Think Halloween, spooky costumes, and “trick or treat” – only it’s summertime. And you’re in the doctor’s office, awaiting your first Lupron injection.
The RN or MD enters the room, holding your Lupron injection, and s/he is wearing a chemotherapy gown, double chemotherapy gloves, and chemical safety goggles. Would you wonder, with legitimate fright, what in the world was going on? Would you hesitate to have something injected into your body which required special handling and protective gear by the healthcare worker in order to protect the healthcare worker from exposure to your Lupron injection? Would you consent to injecting this medication?
Hazardous Drug Classifications
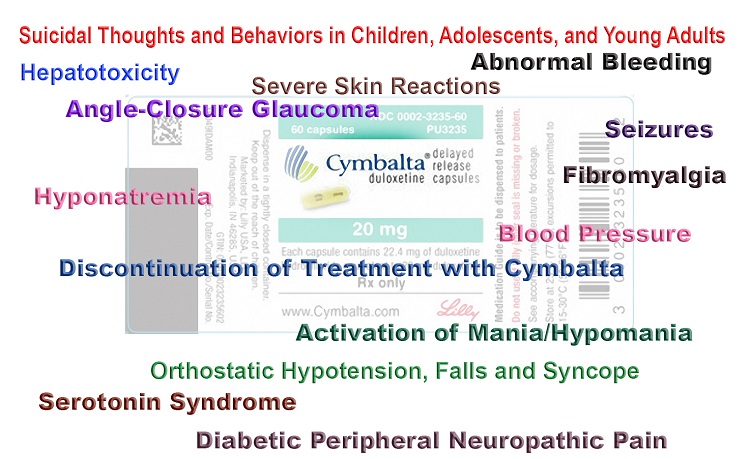
In fact, Lupron, known as an “antineoplastic”[1] and “chemotherapy”, is also classified (along with other GnRH such as goserelin and triptorelin) as a “hazardous drug” by NIH (National Institutes of Health), NIOSH (National Institute for Occupational Safety and Health), and in Lupron’s MSDS (Material Safety Data Sheets); and the handling, preparation, and administration of Lupron by healthcare workers (or consumers injecting at home) requires special protective gear (gown, gloves, and goggles).
Yet, most peculiarly, no healthcare worker (to the best of my knowledge) has ever given a Lupron injection garbed in the required gear. And that would imply not one patient (to the best of my knowledge) has ever received their injection by a gowned, gloved, and goggled RN/MD. If you have received a Lupron injection by a healthcare worker wearing any protective gear, let us know.
How can this be? Several US government agencies, for several decades, have openly identified Lupron as a “hazardous drug” requiring special precautions in its handling, preparation, and administration. Since the 1990s and through the 2000s, I personally have been asking questions and trying to raise the red flag through articles posted on my site LupronVictimsHub. Think about it it for a moment. Shouldn’t the consumer of Lupron be informed of such information? Would you consent to an injection of a hazardous agent for a benign condition from a gowned and double-gloved health worker? I believe that the industry wishes to ignore the fact that Lupron is classified as a “hazardous” drug. As a result consumers have been ‘shielded’ from this, and other, information central to an informed decision.
So these facts have been ‘open’ and ‘known’ for decades, the questions have been asked, “Alerts” have been issued, and still it would appear that entire fields of medicine are in the dark (i.e., gynecology, reproductive endocrinology, pediatric endocrinology, urology) about proper handling and administration of this hazardous drug. As a result, consumers have been denied vital information necessary to form an educated decision about consenting to this ‘treatment’ (trickment).
Impact on Healthcare Workers Unknown
What impact would there be upon healthcare workers (or consumers injecting Lupron in the home) if no protective gear is worn? How important is this issue, since it could be said there have been millions of Lupron injections administered and seemingly there appears to be no evidence of any problem. But the problem is there have been no studies of healthcare workers’ occupational exposure to Lupron in order to answer this question definitively.
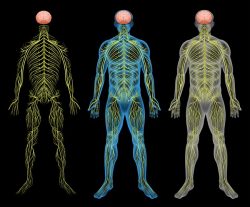
The NIOSH Director has said chemotherapy drugs “can result in adverse health outcomes in workers who are exposed to these drugs, including cancer, reproductive problems, and organ damage when recommended safe handling guidelines are not followed.”
