Yes. While endometriosis typically develops on the pelvic structures including rectovaginal septum, bladder, bowels, intestines, ovaries and fallopian tubes, it has also been found in uncommon/distant regions including nervous system, rectus abdominis muscle (“abs”), lungs (where it can induce Catamenial Pneumothorax), and even rarely, the brain. The ovaries are among the most common of locations, with the gastrointestinal tract, urinary tract and soft tissues following1 – but even disease as far remote as the gastrocnemius (calf muscle) has been documented in the literature.
Symptoms of Endometriosis
Symptoms of endometriosis, in general, do vary considerably, and may mimic those of similar conditions like pelvic inflammatory disease or pelvic infection (but remember, endometriosis itself is NEVER an infection!), ovarian torsion, adenomyosis, fibroids or even ovarian cancer. Classic signs include severe dysmenorrhea (painful periods are NOT the same as endometriosis!), deep dyspareunia (pain associated with sex), infertility/pregnancy loss, chronic pelvic pain, Middleschmertz (painful ovulation) and cyclical or perimenstrual symptoms, and the disease may present as bowel obstruction, melena (bloody stool), hematuria (bloody urine), dysuria (painful urination), dyspnea when the diaphragm or lungs are affected (shortness of breath), and swelling in soft tissues. Degree of disease present (“stage” of endometriosis; 1-4 based on severity) has no correlation with severity of pain or symptomatic impairment.
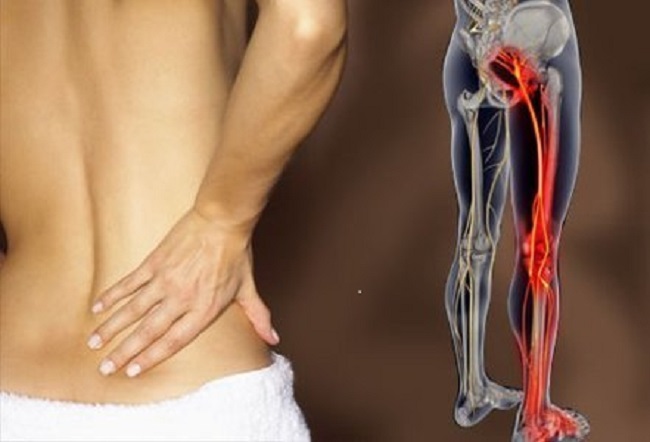
Extrapelvic and Sciatic Endometriosis
Extrapelvic endometriosis certainly does exist, with just a few references to such noted above; indeed, these diagnoses are becoming even more prevalent. This increased recognition may be in part due to the practitioner’s own improved understanding of the disease, and/or to the patient’s active role in her own care: speaking up and making herself heard about new or different symptoms she is experiencing and insisting on proper, authoritative treatment. To that end, one consideration for some patients who may present with specific symptoms is sciatic endometriosis.
Sciatic endometriosis is not abundantly common – but it should always be included in the diagnostic approach to pain and symptoms affecting the sciatic nerve distribution.

The first case of biopsy-confirmed sciatic endometriosis was described by Denton & Sherill in 1955.3 Since then, many additional cases have appeared in the literature. Symptoms that may lead to suspicion of sciatic disease may be predominantly left-sided, though infiltration of the pelvic wall and somatic nerves causing severe neuropathic symptoms due to endometriosis infiltrating the right sciatic nerve has also been well-documented.4
Diagnosing Sciatic Endometriosis
Pain may begin just before menstruation and last several days after end of flow and be accompanied by motor deficits, low back discomfort radiating to the leg, foot drop, gait disorder due to sciatic musculature weakness, cramping and/or numbness radiating down the leg, often when – but not limited to – walking, especially long distances, and tenderness of the sciatic notch. There may also be positive Lasègue’s Sign (an indication of lumbar root or sciatic nerve irritation in which “dorsiflexion of the ankle of an individual lying supine with the hip flexed causes pain or muscle spasm in the posterior thigh” [Kosteljanetz et al.]). There is almost always a history of pelvic endometriosis.
