Recent reports indicate that COVID-19 has important similarities to high-altitude sickness and high-altitude pulmonary edema (HAPE). As those of who have traveled to high altitudes know, acetazolamide (known by its trade name Diamox) is often prescribed to help prevent high-altitude sickness; doctors also use it to treat HAPE. Acetazolomide is hypothesized to work through several pathways, including the inhibition of carbonic anhydrase isoenyzmes, which induces respiration, leading to higher oxygen levels. Acetazolamide has many side effects that make it difficult to tolerate, including nausea, vomiting, and taste impairment. In vitro research shows that thiamine is also a carbonic anhydrase inhibitor (CAI) with a potency approaching acetazolamide. Thiamine has very few side effects, even in high doses, and carries the added benefit of improving mitochondrial function via a number of mechanisms.
If thiamine were distributed to individuals soon after they contract the illness, it could potentially help more people cope with COVID-19 on their own, reducing the demands on hospitals and saving lives. Because it has very few side effects, patients may be more likely to take it than acetazolamide, increasing treatment compliance. The low side effect profile of thiamine could also allow it to be administered in increased doses and with greater frequency, potentially contributing to the treatment of patients at more advanced stages of the illness.
Expedited research is needed to confirm the CAI and other relevant properties of high-dose thiamine and test whether and to what extent it can contribute to the treatment of patients affected by COVID-19.
Background: COVID-19 Resembles High-Altitude Sickness and High-Altitude Pulmonary Edema
In recent weeks, frontline physicians have begun noting similarities between COVID hypoxia and high-altitude sickness and high-altitude pulmonary edema (HAPE). For example, Dr. Cameron Kyle-Sidell, an ER doctor in New York, describes COVID-19 as
“…some kind of viral-induced disease most resembling high-altitude sickness. It is as if tens of thousands of my fellow New Yorkers are in a plane at 30,000 feet and the cabin pressure is slowly being let out.”
Another physician, Isaac Solaimanzadeh, documents in more technical terms the close resemblance of COVID-19 to HAPE. As Solaimanzadeh (2020) explains:
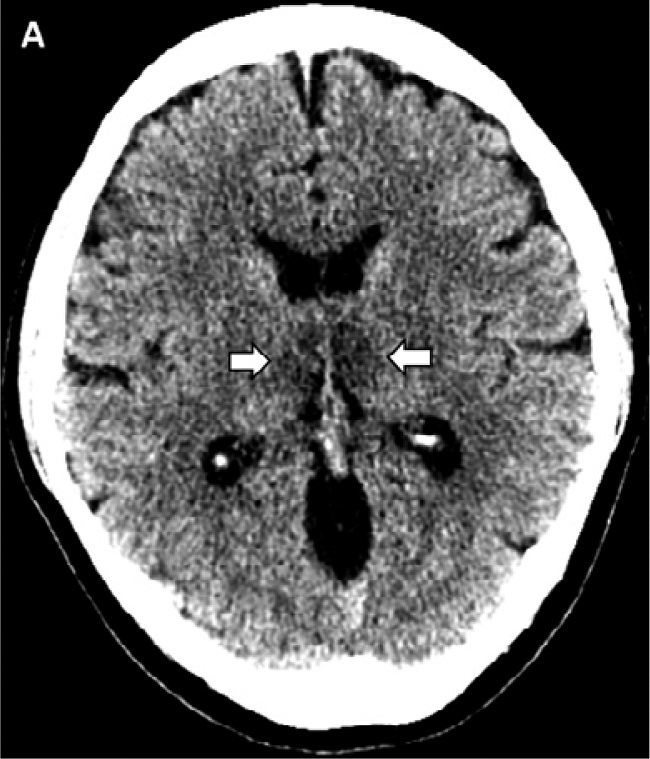
Both COVID-19 and HAPE exhibit a decreased ratio of arterial oxygen partial pressure to fractional inspired oxygen with concomitant hypoxia and tachypnea. There also appears to be a tendency for low carbon dioxide levels in both as well. Radiologic findings of ground glass opacities are present in up to 86% of patients with COVID-19 in addition to patchy infiltrates. Patients with HAPE also exhibit patchy infiltrates throughout the pulmonary fields, often in an asymmetric pattern and CT findings reveal increased lung markings and ground glass-like changes as well. Widespread ground-glass opacities are most commonly a manifestation of hydrostatic pulmonary edema. Similarly, elevated fibrinogen levels in both conditions are likely an epiphenomenon of edema formation rather than coagulation activation. Autopsy results of a COVID-19 fatality revealed bilateral diffuse alveolar damage associated with pulmonary edema, pro-inflammatory concentrates, and indications of early-phase acute respiratory distress syndrome (ARDS). HAPE itself is initially caused by an increase in pulmonary capillary pressure and induces altered alveolar-capillary permeability via high pulmonary artery hydrostatic pressures that lead to a protein-rich and mildly hemorrhagic edema. It appears that COVID-19 and HAPE both discretely converge on ARDS.
