I would like to begin sharing my story, hoping to help others. My journey is from a nurse’s perspective. I recently learned I am thiamine deficient and likely have been for years. Thiamine deficiency affects the mitochondria, causing a disease process known as beriberi. Beriberi mimics many other illnesses, making it very difficult to diagnose. Let me begin by giving you a background about the woman I was before thiamine deficiency depleted my entire being.
I have always been highly driven. I am perfectionist to a fault. I was an honor student in high school, an active- athlete, a cheerleader for four years. I loved swimming, ice skating, rollerblading, skiing, and all sports. I led many extracurricular activities throughout high school and college. As the oldest of 5 siblings, I was the family leader and caregiver as well. I was always strong mentally and physically. I had survived spinal meningitis at age 5 years, after receiving my last rites while hospitalized in isolation several months. I lost my father shortly thereafter, but I survived.
I was a successful RN for nearly thirty years; a gynecological oncology nurse the first 20 years, and a postpartum nurse caring for mothers and their newborns the last ten years. I was married and had two children and even though I worked full-time, I was an avid volunteer, for activities involving both daughters through their elementary and high school years. I was the first and only woman president of my neighborhood association, organizing many monthly events throughout the year. I cared for my mother through ten years of Alzheimer’s. No family member was hospitalized without me as their private duty nurse advocating. I cared for my father in-law through colon cancer, then moved my mother-in-law in with us for 15 years after he died. I watched over her into her 90’s. Then I suffered loss upon loss: my mother, my father-in-law, several aunts, and two beloved family pets, followed by an awful divorce from my high school sweetheart.
Looking back, I understand why my marriage fell apart, I became a woman I barely recognized. I was in pain all the time. I was tired unable to be the “active fun loving Jane,” I had once been.
In 2006, I developed degenerative disc disease (DDD) in my neck, which ultimately led to a cervical fusion. Nevertheless, I returned to hospital nursing 8 weeks later and worked until I could no longer get through the nonstop days without pain. My nursing manager talked me into management after 28 years as a bedside nurse, which I loved. Then, I suffered a lower back injury that, together with my neck issues, incapacitated me from my nursing career. After losing my career, my marriage, and my home, I moved away from the home town which I loved. Multiple losses, stressors, and what I now believe was thiamine deficiency had me suicidal.
I tell you this, because the thiamine deficiency was insidious. It accrued over time. I was performing and had more energy than most… until one day, I didn’t.
My Silent Demise: Unrecognized Thiamine Deficiency
As I mentioned above, I developed DDD in 2006, and as result, I have suffered for years with intermittent nerve pain and muscle weakness. Over the years, the pain and weakness progressed to the point where by 2019, I could no longer walk or function. I had great fatigue, insomnia, depression, anxiety, and lack of energy. This was in addition to GI distress and signs/symptoms of IBS irritable bowel syndrome. I also had serious bladder issues of great urgency, leaking and even incontinence at times. Over time, I developed significant brain fog and cognitive difficulties. This included a “loss of words,” an inability to read and retain information or eventually, to write; all of which I had always loved doing. I began having memory issues and my nervous system seemed to be shutting down.
Looking back on my history, I had been hospitalized for chest pain 3-4 times ruling out pulmonary embolism or heart attacks. I have had a vitamin D deficiency for over 10 years despite supplementation and good diet and plenty of sunshine. My platelets ran high on and off for years. A hematologist ruled out many disease processes through lots of blood work. He even did a hip bone marrow aspiration and never found answers.
My blood pressure at one point was 200/100. I had tachycardia documented on EKG and on my own nursing checks. Heart palpitations were common. I sought the care of a few cardiologists over the years and had a number of cardiac tests all with no answers. I was frequently dizzy, seeing stars, and nearly passing out on many occasions. Five years ago, I was severely depressed and suicidal. I had lost so much weight, and looked anorexic at 108 pounds. Looking back, I have no idea how or why I had such rapid weight loss. Then the weight issue shifted.
By the end of last year, I had difficulty walking. I gained weight and have now been walking that fine pre-diabetic stage. I seem to be insulin resistant now. Added life stressors, once again caring for my sick and aging 81 year old aunt with multiple medical issues, has led to self-neglect. I became short of breath on exertion, weak and faint. I began losing my hair. Thankfully, I once had a thick full head and so the hair loss was not immediately noticeable. Even so, I noticed, and I begged my doctor to help me learn why my hair was falling out and thinning so much but my concerns were made light of.