Left untreated, sciatic endometriosis may presumably cause nerve damage through cyclical inflammation and advance “aggressively” to the epineurium and perineurium.5
Unchecked, symptoms will likely lose their cyclical nature with time, due to scarring, resulting in progressively shorter pain-free intervals until constant pain prevails.6
Physical examination may reveal various neurological deficits involving the sciatic nerve rootlets. There may be localized tenderness over the sciatic notch, but this is not a classical finding [Ellias et al.]. Pelvic examination may also even be normal. The disease can be seen on imaging tests in some cases,7 though ultimately a visual (surgical) diagnosis is indicated. Early diagnosis and treatment is indeed critical in order to minimize the damage caused by the recurrent cycles of bleeding and fibrosis, characteristics of endometriosis.8 While sacral radiculopathies (pudendal, gluteal pain), vascular entrapment or sciatic neuralgia may be at the root of symptoms for some women, in patients with sciatica of unknown genesis and/or suspicion of pathology such as endometriosis, laparoscopic exploration of the sacral plexus and/or sciatic nerve is advisable.9
Sciatic Endometriosis Treatment
Sciatic endometriosis is generally treated the same way as pelvic disease: preferably gold-standard surgical eradication (excision). When not possible, a course of medical therapy may suppress symptoms until such time as the patient can receive proper surgical intervention with a skilled, minimally invasive pelvic surgeon who has vast experience in highly complex cases of endometriosis.
It is very important to understand that not every patient with symptoms relating to the lumbosacral plexus or proximal sciatic nerve bundle will actually have sciatic endometriosis, as there can be several differential diagnoses. However – endometriosis can be a real (albeit, less common) cause of nerve injury and symptomology.10 This extrapelvic manifestation of the disease must be considered in the differential diagnosis of women and girls with symptomatic presentation, particularly if a history of endometriosis or chronic pelvic pain is present.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
References
- Woodward, Sohaey, Mezzetti. Endometriosis: Radiologic-Pathologic Correlation. Continuing Medical Education. Radiographics. January 2001 21:1 193-216
- Poli-Neto, Rosa-E-Silva, Barbosa, Candido-Dos-Reis, Nogueira. Endometriosis of the soleus and gastrocnemius muscles. Fertil Steril. 2009 Apr;91(4):1294.e13-5
- Anaf, Simon, El Nakadi, Fayt, Buxant, Simonart et al. Relationship between endometriotic foci and nerves in rectovaginal endometriotic nodules. Hum. Reprod. 2000 15 (8): 1744-1750
- Ceccaroni, Clarizia, Cosma, Pesci, Pontrelli, Minelli. Cyclic sciatica in a patient with deep monolateral endometriosis infiltrating the right sciatic nerve. J Spinal Disord Tech. 2011 Oct;24(7):474-8
- Teixeira, Martins, Avila et al. Endometriosis of the sciatic nerve. Arq. Neuro-Psiquiatr. 2011, vol.69, n.6, pp. 995-996].
- Grand Rounds; “Endometriosis of the Sciatic Nerve.” Mazin Ellias, MD. Medical College of Wisconsin. April/June 1999
- Wadhwa, Thakkar, Maragakis, Höke, Sumner, Lloyd et al. Sciatic nerve tumor and tumor-like lesions-uncommon pathologies. Skeletal Radiol. 2012 Jul;41(7):763-74
- Possover, Schneider, Henle. Laparoscopic therapy for endometriosis and vascular entrapment of sacral plexus. Fertil Steril. 2011 Feb;95(2):756-8
- Ghezzi, Arighi, Pietroboni, Jacini, Fumagalli, Esposito et al. Sciatic endometriosis presenting as periodic (Catamenial) sciatic Radiculopathy. J Neurol (2012) 259:1470–1471
A version of this article was published previously on the Center for Endometriosis Care website. The current version was edited by Hormones Matter staff and reposted with permission, first in 2013 and again in 2016 and 2019.