The CAI Acetazolamide Is Used to Prevent High-Altitude Sickness and Treat HAPE
As a note published by the Cochrane collaborative confirms, the CAI acetazolamide is effective in helping to prevent high-altitude sickness. Acetazolamide is also an important part of the treatment for HAPE. As Solaimanzadeh explains:
“Acetazolamide has a myriad of effects on different organ systems. It potently reduces hypoxic pulmonary vasoconstriction. Improved minute ventilation and expired vital capacity has been shown in climbers taking Acetazolamide as well. Furthermore, over 70% of patients with COVID-19 had elevated lactate dehydrogenase levels; this too may be connected to hypoxia. Evidently, Acetazolamide has physiologic effects that delay plasma lactate appearance with no effect on ventilatory threshold.”
In a tweet thread, Dan Arendt (2020) elaborates on the benefits of acetazolamide for COVID-19:
“Acetazolamide is a carbonic anhydrase inhibitor, [and] the inhibition of carbonic anhydrase leads to decreased hydrogen ion secretion in the renal tubule. This ultimately results in an increase in bicarbonate excretion. This excretion of bicarbonate begins to reverse a patient’s alkalosis; in addition, the decrease in bicarbonate acts as a respiratory stimulant. Remember, our respiratory drive doesn’t come from the need for oxygen, it comes from the desire to eliminate CO2. Due to the excretion of bicarbonate and sodium, we also see an overall diuresis. Additionally, a pleiotropic effect of acetazolamide is that it leads to dilation of the pulmonary vasculature, decreasing permeability and capillary leak.
Due to these pharmacologic effects, acetazolamide has been used for years as a preventative measure for mountain climbers, to stimulate their respiratory drive and improve gas exchange despite high altitudes and low FiO2. Remember, we are seeing early reports of striking similarities between the ARDS presentations of patients with altitude sickness and those with Covid.
Now let’s put this all together. Theoretically, in a COVID patient who is alkalotic and hypoxic, acetazolamide could decrease capillary leak and edema, improve gas exchange and stimulate the respiratory drive. Adding those pharmacologic effects to the proven efficacy of and oxygen therapy, may be able to correct hypoxia and stave off the need to intubate a patient. Which is especially important when the mortality rate of a ventilated covid patient is so incredibly high.”
In High Doses, Thiamine Is Likely a Carbonic Anhydrase Inhibitor
Ozdemir et al. (2013) evaluated the relative efficacy in vitro of thiamine and several other compounds, including acetazolamide, in inhibiting three of the 16 (or more) carbonic anhydrase isoenzymes. They found that thiamine had effects similar to (though not quite as strong as) acetazolamide against all three of the isoenzymes studied.[1] Smithline et al. (2012) evaluated the bioavailability of oral thiamine HCL (one of the two more common oral formulations of thiamine available) and found that it is well absorbed. As they write, “oral thiamine hydrochloride when given over a 1-week period produce[s] blood levels that approach those obtained by intramuscular and intravenous administration” (ibid.)
Commenting on the results of Ozdemir et al. (2013) and Smithline et al. (2012), one Internet forum commentator noted the following:
“The highest concentration of thiamine is required to inhibit hCA I and it is 380nM/L. This figure from a human study on the pharmacokinetics of thiamine shows that this concentration is achievable using a 1,500mg dose. The concentration[s] required to inhibit the other isoenzymes of hCA were 85nM and 62nM, which are easily achieved with a thiamine dosage of 300mg – 500mg.”
Since oral thiamine HCL has a half-life of about 3-5 hours (Smithline et al. 2012) and cerebral spinal fluid regenerates every 6-8 hours, thiamine would likely need to be administered 3-5 times per day to be of maximum effectiveness.
For more than ten years, Dr. Antonio Costantini and his colleagues in Italy have used high-dose thiamine to treat a range of neurological conditions. While they seem unaware of its CAI properties, the dosages they use (for most conditions, 600 to 1,800 mg of thiamine daily, rising to 4,000 mg of thiamine daily for Parkinson’s Disease, in divided doses) are precisely those needed to reduce cerebral spinal fluid flow in light of the findings of Ozdemir et al. (2013) and Smithline et al. (2012). As I will explain in more detail in a subsequent post, I believe carbonic anhydrase inhibition provides a plausible explanation for the outcomes Costantini and his colleagues have observed, potentially in synergy with other pathways.
