. My husband called 911 ambulance took me to the ER. In route to hospital paramedic gave me nitroglycerin. I was monitored for several hours and eventually went home. During this time had been staying at my mother-in-law’s house for about 6 months because we weren’t sure at this point if something in our house was making me so sick. This was a very stressful time for me at this point we have no idea what’s going on and what’s causing this.
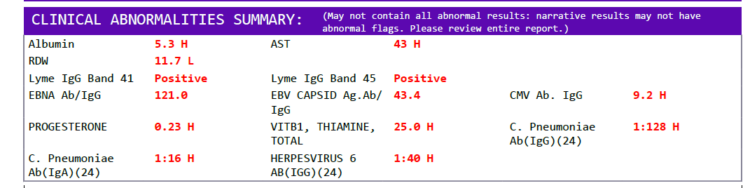
We did have some relief in 2017 when our local naturopathic doctor was able to get a new treatment called UBL or ultraviolet blood irradiation. I had about 6 months where I was feeling off, but having somewhat good days where I could semi-function. My viral count has been very high during these years, EBV, CMV, HHV6, etc., and possibly Lyme. If I push myself, I will crash for hours sometimes days until I start to get any strength back just to walk to the restroom.
Next, I went in for a completely different treatment called prolotherapy. I got one injection into my shoulder, and just like that my body reverted back to like I was before the UBL treatments. I was worse again. It was very strange my body reacted like that.
2016: I was diagnosed with dysautonomia by another specialist, an electrophysiologist cardiologist. I have several of the sub symptoms of dysautonomia including: postural orthostatic tachycardia syndrome (POTS), neurocardiogenic syncope (NCS), dizziness, vertigo, fainting, fast, slow or irregular heartbeat, chest pain, low blood pressure, problems with gastrointestinal system, nausea, disturbances in visual field, weakness, breathing difficulties, mood swings, anxiety, fatigue and intolerance to exercise, migraines, disrupted sleep patterns, temperature regulation problems, concentration and memory problem, poor appetite and overactive sense, especially when exposed to noise and light. We also met with a dozen or so other specialists. None were able to help.
I have multiple tears in both hips worse on right side. Multiple torn areas in the pelvic floor also. Surgery is out of pocket and we have not been able to fly back and have surgery to repair those tears and hips yet as of 2019.
2018- 2019: I went to the ER only three times in 2018 and so far only three times in 2019. We try not to go because we know they never find much. I only go to be reassured that my vitals are still strong when I’m feeling at my worst. I have been denied disability. I had a neurocardiogenic seizure in the courtroom with judge and she still denied me. I have one last appeal that I am waiting on. I am not very hopeful that will go through. At this point, the dysautonomia, fibromyalgia/ chronic neurological pain and the low potassium are what are the hardest things for me to deal with. As of right now, we are concentrating on rebuilding my mitochondrial cells in hoping I can reverse some or most of the damage I think was a direct cause from the Lupron injections.
I was also on bio-identical progesterone creme from around 2012 to 2018. Then, in middle of 2018, my ND wanted me to try the bio-identical that went off the lunar moon cycle. It was a separate estrogen and progesterone creme in a plastic push-up type applicator. She said she was looking into it and thought it might help. Well, I tried it and had terrible side effects, I think most likely from the adding in the estrogen. After second month, I was having terrible stomach pains. I looked four months pregnant and was begging my husband to take me to the ER. The pain was worst at the part of the cycle where I took the estrogen only. I felt like she was going to die. In the past, I was always high in estrogen. I am not sure, but as soon as I introduced in that estrogen, it threw me out of whack terribly. I stopped that in November of 2018.
This is where I am now: in pain, unable to work or care for my children. My husband is my full-time caregiver. He takes care of our kids, shops cooks, does everything I used to do plus works his full-time job. I couldn’t do this without him. The doctors have run out answers. I believe it was the endometriosis all along, made infinitely worse by Lupron and the various rounds of antibiotics, including fluoroquinolones. The only way I can maintain my potassium levels is through huge daily doses. Otherwise, I slide into hypokalemia. We have a standing order at our local hospital to measure my potassium whenever I suspect it is low. We have sought treatment from dozens of specialists and spent our entire life savings and I am no better than I was 10 years ago. In fact, I am worse. Over the last 8 years, we have been supplementing with vitamins and minerals to try and repair the damage done to my mitochondria by the Lupron and the fluoroquinolones. Some things help and others do not. We are at wits end and do not know where to turn for help. Below is a list of supplements that I currently take.
Supplement List
Upon waking:
- 600mg potassium,
- 1 1/4 grain Naturethroid
Breakfast:
- 3 200mg potassium. Daily total 1200mg
- 1 Chewable Hydroxo B-12
- 1 COQ10 100MG
- 1 Biotin 10,000mcg chewable
- 1 Chromium picolinate 200mcg chewable
- 1 Desiccated adrenal from Standard process
- 1 magnesium malate 100mg
- 1 Thiamin 50mg
- 1 Mitocore – it is like a multiple vitamin
- 5 grams vitamin C, mixed with juice, plus I add Lugol’s iodine, colloidal silver, lymph drain and trace mineral mix.
Mid-morning:
- 3 200mg potassium again – daily total 1800mg
- B12 shot, a 100iu syringe
Lunch:
- 3 200mg potassium, daily total 2400mg
- 1 vitamin A 10.000iu
- 1 vitamin K 90mcg
- 1 Lugol’s iodine plus
- 1 nettle leaf cap 400mg
- 1 Monolaurin 600mg
- 2 L-lysine 1000mg
- 1 thiamin 50mg
- 1 magnesium malate 100mg
- 1 more Hydroxo B12
Diner:
- 3 200mg potassium, daily total 3000mg
- 1 thiamin 50mg
- 1 milk thistle 150mg
- 2 L-lysine 1000mg
- 1 DHEA 25mg
- 1 magnolia bark 450mg
- 1 Digestive enzymes
- 1 Dr. Berg Hair formula.
- 1 L-carnitine 250mg
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Image: Maximum Speed of Raphael’s Madonna, Salvador Dali, 1954.
Posted originally on Aug 20, 2019.