I pleaded with many doctors, asking to learn the cause of my multi-organ system’s failings. I suspected they were medication effect or vitamin deficiency related but several good doctors rolled their eyes when I begged to be tested.
I grew weaker and weaker, sicker and sicker as 2019 came to an end.
The Laundry List of Tests and Doctors Conclude: It’s All in My Head
An MRI in January 2020 showed cervical myelopathy but not significant enough to warrant more surgery (THANK GOD). The orthopedic surgeon and his nurse practitioner, offered Gabapentin (as did 5 other doctors) and physical therapy (PT). I refused the gabapentin because it had made me incoherent in the past. I agreed to try PT but was frustrated, since I had tried physical therapy more times than I can tell over the past ten years. This last time, in February, just the PT evaluation magnified all my symptoms and I barely walked back to my car. Returning to my vehicle, I felt like I was on fire with burning nerve/muscle pain all over.
Again, I adamantly refused meds without learning the cause.
I was sent to have an EMG (nerve-muscle functioning testing). The EMG showed multi-nerve damage, or “multiple peripheral neuropathies.” That was in March of this year. I had been twice before to this same physiatrist having EMG’s years prior due to ongoing “nerve pain.” Like many other doctors, he never suspected thiamine deficiency and implied that it was “all in my head.”
I was sent to another consult, a Brown University rheumatologist, who basically told me the same thing that my pain was “in my head,” as most docs do seeing history of “depression and chronic pain.” On exam, I actually jumped when he touched my outer thighs and various areas on my body. I was super “nerve sensitive,” which he was attributing to “my mind.” Outer thigh pain/ sensitivity was a symptom of thiamine deficiency I’d later learn. After my RN daughter, acting as my advocate, spoke on my behalf asking for nutritional deficiency testing to rule out causes, he tried ordering labs but had little knowledge of what to order and “could not find the transketolase test or a simple Vitamin B1 test on my screen,” he replied. To appease me, he ordered multiple other labs and sent me on my way with no diagnosis and no return appointment.
For the multitude of GI symptoms, I was sent to a caring gastroenterologist who performed a colonoscopy and endoscopy with insignificant results and biopsies all normal. He too was empathetically puzzled, urging me to request a thoracic MRI due to my history of degenerative disc disease. Upon exam, this doctor was alarmed at my sensitivity at my breastbone area when touched. It was painful and clearly inflamed.
I had all the symptoms of multiple sclerosis (MS) too, so I had a brain MRI with and without contrast that I asked for after researching my symptoms, wanting to rule out MS too. The MRI showed: “a single small focus of flair hyper-intensity within the frontal lobe white matter, nonspecific and could not rule out demyelinating disease or MS…”
They ruled out “pinched nerves” in a thoracic MRI, recommended by the GI doc after not finding answers to my GI symptoms. I had repeated X-rays and a lumbar MRI having a lengthy history of lower back pain too.
The lumbar MRI incidentally found gallstones which sent me to a surgeon who recommended gallbladder removal. In this COVID environment, I have minimized symptoms with better diet and supplements thus far.
Discovering My Thiamine Deficiency: A Bit of Research and a Bit of Serendipity
In February 2020, I had begun reading the book “Thiamine Deficiency Disease, Dysautonomia, and High Calorie Malnutrition,” written by Dr.’s Lonsdale and Marrs. From the case studies and the research, I knew that I had thiamine deficiency. The trick now was to get someone to believe me. I brought the book to an upcoming neurologist appointment. Although, with each of the 7 previous consults, blood work was done, it was this last consult, with an astute neurologist, that I found out why. He knew after examining me and listening to me that I was deficient in thiamine. He took the time to research my history and found that I’d been diagnosed as thiamine deficient 5 years ago, but sadly, no one told me. In 2015, lab tests showed that my thiamine was 6 nmo/L , below the lab’s reference range of 8-30 nmol/L. I was still deficient in thiamine in February 2020 with a result of 7 nmol/L. He explained that I “needed to take 100mg thiamine daily, starting immediately and that it would likely take 6-12 months to hopefully reverse symptoms.” He also indicated that I would need supplementation for life now. As I have continued to research and read about thiamine deficiency, I learned that I would likely need much higher doses of thiamine, in the form of something called TTFD. TTFD is a synthetic thiamine that crosses the blood brain barrier getting into the cells better.