Studies have been conducted showing increased levels of antineoplastic drugs in the environment and in the urine of nurses and other hospital personnel in contact with hazardous drugs or following a spill (here , here and here). Other studies have found a significant increased risk of miscarriages and stillbirths in nurses and pharmacists handling hazardous drugs, and another study of oncology nurses identified that occupational exposure to antineoplastic drugs may reduce fertility and increase poor neonatal outcomes. Unfortunately, these studies and surveys do not appear to have included Lupron and identify only a few or the ‘top 20’ antineoplastics.
A search of PubMed for ‘Lupron leuprolide’ and ‘occupational exposure’ yields “no items found”. In light of Lupron’s common use and the apparent long-standing disregard of safe handling techniques, there is no legitimate excuse for the lack of investigation into potential occupational exposure. (A search of PubMed for “Lupron” [as of 8/5/16] displayed 3,122 published articles.)
NIOSH Alert
The 2004 Alert by NIOSH (as well as in subsequent NIOSH lists), identifies that leuprolide (Lupron) has been included on NIOSH’s “hazardous drug” list because of its “carcinogenicity, teratogenicity (reproductive and developmental toxicity), and genotoxicity” properties (see pages 32, 37). This Alert (and subsequent NIOSH lists) advised “[w]hen a drug has been judged to be hazardous, the various precautions outlined in this Alert should be applied when handling that drug” (see page 33) (emphasis mine).
There are no safe exposure levels for carcinogens. For nearly three decades “authoritative guidelines developed by professional practice organizations and federal agencies for the safe handling of these hazardous drugs have been available … [yet] [d]espite the longstanding availability of safe handling guidance, recommended practices are not always followed …”.
Lupron labels completely fail to identify the need for protective gear when handling, preparing and administering Lupron. The manufacturer of this drug appears to have recognized the need to attempt to reduce occupational exposure, as evidenced in some formulations, by the manufacturer’s use of an engineering control in Lupron syringe luer-lock system. Clearly education and training on the hazardous nature of Lupron and need for personal protective equipment has been universally lacking, and much more information and instruction is necessary.
It would appear to be time to euphemistically ‘take the gloves off’. A ‘fast-track tutorial’ for healthcare workers (and consumers in the home) who are handling, preparing and administering Lupron/GnRHa needs to take place immediately (it’s time to ‘put the gloves [etc.] on’). The label should be revised to include, plainly and unmistakably, language identifying it as a “hazardous drug”, with specific delineation of safe handling technique and personal protective equipment required for its handling, preparation, and administration. Surveys should be conducted and studies initiated to evaluate the health and reproductive status of persons who, for years, regularly handled, prepared and administered Lupron without using any personal protective equipment. Finally, professional practice organizations should be made to explain how the proper handling of Lupron has ‘fallen through the cracks’ for 30+ years, placing healthcare workers (and consumers injecting Lupron in the home) at unknown and unnecessary risk.
For further details and additional background information, please see my recent article ‘Decades-Long Universal Disregard for NIOSH Precautions During Handling, Preparing, and Administering the “Hazardous Drug” Lupron’.
[1] Lupron is most often referred to as a “Hormonal Antineoplastic”. However, it has also been classified (by the deHaen Modified American Hospital Formulary Service Therapeutic Classification System) as an “Antineoplastic/OTHER” (emphasis original). This deHaen Classification System further delineates its categories numerically, and Lupron’s “Antineoplastic/OTHER” classification is assigned the number “10:00.12”, as opposed to the deHaen’s “Antineoplastic/Hormone” classification number of “10:00.10”. (deHaen Modified American Hospital Formulary Service Therapeutic Classification System, New Drug Analysis Europe and Japan, 1995, Vol. XIV, p.16). I remain unable to define “OTHER”, however other drugs carrying the “10:00.12” classification include Interferon.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.












The nurse who gave me my Lupron injection brought it into the room in a yellow plastic bag marked CHEMO and put on double gloves. But no gown or goggles. I had asked my doctor if it was chemo when my pharmacy told me they couldn’t order it in but my doctors assured me that it was not. That it was sometimes used to supplement certain chemo therapies but that on its own and at such a low dose it was not chemo. To me this sounded like I metaphorically had a duck that they were trying to convince me was a chicken. I honestly felt like I had no other choice. My gyn didn’t want to do another laparoscopy, he told me a hysterectomy at 28 would basically guarantee I would die 20 years prematurely. Lupron was the only thing he suggested and my regular doctor supported that recommendation and reassured me that it was safe and that I would be ok. That most women don’t have any side effects and if if did they would be minor. Anyway, when I told my doctor about the double gloves, chemo bag, and “what to expect” handout from a chemo website, my doctor said the administering nurse (a chemo-nurse) is supposed to be more careful than that to not scare people for no reason. But she couldn’t or wouldn’t give me an answer when I asked why her nurse couldn’t do the injection instead of me having to go to a chemo-nurse. It took barely a week before my hair started falling out among a lot of other moderate to severe side effects that they specifically told me couldn’t happen. When I complained about them and said “I thought this wasn’t supposed to happen” she responded with “changing hormone levels can be unpredictable and can affect all areas of the body. Hang in there” and started me on an estrogen replacement pill. Doctors don’t just not tell you the whole truth. They lie.
