Rheumatoid arthritis is an autoimmune disorder which causes the body’s immune system to attack the joints, resulting in pain and swelling. About 1.3 million people in the United States have rheumatoid arthritis, and of these, nearly 75 percent are women. “In fact, 1–3 percent of women may get rheumatoid arthritis in their lifetime. The disease most often begins between the fourth and sixth decades of life, however, RA can start at any age.”
At this point in my research into hormonal contraceptives, any disease that affects women so much more drastically than men I find suspicious. While reading the Nelson Pill Hearings (NPH), the testimony of Dr. Giles Boles, a professor of internal medicine, caught my attention. He was discussing oral contraceptives and rheumatoid arthritis. Like diabetes, this is another connection I had never heard about before.
At the hearings, Boles describes a 24-year-old woman who was experiencing mild rheumatic symptoms. After running some tests, she showed three abnormalities commonly associated with lupus. She had been taking oral contraceptives for 8 months and was on no other medication. “She was advised to discontinue her oral contraceptive therapy and within 6 weeks all of her laboratory abnormalities had disappeared.” Doctors continued to monitor her for over 2 years and she remained disease-free.
He also spoke about a two-year study published in 1969 that showed rheumatoid arthritis in women taking oral contraceptives increased more than 50 percent. Another study from the same year reported that 22 women with rheumatic symptoms had their symptoms diminish or disappear after discontinuing the pill (NPH page 6089).
That study, which was originally published in the British medical journal Lancet, was also discussed in Barbara Seaman’s book The Doctors’ Case Against the Pill (page 122):
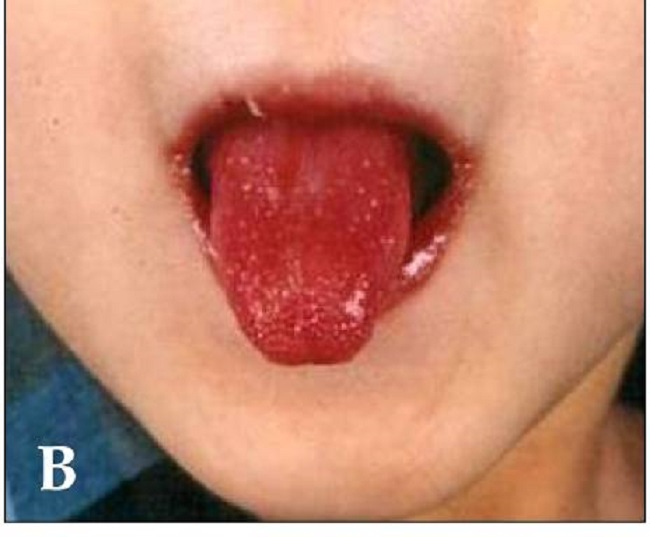
“Over the past three years we have seen 22 young women who… after beginning oral contraceptives developed [arthritic symptoms]. The joint swelling was usually limited to the hands. On cessation of the oral contraceptive, the symptoms disappeared… We specifically inquire as to the use of oral contraceptives in all young women we see with rheumatic complaints…”
In researching the connection further, my first stop was the Centers for Disease Control. On their page for rheumatoid arthritis under “Risk Factors” is the following:
Oral Contraceptives (OC): Early studies found that women who had taken OCs had a modest to moderate decrease in risk of RA. However, most recent studies have not found a decreased risk. The estrogen concentration of contemporary OCs is typically 80%-90% lower than the first OCs introduced in the 1960s. This may account for the lack of associations in recent studies.
This seems very odd to me for a few reasons. First of all, if oral contraceptives decrease the risk of rheumatoid arthritis, why put it under “Risk Factors?” Secondly, though the “early studies” being cited are from 1993 and 1989, they point to the higher concentration of estrogen from pills in the 1960s as a reason for the conflicting information. Yet in 1970, Dr. Boles testifies about a very real connection between rheumatoid arthritis and the use of oral contraceptives.
Rheumatoid Arthritis on the Rise
“The incidence of rheumatoid arthritis (RA) in women has risen during the period of 1995 to 2007, according to a newly published study by researchers from the Mayo Clinic. This rise in RA follows a 4-decade period of decline and study authors speculate environmental factors such as cigarette smoking, vitamin D deficiency, and lower dose synthetic estrogens in oral contraceptives may be the source of the increase.”