A Possible Family History of Latent Thiamine Issues
I continued reading, researching, and learning from case studies and groups. Thiamine deficiency is much more common than thought today. It can be passed on at birth in an unknowing deficient mother. Looking back, I fully believe my mother was deficient given her history of problems in school, high anxiety, and severe depression on and off for years. Her symptoms worsened with divorce when she was still pregnant with her fifth child. Each of her children were born only 12 – 13 months apart! I recall her getting dizzy, feeling faint often. She suffered with leg pain for years.
I am most concerned over the genetic factors influencing me and my family. The first stages of thiamine deficiency see thyroid issues, which my mother, sister, and aunt all had/have. Diabetes runs in my family: my grandmother, aunts, sister, and I’m now at the pre-diabetic stage. Cardiac issues are often seen: my grandmother, mother, aunt, and I have had them. GI issues also are noted in multiple family members. The most worrisome disease is Alzheimer’s disease, which is often seen in late stages of thiamine deficiency according to research. My grandmother, mother, many of her sisters (now deceased) all had Alzheimer’s disease. I am currently seeing early Alzheimer’s and short-term memory loss in my 80 year old aunt and her 75 year old youngest brother.
I have been monitoring my aunt who could not tolerate the Alzheimer’s medications that she was given. I began using thiamine with her in March 2020. We began with a good B-Complex having 100mg thiamine mononitrate and then added 50 mg Allithiamine in mi- July when she got very sick with what I believe was Covid-19. I kept her on this dose through August and then upped it to 100mg in September. I am now seeing improvements. Her energy has improved greatly. Although still forgetful, her memory is improving. She recovered after three weeks with the virus, yet suffered with extreme fatigue many weeks to follow. I will write about her story in a subsequent post.
The Path to Recovery
As a nurse, journaling my symptoms, diet, supplements, and vital signs, etc., I have watched my symptoms, rated on a scale of 1-10 with 10 being worse, go from 7-8s down to 3-4s over the last 6 months, after beginning thiamine replacement. I have been thoughtfully self-experimenting, slowly increasing my TTFD, using the brands called Allithiamine and Thiamax along with magnesium and potassium for proper absorption. Since rebalancing thiamine often brings out other deficiencies, I alternate a good multivitamin/mineral supplement and B-Complex and take probiotics for good gut health and better absorption. Over the last 6 months:
- My neuropathies, which were tested pre-thiamine in February 2020 and again in June 2020 after a little over 5 months into thiamine treatment, are reversing.
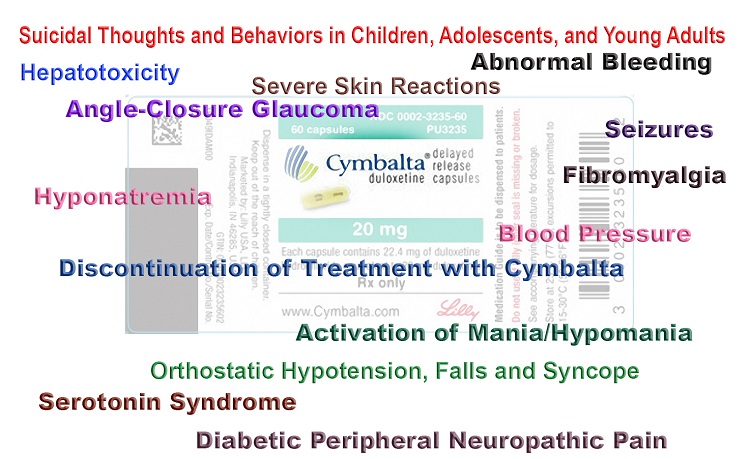
- I am off all pain meds, antidepressants, and other scripts (weaned under supervision SLOWLY).
- I am happier, calmer, healthier overall.
- I am most impressed with my renewed desire and ability to read, write, and research and retain information learned!
I’m now so hopeful for a good recovery by next spring. I understand I will need thiamine supplementation for life now, hopefully in lower doses eventually. Time will tell.
Drugs Don’t Solve Vitamin Deficiencies
With this experience, I have learned that there is no one easy answer for all as far as dosing goes. Replenishing thiamine requires careful rebalancing of other vitamins and minerals, as most people have multiple nutritional deficiencies. Prior to supplementing with TTFD, my labs showed Vitamin D deficiency for over ten years and low thiamine since 2015. If not for the COVID environment, I would have been hospitalized for IV thiamine treatment and looking back now, probably should have been.