Similarly, Dr. Derrick Lonsdale has used thiamine in varying doses for decades to treat a variety conditions where disrupted oxidative phosphorylation leads to many of the key variables noted in COVID-19 patients, including molecular hypoxia. Thiamine is also included in Paul Marik’s EVMS COVID-19 protocol (Marik 2020) based on his earlier experience with a combination of vitamin C, thiamine, and hydrocortisone for sepsis (Marik et al. 2017).
To determine the full potential of thiamine to substitute for acetazolamide, tests would be needed to confirm not only its CAI properties but also the extent to which it results in pulmonary vasodilation and increased blood flow to the brain.
Distribution of Thiamine Could Help People Cope With COVID-19 at Home, Reducing Demand on Hospitals
If thiamine were proven to inhibit carbonic anhydrase isoenzymes as effectively in people as it does in vitro, my suggestion would be to have patients start at home with a starting dose of thiamine before the disease reaches its more dangerous phases, and then gradually increase the dose based on certain defined markers of disease progression. Hopefully, this would help them cope at home, but if necessary, they could be transferred to a hospital, where the low side effect profile of thiamine might allow higher and more frequent doses than acetazolamide, potentially reducing the share of hospitalized patients who need to be transferred to the ICU or put on a ventilator. Given the anti-viral properties of Vitamin C (Biancatelli 2020), another safe and well-tolerated supplement, consideration should be given to including Vitamin C at all phases of the protocol.[2]
Conclusion
In conclusion, research is urgently needed into the potential of high-dose thiamine to help newly diagnosed patients cope with COVID-19 at home, reducing the demands on over-burdened hospitals. Research is also needed into whether higher and more frequent doses of a CAI like thiamine would help keep more newly hospitalized patients out of the ICU and off of ventilators. This study could and should be done on an accelerated basis to make the treatment available ASAP, if it proves effective. A proposed testing protocol is included in my working paper.
Endnotes
[1] In the text of the paper, the authors state that thiamine is more effective than acetazolamide in inhibiting the hCA I isoenzyme, but I read the table as showing that thiamine is somewhat less effective.
[2] This would obviously complicate interpretation of the results of a randomized trial, but given the crisis we are in, it may be better to test an easily distributed combined protocol first and worry later about how much each agent contributed to the results.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Image credit: Pixabay.













If you are interested in this topic, please see my September 24, 2020 update summarizing new evidence on the potential of thiamine to help reduce the severity of COVID-19.
https://www.hormonesmatter.com/thiamine-missing-piece-covid-treatment-puzzle/
For what it’s worth. I noticed a benefit from taking 100mg Benfotiamine(thiamine) twice daily when I had SARS-Cov-2 myocarditis but now after reading this article.. I should have taken more.
I was also taking other supplements for other purposes that worked with thiamine.
Jarrow formulas 1000mcg methyl B12 to produce sufficient melatonin to fall asleep and sufficient red blood cells because the SARS-cov viruses destroy red blood cells in positive blood types. I was taking 2-3 pills before bed.
New roots B-Complex + Vitamin C to cover my other minor B vitamins. Twice a day.
Naturelo Vitamin C 500mg multiple times a day.
Magnesium bisglycinate for immune system modulation and therefore prevent cytokine storm.
Natural factors resveratrol (antiviral).
Vitamin D supplement + Vitamin A(from carrots) to produce immune system cells. However I can’t eat carrots that often post viral infection since they promote clotting.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC298966/
I also noticed niacinamide/niacin made symptoms worse. So did quercetin/NAC. Quercetin would cause tachycardia and NAC would eliminate the tachycardia but NAC taken alone would lower my blood pressure too much. So I stopped taking them.
Adaptogens just lowered my immune system cells. They made symptoms worse.
Doing bodyweight squats and bench dips before bed also made sure I woke up in the morning.
Hopefully this will help those susceptible to this virus.
Thanks for the note, Andre. I hope your recovery is going well. There have been increasing reports of persistent disability following COVID-19 among some individuals that sounds similar to what people with ME/CFS have been reporting for years following severe illness. I wish there were more focus on preventing the immune system from overreacting early in the course of the illness to try to both reduce severity of COVID-19 and possibly reduce incidence of continued post-viral problems.