Yet this WebMD article discusses a small German study that showed that oral contraceptive use could ease some symptoms of RA. Incidentally, the article also points out, “certain patients with inflammatory arthritis may increase their risk of blood clots by going on oral contraceptives.” This statement makes it seem that only some women are at an increased risk for blood clots when using oral contraceptives. That’s untrue. ALL women who use hormonal contraceptives are at an increased risk for blood clots.
While the German study was small and focused on symptoms, a meta-analysis of 17 studies showed no “protective effect of oral contraceptives on the risk for RA in women.”
Perhaps even more strange are the findings presented at the American College of Rheumatology Annual Meeting in Boston in 2014. The study presented there showed that choice of contraception may influence rheumatoid arthritis autoimmunity risk, with the biggest risk coming from IUDs (intrauterine device), though the research findings don’t specify whether patients used a copper IUD or a hormonal IUD.
According a meta-analysis by Hazes and van Zeben the overall unsatisfactory state of studies relating RA to the contraceptive pill suggest
“that oral contraceptive use may in fact be a marker for some other causal factor.”
Another article by William H. James from the Annals of Rheumatic Disease describes the problem with determining the connection between oral contraceptive use and rheumatoid arthritis:
“Over the last decade a dozen large scale studies have offered strikingly dissimilar conclusions on this possibility. An international workshop was held in Leiden in 1989 in an attempt to reach a consensus. It is not unfair to comment that consensus proved evasive.”
Is Rheumatoid Arthritis Connected to Hormonal Contraceptives or Not?
In 1970, the research clearly showed a connection between rheumatoid arthritis and hormonal contraceptives. Further research confirmed that. Then other studies attempted to demonstrate that the pill mitigated symptoms, while a meta-analysis showed no protective effect. Yet recent findings show an increased risk for women who use IUDs. In all of the recent research, the only consensus seems to be that there is no consensus.
The bottom line is that evidence about the connection between rheumatoid arthritis and hormonal birth control is inconclusive at best, incoherent at worst, and sometimes downright contradictory. Once again, I have to ask why. Why were there not conclusive studies conducted immediately after the 1970 Congressional hearings? Who gains by there still being confusion about this issue? Who loses? That one I can answer; women lose.
Real Risk Study: Birth Control and Blood Clots
Lucine Health Sciences and Hormones Matter are conducting research to investigate the relationship between hormonal birth control and blood clots. If you or a loved one have suffered from a blood clot while using hormonal birth control, please consider participating. We are also looking for participants who have been using hormonal birth control for at least one year and have NOT had a blood clot, as well as women who have NEVER used hormonal birth control. For more information or to participate, click here.











WOW!! I am in shock reading these posts. I too fall in the same catagory of having paint in joints and stiffness after GYN stopped my BC Pill to see if I had gone thru menopause. I am 52 and had never suffered joint or muscle issues my entire life UNTIL going off Oral birth control. I used BC pills for 30 years and after stopping use my quality of life has diminished. I was physically active, a non smoker ever and not over weight and white. I added the white because in the studies I have read about women that have extra harsh menopause symptoms were those that smoke were obese and black.
Anyway still not getting and answer to the fact that if Oral birth control pills could cause these particular side effects from using or stopping using after decades of use without being a high risk factor or a smoker mainly to increase your risks of stroke or blood clots etc. but nothing about muscle stiffness and extreme joint pain then I think a fat lawsuit is in order AS WELL as studies done in THE USA about long term effects not mentioned from taking BC pills.
If you read all the other comments before mine in this article all of us women have one thing in common we took oral birth control for years and stopped then experienced similar if not the exact same problems which was the onset of joint paint and muscle stiffness.
I believe we should get as many women as we can to come forward to leave comments about this issue and combine our complaints to get action in this.
If I had know taking BC pills for 30 years and stopping would cause this HELL I would never have taken them in the first place.
Please leave a comment and share your story. Let’s do something about this together.