This is very interesting indeed. I have severe sciatic pain during my menstrual cycle days 1-3. Radiates down my left leg every single time. I find it difficult to stand for long periods of time. I am only 30 but I feel older when I get this pain haha. I have a few other symptoms of this endometriosis but no confirmed diagnosis. Thanks for the article!
Hi Elena
I also have the same thing.
I am 35 and the year before the first lockdown I started experiencing a pain in my right bottom that shoots down my leg. This only happens every time I start my period. It stops after the first day then gets really bad around ovulation. Causes sleepless nights. Went to a chiropractor and did an X-ray. Showed that I had a few degenerate discs and was offered a course of treatment. I didn’t really carry on the treatment as I felt like I needed to investigate further just incase it could be something else. I only thought this because it’s happening during my periods so there’s a link it could be hormonal related. I have recently had an mri and just waiting on results.
I cannot stress enough on how painful and mentally draining this has all been for me. Most people I tell at my workplace tell me they have experienced this pain during pregnancy. Know one has experienced it just through their period. Doctors don’t know anything about it. Living on painkillers isn’t what I desire for the rest of my life so wish to god we can find what the actual cause is.
Hi Sinem,
I experience the same symptoms for years. The pain is horrible and
starting to effect the nerves in my legs. It is really scaring me! Just wondering what the outcome was and did you get treatment for the pain. Thanks
Rose
Hi Rose
I got my mri results back and all came out clear. Not sure how that could’ve been because the chiropractor told me I had disc degeneration and one bone missing from my spine. Mri is more clear so was I being lied to? God knows.
I went recently to see an osteopath for a second opinion. He said all looks normal and the pain I could be experiencing is called piriformis syndrome. He said he can help me. Just don’t know why it’s happening during menstrual time and a week before ovulation,
If it’s sciatic endometriosis the only way to detect it is laparoscopy.
I’m suffering this too. Have you had any relief at all?
Hi,
I doubt that sciatic endometriosis might be what I am suffering from. I have had pain in my ankles, mostly right, but sometimes on the left too, since atleast 2015. It is a kind of radiating (I don’t know the correct word) pain, but often difficult to pin point a location on my ankle. On some occasions, I can feel the pain radiating from my sciatic region towards the foot along the calf muscles. The doctors I have consulted have not found anything in the xrays or blood test. Since my menstrual cycle has been highly irregular in the past and still a bit irregular, I cannot with 100% confidence say this, but I almost always notice that the pain is severe a week before my periods. My periods is not particularly painful I think. Blood flow might be on the higher side, not sure again how to judge this. But this pain is making life a hell for me. Also, I have had an abscess on my right lower back in 2014 which was more than an inch deep and was surgically removed. Was wondering if all these are related. Can anyone suggest if I should bring this up with a GP and should I consult a obgyn?
I’m not sure if this is an okay place to comment this on but I’m at a loss and I don’t what to do. I broke my tail bone in head start(pre school), from a nasty push off of a swing set. It was determined by a doctor that it was in fact broken. Fast forward a couple months to when it was healed and everything looked good, I have horrible pain starting in my lower back and going in my hips, down my legs and Into my feet. And a tingling burning in my feet mostly the left foot. I am now 22 and I still have this pain. Only its getting more and more frequent. I’ve seen countless doctors but none of them seem to have an answer because these “episodes” only last about 30-45 minutes. What do I do?
Try a chiropractor or acupuncture!
Yes, but the cause is a disturbing focus leading to Dysautonomia, influencing the hypothalamic-pituitary-hormonal cascade
and influencing the intervertebral joint fluids, leading to irritation of the nerve roots, leading to muscle constriction, arterial constriction, compromised venal and lymphatic flow in the connected dermatoms.
This is a great article thanks for sharing 🙂 Nancy Peterson’s remarks on Facebook about it being in the side pelvic walls made me think about it a lot since I have have Deep dissection of the pelvic wall and wondering if the sides were checked at all or he just focused on that part. Very interesting indeed.