I hope my story here can in turn help others find answers which sadly so many Western doctors seem to miss. Nutritional knowledge is barely taught in medical school. I hope that changes, as malnutrition is often the root cause of many diseases. I know all too well how frustrating it can be to go from doctor after good doctor who only know what they are taught: “treat symptoms with drugs.” Sometimes, it takes one’s own persistence, research, and being proactive to regain wellness. Of course, wellness means cleaning up the diet by avoiding processed foods, carbs, and sugar. Recovery takes eating clean, whole organic foods mainly. It means balancing exercise, sunshine and good mental health. It takes looking at your environmental toxin exposures. It means DE-stressing and cutting back on EMF’s. It takes changing your lifestyle but most importantly, listening to your body and allowing rest and recovery and above all, a well-balanced life.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Photo by Marija Zaric on Unsplash.













Anthony, I too have burning lactic acid in thighs. After years of trying to find diagnosis, figured it to be chronic venous insufficiency, aka CVI. Medical history includes (stress in childhood from alcoholic parent and so on), Hashimoto’s and celiac, a heart attack (“idiopathic”, no stents) after eating a lot the day before and dehydration walking fast in a 5k. I have just ordered Eliot’s thiamine and will go from there with other supps (niacin is awesome). Otherwise, what helps is not eating much, drinking my meals (smoothies) for hydration and higher nourishment, and de-stressing (sleep helps). From different practitioners I know I don’t process carbs, nor fats well. So that leaves protein, and I don’t like meat. 😛 I’m likely on the autism spectrum undx, but I don’t care about that. With CVI, allopathic’s answer is to remove or cauterize the vein of which I’m scared to do. I do need to lose weight which has been difficult I think due to possible candida (hard to get diagnosed). I crave starch which feeds the candida I presume. I believe the candida or dysbiosis is affecting vessel walls (could also be viral as the world has learned from news on this year’s popular viral strain).
Look into amyloidosis as well.
They ruled amyloidosis
out during my hospitalization hospitalized. My daughter & I thought that was a top possibility too.
Jane,
I just found this website and and I concerned that my daughter may have A vitamin B one deficiency. She has Hashimoto’s and vitiligo and recently took a drug called gabapentin which left her almost bedridden and with severe hand and foot swelling. Her blood test show that she is low in albumin, magnesium, folate, and potassium. We did not have any vitamin test done. She is 33 and absolutely miserable. I have tried to contact so many doctors as it has been six months since her last dose of gabapentin. They all say that no drugs could cause this. Maybe they’re right maybe it is just a combination of so many drugs she has taken over the years for pain. She also has had severe pelvic pain. She is a beautiful, bright, strong young woman… it kills me to see her in such a poor health. Where did you learn about all this dosing information? Is there a doctor that will treat her? We are so desperate for help.
Sry, just seeing your message now.
Even my astute neurologist who’s diagnosed me is learning lots from my researched articles that I bring him from Dr.’s Lonsdale and Marrs. He encourages me to be PROACTIVE which I have had to be!
He diagnosed me then told me I immediately needed to begin taking 100mg of any OTC Vit B1. Researching has taught me most but the most frustrating part has been dosing because there’s so many conflicting opinions out there.
What I have learned most is that treating symptoms earlier rather than waiting for testing, which is not always accurate, is easier to treat than chronic deficiency.
Start LOW and UP dosing SLOWLY.
Learn about the many forms of thiamine first. Dr.’s Lonsdale and Marrs have many great article’s here on all this.
Unfortunately, you won’t find one EASY answer right for everyone. We each start in different conditions with various underlying health issues and root causes; have had different stressors; genetics seem to be a huge component; history of steroid and antibiotic heavy use ; medical history; diet issues and more may dictate doses needed.
I have found most tolerate thiamine hcl, the water soluble form fairly well unless their health is very fragile. Early on IV therapy helps us most but trying to find doctors who’ll give it to those other than alcoholics, ironically!! That’s only one of many other causes of TD and until we can get it recognized as a disease needing thiamine to see improvements, we’re left on our own to educatedly trial things. I journal, learn all I can and carefully try things after talking to many highly educated people. Early on it was a very challenging journey but I now tolerate most forms and high doses. I use ttfd form combined with hcl form and benfotamine to help my peripheral neuropathies. I’ve slowly upped dosing carefully journaling and supporting my electrolytes, and other vitamins and minerals.
