It is widely believed that almost no calories are used during sleep. That is incorrect: while the body rests during sleep and energy consumption is not high, it is a long way from zero. A convenient way to measure energy use is known as the “metabolic equivalent” (ME). This is defined as the rate of energy used by a person sitting and awake, the “resting metabolic rate”. A person riding a bicycle may be using five MEs; a runner, nine or more. A sleeping person uses about 0.9 MEs, so we burn calories when we are asleep about 90% as fast as while sitting on the couch watching television.
Energy conservation is important in sleep, but it’s expenditure is still required. It has been proposed that sleep is a physiological adaptation to conserve energy but little research has examined this proposed function. In one study, the effects of sleep, sleep deprivation and recovery sleep on the whole-body, total daily energy expenditure was examined in seven healthy participants aged 22+/-5 years. The findings provided support for the hypothesis that sleep conserves energy and that sleep deprivation increases total daily energy expenditure. I read somewhere that an enthusiastic young astronomer decided that sleep was unnecessary and used his telescope for 13 nights without sleeping during the day. He became extremely ill, thus showing the importance of sleep in survival. The recognition that sleep is one of the foundations of athletic performance is vital.
Research in the general population has highlighted the importance of sleep on neurophysiology, cognitive function and mood. In a post on Hormones Matter, we reported several young people who had a post Gardasil vaccination crippling condition that turned out to be due to thiamine deficiency. All of them had been exceptional athletes and students before the vaccination. We concluded that the brain energy requirement for exceptional people put them at greater risk of succumbing to stress if their capacity for MEs was limited, either for genetic or nutritional reasons. We assumed that their thiamine deficiency before vaccination was marginal and either asymptomatic or producing trivial symptoms ascribed to other “medically more acceptable” causes. The stress of the vaccination required an energy dependent adaptive response that precipitated fully symptomatic thiamine deficiency. You might say that they were “weighed in the balance and found wanting” as the proverb says.
The Stages of Sleep
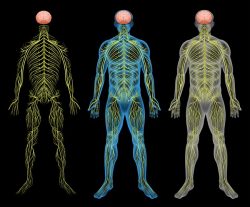
Sleep is a complicated process. The first sensation is known as “sleep latency” and registers the time taken from eye closure to falling asleep. The sleep cycle is then divided into five stages, each cycle lasting approximately 90-120 minutes. Stage one is known as light sleep. In stage 2 the brain is resting the parts used when awake. Stages 3 and 4 are deeply restorative. Stage V is known as rapid eye movement (REM) sleep and may be the most important part. Movement of the eyes behind closed lids is observed. The autonomic nervous system is activated for unknown reasons. It is in this stage when we dream and most sleep disorders occur.
Circadian Rhythm
The word circadian means “about 24 hours”. The circadian clock is a complex, highly specialized network in the brain that regulates its day/night metabolism and is a key for metabolic health. It is modulated by behavioral patterns, physical activity, food intake, sleep loss and sleep disorders. Disruption of this clock is associated with a variety of mental and physical illnesses and an increasing prevalence of obesity, thus illustrating that it is dependent on energy balance (production/consumption). Reduced sleep quality and duration lead to decreased glucose tolerance and insulin sensitivity, thus increasing the risk of developing type 2 diabetes. In other words there is a close link between circadian rhythm and available energy . I have seen patients who were unable to take the night shift at work because they were unable to adapt. The increase in obesity has been paralleled by a decline in sleep duration but the potential mechanisms linking energy balance and the sleep/wake cycle are not well understood. An experiment was reported in 12 healthy normal weight men. Caloric restriction significantly increased the duration of deep (stage 4) sleep, an effect that was entirely reversed upon free feeding.
Sleep Apnea
This condition is fairly common in the United States and is probably generally fairly well-known by most people. The patient stops breathing during sleep and may repeatedly awaken with a start. The disease was discovered because a woman reported that her husband kept waking up with a start because “he was affected by an evil spirit”. Fortunately, the physician took her seriously and it led to the studies that determined its cause. Many patients with, or at risk of, cardiovascular disease have sleep disordered breathing (SDB). These can be either obstructive because of intermittent collapse of the upper airway, or central because of episodic loss of respiratory drive. SDB is associated with sleep disturbance, hypoxemia, hemodynamic changes and sympathetic activation. Brainstem dysfunction combined with heart disease is the hallmark of the thiamine deficiency disease, beriberi.