I’m 53 years old and been on the birth control pill for about 22 years. I really never had any problems on it and my periods were light to medium, same time every month, so for me I continued on it until my gyno recommended I get off of it to see if I was menopausal. He said we would never know if I was in menopause if I was continually getting my period every month. So I agreed. He told me he could wean me off of it by giving me a lower dose pill but for some crazy reason I said no I’ll do it cold turkey. Well, I stopped taking the bc pill in November after my period and probably around middle of December I noticed my joints and muscles were very stiff and something just didn’t feel right. It never seemed to go away. The joint pain was getting worse. My feet hurt. Never had feet pain in my life. It felt like I was coming down with the flu because my body just ached all the time. I felt weak. Also, my right hand and sometimes left hand would fall asleep every night. It’s so bad that I wear a hand brace to help. It’s fine during the day but goes completely numb at night and wakes me up. I decided in January I would go get bloodwork done. I told my primary that the only thing that changed was getting off the bc pill. She said if the bloodwork came back ok it was probably my body going through the withdrawals of the bc pill. My bloodwork came back normal. Only thing flagged was I was taking too much vitamin D and she did the test for inflammation to rule out lupus etc. Well, my inflammation was at a 31 normal range is 1-10. Not horrible. So I thought ok I can do this knowing that it’s most likely the withdrawal of the bc pill. Well,I decided to go back to my gyno last week and showed him my bloodwork and asked him his thoughts. He thinks that I’m menopausal because I haven’t had a period since getting off the pill in November. He told me he could put me on hrt therapy or on a lower dose bc pill and hopefully that would help my joint pain. I decided I shouldn’t have to live like this at 53 so I am back on the bc pill(lower dose). I’m not sure if I made the right decision, I just want to feel better. I’ve also added supplements like turmeric and magnesium during this time to see if they help. I will continue with those as well as trying to eat more anti inflammatory foods. Hoping to see some results soon. Will keep you updated in my journey. Thank you.
I have had lupus for years and my deterioration is on the rise, my friend suggested trying to pull because she swears it caused her to lupus to go into remission. I’ve been in the pull for a little over a week and my systemic pain is the worst it’s ever been. This article is what I needed. Thank you for the work you do. I’ll be stopping and going back to the drawing board with my rheumatologist.
Wow I am not alone. Stopped birth control pill I have been taking since I was15 because of high blood pressure. I am now 49. I wake up or get up from sitting and can barely move. If I knew what I know now I would not have ever put those added hormones in my body.
The pill stopped my RA. First off I was on the pill for around 20 years. Stopped maybe 9 years ago to get a copper iud. Had -for the first time In my life age 40-severe arthritis that would swell my wrists and fingers so bad I couldn’t even drive! Back on the birth control pill since June of this year. No ra! No shots or drugs needed. Doctor said it’s estrogens protective effects on joints. I’m taking the Bc pill until I’m dead/ ( quality of life issue) if I get a blood clot at least I’ll have a full, mobile, pain free life unto then.
I am 32 years old. I came off the pill 2 months ago after 15+ years on it, and 2 weeks after doing so I started getting pain in my right index finger. It soon spread to many joints throughout my body and has persisted for a month and a half. My period has not returned and I am really anxious about all this because I came off the pill to start a family. Far from being able to do that, it feels like I’m going through menopause at 32. Blood tests for RA and inflammatory markers came back negative, as did my thyroid level.
I wake up every morning barely able to bend my right index finger and with aches, pains and stiffness all over. Hot showers and movement throughout the day help a bit but the joint twinges continue and basic manipulation tasks like opening a water bottle or turning a key in a stiff lock are really difficult for my right hand because of that finger. I’m not able to do some of the activities I love like playing tennis anymore.
It helps to know I’m not alone but I’m also really worried that this is happening to me at such a young age right when my husband and I want to start a family. I’m sharing my experience for anyone else out there who might be going through this and feeling alone. You’re not alone!
I started the pill in April and I have been in pain to the point where I can’t dress myself, wipe myself or even dress myself. I feel weak and all my joints hurt, especially my shoulders and my hands.
So far, in the last couple of days, I have been able to move my arms more. I pray that I start feeling better.
I have had an opposite problem. I took birth control pills for years- like 30 yrs. And within 2 mos of going off of them, as I was menopausal, I woke one morning, with my hands so stiff and swollen that I could not even bend them. The shooting pain was unbearable. The pain was in both hands. My feet also were swollen and in pain as well as other joints. I felt like I woke up as a 90-year-old woman out of the blue. I have had $2800 worth of blood testing done everything under the sun including RA and they’ve all come back negative. I am currently on hormone therapy from my gynecologist,Low estrogen patch and progesterone pills 12 days out of the month. The pain has never subsided. I feel as though it is all hormone related, but mine started when I went off of birth control. I am 52 years old. I have thought about going back on birth control pills just to see if it would take the pain away again.