@Ann- Since you mentioned vitiligo in your post, I just wanted to mention that when reading reviews for Betaine HCL, I came across a post from a woman who said her husband had vitilago for many years and that Betaine HCL was helping to get rid of it. He wasn’t 100% healed, but definitely on his way. I just looked for that review to post here, but couldn’t find it. But here’s a post on low stomach acid and vitiligo: https://thevitpro.com/low-stomach-acid-and-vitiligo/
Thank you so much for writing this! I’m currently bed-bound again by what I believe is B-1 deficiency. After ten years in Africa, and more parasitical infections than I care to remember, I now suffer from multiple autoimmune diseases, Celiac Disease being one of them. I could feel Thiamin deficiency creeping up on me again, but I chalked the tail tail symptoms up to other things. Multiple ER trips have revealed absolutely nothing, except the fact that doctors like to push medications that have an array of awful side effects (which I’ve always refused), or the subsequent diagnosis of “anxiety.” I’m currently supplementing with high doses of a B complex, and am waiting for the Allithiamin to arrive in the mail. I also take magnesium with every dose of B complex, and plan to add nutritional yeast to my food. This is just a dreadful deficiency to battle, and at times very scary. Again, I appreciate you sharing your story as well as all that you’ve learned (are learning). Many blessings as you heal.
Thank you for making time to read my story. I’m so sorry you’re going through this awful disease too. It is infuriating how dismissive doctors can sometimes be. I am working on part 3, now ten months into my thiamine high dose therapy. Stay tuned. I’ve learned lots more, in relation to viruses, testing, and more. Well wishes. ❤️??
It is important to understand that this is nothing to do with vitamin replacement. We are advocating thiamine as a drug and I will try to explain. The major activity of this vitamin is a catalyst for enzymes that turn glucose into energy. But these enzymes also require magnesium. Recent research has shown that thiamine is also required for processing certain fats, and it has long been known that it has an important effect in protein processing. Therefore, thiamine and magnesium are required for the oxidation of all foods. Because the diet in America is very high in calories and deficient in the necessary catalysts, the enzymes appear to deteriorate gradually. We know this because of the studies done in determining that thiamine deficiency was the cause of a disease that had been haunting mankind for thousands of years. It took huge doses of the vitamin in order to retrieve the health of affected patients. Beriberi has a long morbidity and a relatively low mortality so that affected individuals suffer for many years when the deficiency is not recognized. Add to this the fact that genetic changes appear to be quite common. The appalling fact is that a mother can be thiamine deficient and provide a legacy to her yet unborn child that goes through his or her life. So using thiamine as a drug is an attempt to stimulate the damaged enzymes so that their full effect is restored. Please understand that this information has been deduced from clinical and library experience, not by concentrated scientific studies. Recognition of the symptoms is obviously mandatory, but all of them are the result of energy deficiency and this explains why fatigue is a major symptom. But I cannot claim that thiamine is the only catalyst necessary for the production of energy, perhaps explaining why megadoses of thiamine sometimes do not work. Therefore, if you have found that your symptoms respond to thiamine, you must then add B complex, magnesium and a multivitamin.
Thank you Dr Lonsdale for this clarifying message. It is greatly appreciated.
I understand I am using thiamine as a drug at much higher doses than “vitamin replacement,” trying to correct my issues now in beriberi, long standing deficiency stages.
I do understand the importance of adding magnesium, BComplex, and multivitamin since seeing how thiamine has minimized my symptoms.
I recognize that MY long standing thiamine deficiency has damaged my enzymes and that life long therapy for me will be needed. I’m grateful for your research in the progress I am making, but also know realistically that my outlook is more challenging. I also understand that the production of energy is complicated and includes many factors.
I’m grateful for my continued learning from both you, Chandler Marrs, and others.
Sincerely,
Jane Finn
Thank you very much for all this information.
My story is very much alike but I cannot really tell it because my english writing is not that good . And also I am too tired.
I am 63 years old an live in Belgium , where doctors even have less knowledge of all this
You are helping me a lot cause I thougt I was going crazy and so do the many, many doctors I ve seen .
Kind regards
Francine
Hopefully one day, you will learn to tell in here with translations. It’s good to know we are not alone. ❤️??
This is a belated response to Jane who asked me to talk about thiamine. There are very limited body stores and we can easily run out in a severely stressed world. Every mental and physical action requires energy and thiamine is the “gatekeeper” for energy synthesis. The brain, heart and nervous system are the most energy consuming organs and the brightest brains are more at risk because of this. Poor diet, surgery, trauma and critical illness are all at risk for thiamine deficiency (TD) because of the energy requirement and that certainly explains some of the “inexplicable” symptoms of Covid-19 and the prolonged symptoms that haunt post viral disease for months and can last indefinitely. An important post on Hormones Matter discusses the research on “stress” by Hans Selye who was the first to show the vital connection of “stress” with the need for energy to fight it “adapt”. Prolonged TD is hard to reverse and we have known for years that the treatment of beriberi required huge doses of thiamine for months to reverse symptoms. Why do doctors rarely spot the typical symptoms and call them psychosomatic. The entire profession believes that vitamin deficiency absolutely does not occur in America.