Jacci B,
They do “lie” – and unfortunately you had to find this out the hard way (which is the same way many other lupron victims have learned that lesson). Your doctor’s statement that the chemo nurse is “supposed to be more careful and not scare people for no reason” in effect addresses the real problem: the ‘chemo nurse’ (*and* prescribing doctor) had a duty to educate the patient about the risks of a known hazardous drug – and not try to diminish or dismiss Lupron’s hazardous status – which clearly happened in your case.
Thank you for leaving this comment about your experience – this is the first time in all my years of following this issue that I have heard of any woman receiving Lupron with the use of any type of protective gear for the professional.
The Lupron injections I received were administered by a nurse who did put a gown on and gloves. That seemed strange and wasteful
Here’s an acceptable explanation as to why the otherwise profit savvy Fertility Industry would make an exception and forgo the potential little earner of daily injection visits. When your IVF expert tells you to ignore all warnings you may have heard rumored, because in the right hands Lupron is completely safe, s/he’s probably right: Letting patients handle and self-inject this poison suddenly makes a lot of sense. And here we all believed their explanation, in awe of their willingness to accommodate patient convenience.
If we consider that all drugs used during IVF are marked pregnancy x, that is, they are toxic and hazardous to a growing fetus, this type of treatment is probably not suited to intelligent and thinking women; so long as they are adequately informed. However, through clever marketing, selective media releases and deliberately withholding and/or denying its true risks, IVF and the associated use of high doses of fertility drugs became widely accepted in spite of the first successful procedures, initiating public acceptance, involving no fertility drug at all.
The more drugs a woman takes, the more unlikely it becomes for her body to regain its natural healthy chemical balance to perform the functions required for conception. Anyone wanting a healthy conception must look to women who have accomplished this in the absence of chemical intervention. Whole books were written on how to successfully combat any condition, from endometriosis and PCOS to unexplained infertility, to conceive naturally – even at “advanced maternal ages”. Women with tubal pathology might consider reconstructive surgery, before permanently shutting down their systems with Lupron or any other GnRHa, like Buserelin (Suprefact, Suprecor), Goserelin (Zoladex), Histrelin (Vantas, Supprelin), Nafarelin (Synarel), Triptorelin (Trelstar, Decapeptyl, Gonapeptyl). Look for “-relin” and say NO. Modern assisted reproductive technologies comprise a flourishing and reckless industry that has slowly gone collectively insane by actually starting to believe their own dangerous lies.
It is a great pity that so many highly intelligent and educated individuals have now assumed the roles of enablers, supporting ART procedures with their “natural” approaches, when they really should know better. An active healthy lifestyle, including fertility diet and exercises will not make a difference to women whose systems have been chemically hijacked, in fact, becomes impossible; and ovulation charting becomes pointless for those who lost their periods outright, following chemical sterilization. Taking a slice from that pie must be very tempting.
Anyone who doesn’t want a safety goggled and double gloved and chemotherapy gowned someone anywhere near them should think twice about whom they allow to be involved in the conception of their child. That wheezing mummy, slowly shuffling towards them waving a syringe, is completely harmless compared to the confidently smiling IVF expert, claiming treatment safety and boasting his or her “successes” (emphasized, as the public still knows very little about the long-term health outcomes for mother and child – most likely still childless mother).
Cherish your infertility, which is more likely to be transient than IVF success: after IVF you may be permanently sterile. When biased experts tell you, you’ll never conceive a child without IVF, don’t go into shock (they need you to feel helpless to proceed), but inform yourselves and prove them wrong. That biological clock may be ticking, but not at the accelerated rate the experts claim, and it may go into overdrive following GnRH-a (-relin) drugs. When it comes to IVF, don’t walk away: RUN.