Similar symptoms for me. Was on birth control for about 33 years. Then, about 2 months after stopping, the majority of my joints were painful. I felt like I had become old overnight. It hurt even to cross my ankles. It has gotten better, ever so gradually. My knee is still painful after the onset 10 months ago. I wasn’t sure if it was from going off the birth control or from getting the shingles vaccine, so I never got the booster. I had lots of bloodwork and everything was good and it was not Lyme disease either. I am still baffled and wondering if it was from stopping the birth control or the shingles vaccine.
I was near tears reading yours and Karla’s posts, as both of your stories are exactly mine, and I didn’t think anyone else had gone through what I have. I also went off birth control after 25+ years. After about 2 months, I had severe pain and swelling in my joints. I couldn’t even get my rings over my 1st knuckles. Like you – I felt as if I had aged overnight. After months of testing, and assurances that this had nothing to do with coming off of birth control (even by an Ob/Gyn physician), they assumed it was seronegative rheumatoid arthritis and gave me a prescription for RA meds. Not feeling right about this diagnosis, I got a 2nd opinion from a GYN doctor, who was very convinced that this was indeed related to birth control. As an “experiment”, they had me go back on birth control, and within days, all swelling and majority of the pain had disappeared. Not sure what the plan is now, as I don’t want to be on birth control forever, but sure don’t want to repeat what I’d been through. No one seems to know the best plan forward. Thank you for sharing your story. I’m sorry that you had to go through this as well, but am thankful to have found others out there. Someone should be studying this!
Ladies, just having same problems now. Was on bc pill for 30 years and just went off about 3 months ago. I’m 56. My lower back and hips ache. Sometimes when I’ve been siting and then get up to walk I can hardly move the first few steps. Very unusual for me. Chiropractor seems to help. I had Covid in March and thought maybe it was from that BUT I’ve been thinking more about it being from going off my bc pill. Now I see your post. Guess I should check in with my gynecologist. Think I’d rather take the BC instead of RA meds. Not sure she would agree.
I have the exact same problems and felt it was related to going off the pill, but none of the doctors have agreed with me yet. Was planning to go back on the pill as an experiment as well. In the meantime, have any of you ladies found any solutions? I’m in the process of looking for a doctor that may listen to me.
This exact thing happened to me. I’m 26 and had been on the pill for 3 months and developed major joint paint in my hands and knees. Sometimes I could hardly walk. I also developed bruises on my legs without doing anything. All the signs pointed to RA and my doctor told me to stop taking my OC and after a few weeks I feel perfectly normal again! All my blood results came back negative for autoimmune diseases.
I’m 36 years old I started to take birth control pills about 8 months ago, about a month after I started taking them I woke up with my right hand and my index finger swollen with no explanation of why , the doctor think I have remautoid arthritis I’m still under testing , I had have stopping taking the birth control pills for about a month now I have not seen an improvement on my hand I will keep you’ll updated .
Any updates? I just stopped my pill on Aug 1, 2021. I’m waiting to see a RA doctor.
I started the pill in April and I have been in pain to the point where I can’t dress myself, wipe myself or even dress myself. I feel weak and all my joints hurt, especially my shoulders and my hands.
Hello
Thank you for this article..I am 34 years,and I have polyathritis..I have never taken contraceptives pills in my life until recently that I was told it can reduces inflammation.
I started taken it (combination 3),and I discovered the pain increases day by day..I took the pills for 6days,and I decided to give it a break,to my greatest surprise I feel relieved from my pains..
In my own conclusion, I don’t think contraceptives pills have any effect on arthritis patients.
Thanks
Titilola
I am a 49 year old female, diagnosed in 2008 woth Lupus and autoimmune hepatitis( and now RA). My only symptoms have always been and continue to be extreme joint pain and fatigue.
I have never taken oral contraceptives, but my disease has clearly been triggered by pregnancy and flare ups due to hormonal swings.
My path has been conventional medicine for one year followed by Alternative/natural treatments. I start to feel better, but hormonal swings always set me back.
I know its due to Endocrine disruption from the environment, but no doctor has been able to help me so far.
I am on 3 waiting lists to see a functional medicine doctor with experience in arthritis treatment and hormone treatment.
Its all about the Hormones for me!
Amy~I’m sorry to hear about your suffering. You might try going to UCSF Hospital in San Francisco, California. I’ve heard great things about their doctors & practice of medicine at one of the best teaching hospitals. I wish you the best! Love & light✨ ?✨