Thank you Dr Lonsdale. As always, I keep learning more everyday thanks to YOU and Chandler. I continue spreading awareness, hoping to prevent others from being ignored as I was for way too many years! I so appreciate you both! ❤️??
Dr Lonsdale,
Thank you so much for all the work you put into responding to questions and writing articles. I am sincerely hoping what I have going on is simply thiamine deficiency. I’m a 45 year old male and about a year ago I developed acute kidney failure coupled with intense abdominal pain (they’ve no idea why). For almost a year afterward, I could not tolerate most foods for the pain. I ate mostly just steamed cabbage (mostly red cabbage at that (which I now understand has anti-thiamine components)). I continued this diet for 10 months and over the same period of time developed some pretty extreme memory issues. I pretty much forget anything that happened (or that I learned) more than a day ago. It’s short term too in that I can easily forget who I’m on the phone with or what we’re talking about if the conversation goes silent for a few seconds. I can easily even forget I’m on the phone. This has been coupled with pretty severe fatigue and some neuropathy and a sudden increase in blood glucose levels. I find that ANY carbohydrates worsen all of my symptoms. I’ve been taking TTFD at about 2.5 grams / day (spread across the day) for 6 weeks now with zero improvement. Is it possible that this is just going to take longer than a couple months? Please respond as I’m becoming increasingly concerned that life as I know it may be over.
Hi Joe,
I hope reading my story has shed some light on yours. I have learned from Dr’s. Lonsdale and Marrs that if one has long standing deficiency, it may take 6-12 months to reverse symptoms.
I have learned time and patience along with balanced diet and supplementation is most helpful. Well wishes Joe.
❤️?? Jane
Best to take with magnesium too…..they need each other.
Dr Lonsdale,
I hope you are still reading these posts.
Dr Lonsdale,
I wondered if you could offer some advise.
For many years I have been suffering with mental/physical fatigue.
The first noticeable “debilitating” system was in my thigh muscles, I suffer from a “burning” like sensation. similar to an over exertion squatting heavy weights in the gym producing lactic acid.
Each year i’d feel more pain in my thighs after little exertion. I was always off sick in bed for a week or two, by 2015 noticed I was usually off work several weeks per year where my body was completely wiped out and I was unable to get out of bed. fevers, flu, norovirus and other such related issues.
Prior to that as a child I had tons of energy, I was always good at athletics ; one of the fastests sprinters at school’s, hurdles and high and long jump.
By 2016 I had crashed completely, I was frequently urinating, always thirsty. Poor digestion – loose stools/diarrhea – ( My digestive system was never good since I was child and I believe I became more and more intolerant to foods).
Constantly absolutely exhausted, felt like my body was not able to produce ATP at all. I would have to lay in bed most of the day , sleep was unrefreshing By now I was struggling to stand statically for more than a minute or two. I could walk 0.5 mile or so, but I felt so wiped out.
My shoulders would burn, even sometimes using my phone would tire my muscles.
I had numerous GP visits, paid to see Physiotherapists, Endocrinologists, Chiropractors, Rheumatologists, Neurologists. They all had no idea and labelled it as a “post viral” issue and or CFS.
Luckily my brain still functioned well, I was able to work.
After researching answers myself and not giving up hope I came across the RCP. – For several years (3 years) I have been following the RCP (root cause protocol). Reducing my unbound iron, increasing magnesium, ferroxidase activity and other related vitamins from food. working out my food allergies brought me out of bed and functioning well, the clock has definitely turned back. But I lost a lot of weight (79kg -> 68kg, 6ft tall). No sugar, very low carb (as cant digest grains/rice/pasta well)
I am still unable to “exercise”, I can walk several miles but I am unable to climb many flights of stairs without my legs burning. Even 5 squats with no weight will cause me to feel lactic acid burn, which I am still trying to connect the dots too.
Recently I have had a sore right index finger (feels like RSI) for 5 months, if I rest it it feels okay, only sore under use. Most other symptoms have slowly resolved.