An interesting discussion has arisen between Jeffrey Lubell and Andrew Luks and Associates. JL argues that thiamine is a carbonic anhydrase inhibitor while AL et al. argue that HAPE treatments are inappropriate for treatment of Covid. I must point out that the overall responsibility of thiamine is the production of energy and when the high doses are being used, it is acting as a stimulator of the enzymes for which it is a catalyst. Even though AL et al. point out that in Covid patients it is a viral-mediated inflammatory response, the question remains as to the mechanism. Thiamine deficiency produces pseudo-hypoxia and the pathology is no different from true hypoxia that is the underlying cause of HAPE. It has long been known that arterial oxygen concentration in beriberi is low, while the venous oxygen concentration is relatively high. To support Lubell’s argument the arterial and venous oxygen saturations could be compared. On the other hand, high-dose thiamine has absolutely no toxicity and could be given without any risk to the patient. In the medical literature, the clinical response of high-dose thiamine has been accepted as evidence of ifs effect.
I’m with you on the Thiamine. How many of the elderly whom have passed from Covid 19 were also Thiamine deficient.
I’m also interested in non shivering thermogenesis as a potential treatment.
Currently I’m supplementing with Cod Liver oil to provide vitamins A and D. Vitamin A Upregulates Uncoupling Proteins whilst Vitamin D suppresses them.
I’ve added omega three fish oils for fuel.
Acetyl l Carnitine to provide Acetic acid for acetylcholine production and Carnitine to shuttle the fatty acids.
As hypokalaemia due to urinary excretion leads to fatality I’m taking magnesium to hold onto potassium from fruit juice.
In addition to this I’ve been taking Thiamine 250 mg a couple of times a week.
I additionally think alpha2 adrenergic agonists such as clonidine or Guanfacine have use as a treatment to prevent the cytokine storm.
Smokers may have some protection as nicotine induces browning of adipose tissue.
In 2018 when they found 6 new Corona virus samples in Myanmar, most was found in guano or bat shit rather than nasal or rectal swabs!
Dr. Lonsdale,
Do you think the “ground glass opacities” are oxalates?
I believe that the missing link in offering thiamine treatment is that immunity is controlled by the parasympathetic vagus nerve through the spleen. It requires acetyl choline as its neurotransmitter. The acetylation of choline depends on function of the citric acid cycle that is dependent on thiamine oxidizing glucose. Thiamine can be given in megadoses and has no toxicity by mouth or I/V. There is evidence that thiamine deficiency is precipitated by any serious illness.
Thank you for highlighting this point, Dr. Lonsdale. I’ve included below three links for readers who wish to access more information on the points you raise. Please feel free to suggest other links that might be helpful.
https://www.hormonesmatter.com/energy-loss-cause-disease/
https://www.hormonesmatter.com/mitochondria-energy-not-genetics-underlies-health-disease/
https://www.amazon.com/Thiamine-Deficiency-Disease-Dysautonomia-Malnutrition-ebook/dp/B073NCFNLX/
Since this blog was posted, a number of doctors have released a rebuttal to Solaimanzadeh, arguing that lung injury from COVID-19 is different from that of HAPE in important ways. See https://www.liebertpub.com/doi/pdf/10.1089/ham.2020.0055 . They argue that the HAPE treatments nifedipine and sildenafil are inappropriate for COVID-19. They do not address the applicability of acetazolamide to COVID-19, however, which was the primary adjunctive treatment recommended by Solaimanzadeh and the one I focus on in my blog post.
The debate about how best to treat the illness once patients become critically ill is extremely important, but ultimately beyond the scope of my recommendations. My proposed treatment protocol focuses on adjunctive therapy to help patients cope with the disease on their own, reducing the need for hospitalization and admission to the ICU. I do not know and offer no hypothesis as to whether thiamine would be useful for treating critically ill patients once they enter the ICU. I have added language to my working paper to make this point clear.
My updated working paper is available at the same link: https://docs.google.com/document/d/1vnYosVsgChnGVecOXp96T5i2UibTsnHVaDUVF6Us2uM/edit?usp=sharing
.
Dr Marik’s protocol includes IV thiamine: https://www.evms.edu/covid-19/medical_information_resources/
Yes, likely based on Dr. Marik’s experience using Vitamin C and thiamine for sepsis, as reflected in his 2017 study. There have been a number of studies since then, with mixed findings. I cite and very briefly discuss the studies in the working paper cited at the very end of this post. I don’t dwell more on this literature because I’m focused on a different hypothesis for how thiamine could help patients with COVID-19.