I read a lot of papers on thiamine and lots of posts by yourself, including various youtube videos by Elliot. I decided to start increasing thiamine via raw garlic several times a day and lots of pork. Slowly moving on to tiny amounts of Allithiamine by August 2020. I have been slowly titrating and am up to 300mg Allithiamine. I consume 1tsp of Bee pollen daily, several tsp of unfortified nutritional yeast, 300mg of Ox liver per week and recently added a whole food b complex (garden of life) to support the other B vitamins as you suggest. 600mg of magnesium per day, potassium and salt are also supplemented.
I definitely feel like i’ve shifted a gear, but this lactic acid issue in my legs has not gone away.
My question are:
1.) Does this sound like a Thiamine deficiency? – As a child I was unable to produce enough Growth hormone and had to be injected daily 0.25ml since 3->17. I was then tested and deemed normal at 17. I have not read any relation to this before, but wondered if you had come across anything?
Test Readings:
19.8 mU/L in 1987
in 2001 – 104 mU/L at 60 minutes on the ITT. GH then discontinued.
link to my bloods – https://docs.google.com/spreadsheets/d/1NIRFdw7F_ZF3Gj7PdkChn8S9QjMvFwd5bhOJNmTpi9I/edit?usp=sharing
as you can see i did have a high B12 reading, I also read this can be due to a thiamine deficiency as it’s not being utilised in the blood.
2.) I have not seen many report of supplementing Allithiamine over 300MG. I have read you state many times it is safe, but I don’t want to overdo it and cause other functions to go out of balance after all this progress.
Thank you so much for all your research, articles and post replies.
Dr. Ben Lynch mentions that Lithium Orotate 3mg takes B12 into the cell. For some people B12 tends to just float around in the blood.
Hi Jane, I’m happy that you’re feeling better. Have taking thiamine help to cure your neck? My brother has this same condition disc disease (DDD) doctors told him it was calcification which fusion. He’s unable to turn his neck to the left. I feel so bad for him. Also do you think thiamine deficiency could cause nystagmus? Thanks Erica
Erica, I believe thiamine deficiency may be the underlying issue in many diseases as Lonsdale and Marrs elude to in their book and on this site. They have many great articles here to learn more.
It has helped minimize my DDD lower back and neck pain. I’m off all pain meds now. I too have had a neck fusion C5-C6 and had many steroid injections in my lower faucet joints in my lower back due to DDD pain. Wish I knew back then, what I now understand about thiamine role.
It is important for the reader to understand this complex story. Without thiamine, cellular energy is impossible and you have between 70 and 100 trillion cells that require it in order to function. It is a situation where genetics and nutrition come together. Note that Jane describes her adolescent years that clearly indicate her superior ability. This superior mental and physical function requires superior cellular energy. Her capacity to meet this demand presumably failed because of poor diet or genetic risk factors. Her description of family illnesses suggests that there was indeed genetic risk. Every mental and physical function depends on energy and it becomes easy to understand why there are so many symptoms attached to thiamine deficiency. It depends on the distribution of the deficiency as to where the symptoms will develop. The brain, heart and nervous system are the most energy requiring organs in the body, so it is not surprising that they are the most affected by this deficiency.
Thank you Dr Lonsdale for hearing my story. THANK YOU for all your many years of empathetic HARD WORK and passion for helping others. I continue re reading your book. You have helped so many, and I hope to continue spreading your word for years to come! You are truly appreciated more than my words will ever express. I will continue thanking you and Chandler Marrs for the rest of my life!
Hi Anthony,
You sound so much like me and my story here. I have used high dose allithiamine and other thiamine forms.
I’d be glad to talk to you privately on Facebook PM if you’d like to friend request me. Thxs for reading my story.
I too would love to hear Dr Lonsdale’s most up to date advice on thiamine dosing and the now “gold standard” testing for thiamine deficiency. He does have many articles here on hormones matter. Thiamine Deficiency, Dysautonomia, and High Calorie Malnutrition by Derrick Lonsdale and Chandler Marrs is an excellent resource also ( copyright 2017). I am so grateful to them both for helping me in my fight. It sure sounds like you too have had long term thiamine deficiency which from all I have learned, takes at least a year on thiamine supplementation to hopefully reverse symptoms.
Jane Finn or email me at finnjane19@yahoo.com
Dear Jane,
I notice that your surname Finn is Irish and I wondered two things – firstly, do you have direct Irish heritage or is that a maiden name? Secondly, if you do have direct Irish heritage, as I do, do you think its something that the Irish are especially susceptible too? The symptoms you describe are very common in my family and many others that I know.
Ps – your story is fantastic and a testament to the fighting spirit and never giving up/
Hi Brian,
Thank you for taking the time to read my story. I’m sorry to hear your family has similar issues too.
FINN is my name taken by marriage. I’m of Portuguese decent.
These issues are much more common than recognized by Western Medicine.
It’s why I’m sharing my story.
I hope you’ll research too and find best answers for your family.
More of my story to come. Well wishes to you and your family. Thxs for caring! ❤️??
How much allithiamine were you suggested to take per day to reverse the symptoms?
Have you tried increasing the dose?
I started by taking a good BComplex in March, then increased to allithiamine 50mg, slowly upping by 50mg to 200mg April, until I got Elliot Overton’s thiamax 100mg caps. Then I used Both to keep upping dose by 50 mg until I felt best taking 300mg 3X/day in divided doses for me as it seemed to last 4-5 hrs then I’d crash.
My long standing deficiency, now thiamine dependency, requires higher doses to feel the benefits.
I’ve personally tweaked my dose using various forms depending on my stress and health status.
After chelating testing sent me into acute kidney failure, I requested IV thiamine 500mg every eight hrs. They kept me on that dose x 2days, then 200mg IV every eight hours for the week along with oral niacin 500 mg and a multivitamin Tab.
I got home and took lipothiamine 200mg three times a day which helped lower my BP, BS and reverse my kidney failure.
I have the same symptoms,tingling numbness,burning began in feets 10 years ago,climbed up to over the knee,also pains in my thighs,since 2-3 years same happen in my hands and arms,(and I cannt play the piano no more–I am aconcert pianist,ahime…) woking with a cane ,my brain function and cognition\memory,is still ok,but being an M.D by profession\education,and interested also in naturopathy,including studies I did in naturopaths schools,I had a big suspissioin that I had a problem,and when I mesured organic acids in my urine,a test that was done by my naturopath coleeghs,I found that I WAS NOT ABSORBING THE B vitamins,and especially defficient in B1=THIAMINE !!! This gave me the reason for me crying all the time that ”I HAVE BERI-BERI,–LOOK AT ME!!! I HAVE BERI BERI!!!” which no neurologist took seriously!!!,they think that BERI BERI has passed from the world and was only in INDIA of the 19th cencioury…I have also a cervical spinal stenosis<and they wanted to opperate on me to enlarge my cannal and fix me with scruse and metal plates,which I luckyly refused.I have an IBS CONSTIPATION,and my kidneys are working now badly with eGFR at 49,I also have a problem with LEAD which I suspect might have caused me some probleme because stupidly I've soundproofed my piano room with LEAD some 20 or more years ago,and still have to find out if it has a connection in all my condion with the thiamine defieciency,and or my renal function etc. I am still trying to connect all the dots here. I saw here in your webside that chelation therapy with EDTA for LEAD cronich toxisity may be even more harmfull for thiamine defficiency.SO now I am really at the end of my roap and wits–I am living in ISRAEL!!! PLEASE–HELP!!!
I’m glad to hear of your success. I’m taking 150 mg Allithiamine, B complex, 400 mg magnesium and a multivitamin in an effort to balance my hormones (I have primary ovarian insufficiency) and cure my POTS. Like you, I suspect my family has had a history of thiamine deficiency. I suspect I’ve been deficient my whole life even though the clinical symptoms only began recently.
I noticed improvement of symptoms immediately on starting the thiamine (50 mg) but have been titrating the dosage because I still have POTS. My sympathetic nervous system is also really sensitive and I have insomnia issues. I’m sure vitamins or hormones are related. Has thiamine supplementation helped with your sleep? Or has anything else?
I started by taking a good BComplex in March, then increased to allithiamine 50mg, slowly upping by 50mg to 200mg April, until I got Elliot Overton’s thiamax 100mg caps. Then I used Both to keep upping dose by 50 mg until I felt best taking 300mg 3X/day in divided doses for me as it seemed to last 4-5 hrs then I’d crash.
My long standing deficiency, now thiamine dependency, requires higher doses to feel the benefits.
I’ve personally tweaked my dose using various forms depending on my stress and health status.
After chelating testing sent me into acute kidney failure, I requested IV thiamine 500mg every eight hrs. They kept me on that dose x 2days, then 200mg IV every eight hours for the week along with oral niacin 500 mg and a multivitamin Tab.
I got home and took lipothiamine 200mg three times a day which helped lower my BP, BS and reverse my kidney failure.
It was helping ease all my symptoms. I found I needed to not take it after 4 pm and in divided doses throughout the day, as it would keep me awake with too much energy taken in evening.
I tweak dosing according to stress, illness and needs.
Melatonin helps me sleep.