What that means is that there are two types of sleep apnea. In the obstructive type, the tongue falls back into the pharynx and blocks the airway. In the one where there is loss of respiratory drive, the centers in the brain stem are compromised. It is these centers that completely take over the control of breathing when we are unconscious as in sleep. If their supervisory mechanisms fail, breathing ceases. Carbon dioxide concentration increases and stimulates the brain controls that restart breathing. Occasionally these mechanisms are so sick that breathing does not restart. Hence a form of nocturnal sudden death follows. When we are awake we can override these centers and control our breathing voluntarily. Obesity and obstructive sleep apnea have a reciprocal relationship depending on the regulation of energy balance. When I was in practice I treated several patients with sleep apnea using large doses of thiamine. Because of this I hypothesized that the association of dysautonomia with so many different diagnoses is because of loss of oxidative efficiency and subsequent disorganization of controls that are mediated through the limbic system and brainstem. I came to the conclusion that energy deficiency in the brain was the core issue.
I recently had a letter from the parents of a then five-year-old child who came under my care 35 years ago. She has a genetically determined disorder that affects energy balance and I had treated her by dietary restriction and providing non-caloric nutrients. They informed me that she was doing very well. The condition is known as Prader Willi syndrome, a terminology that indicates that nothing was known about its cause when it was initially described. Today, 10 studies have provided evidence that total energy, resting energy, sleep energy and activity energy expenditure are all lower in individuals with this syndrome. Dietary discipline and nutritional supplementation had paid off.
An Explanatory Analogy
You may think that comparing the human body with an automobile is manifestly absurd, but the principles that I will use in the analogy are simple.
Fuel
First of all, both use fuel: gasoline is the fuel for a car, but it must be calibrated to the design of the engine, giving rise to the gasoline choices at the pump. Although different forms of human food may be compared to gasoline choices, the primary fuel for our cells is glucose and this is particularly true for the brain. Glucose, a carbohydrate, can be synthesized in the body from other components in the diet and different diets are sometimes used therapeutically. Unlike the car, the human body must derive its “spark plug” from the food and is the basic reason why organic, naturally occurring, food is a necessity. The food industry cannot imitate or replace it.
Engine
The engine in a car burns gasoline to create energy. It requires spark plugs to ignite the gasoline and waste gases are eliminated through an exhaust pipe.
Every cell in the human body has an “engine”. Without going into details this is known as the Krebs cycle (named after its discoverer). Its objective is to produce energy and glucose has to be “ignited” (oxidized). The oxidation process, while releasing energy, gives rise to carbon dioxide (the “ash”) that is eliminated in the breath. Energy is stored in an eletrochemical form known as adenosine triphosphate (ATP).The nearest parallel would be a battery. It releases an electrical form of energy that is then used for function. Whether we like to recognize it or not, we are electrochemical machines and the only way that we can preserve or retrieve health is by furnishing the complex of ingredients that enable food to be converted into energy.
To continue the analogy, when you put your car in the garage and turn off the ignition the car is technically “dead”. Obviously, we are unable to do that with the human body, but let us make a simple comparison. Supposing for some reason it was desirable to keep the car “alive” when it was in the garage. The engine would continue to run and it would be consuming fuel. Because the body requires energy to remain alive, the “engines” have to continue running, even when we are asleep. This does make sense for the consumption of energy when we are asleep———it keeps us alive !
Transmission
The energy developed from burning gasoline has to be transmitted to the wheels in order to produce the normal function of the car, which is the ability to move. The transmission is a series of levers that are interconnected.
The same is true in the human body, but it is biochemical in nature. A series of energy consuming enzymes use the protein, fat and carbohydrate to build the diversity of tissues that make up the body. Throughout life, cells are destroyed and replaced, so this is a continuous process of energy consumption and repair. Every physical movement, every thought and emotion, consumes energy. Like the transmission in the car, the energy produced by the citric acid cycle engine is consumed in every movement of the body, every thought occurring in the brain and every emotion.
Chassis
The body of a car is just a container on wheels designed to carry around human beings. Its sole function is to move and until we have driverless cars a human being must be the driver.
In comparison, the body of a human being is merely a chassis that carries the brain around. It might be said that the brain can be compared with the car driver and every function of the body is under the command of the brain. Another analogy that I have used is an orchestra where the brain is the conductor and the organs are banks of instruments in which the cells come under the command of the conductor.
Putting It All Together
The 2019 Nobel prize has just been awarded to three scientists who have discovered how our body cells respond to low concentrations of oxygen (hypoxia). The reaction of medical scientists is very positive since this discovery will certainly be applied to the treatment of many diseases. Apparently scientists are already trying to find drugs that will influence this effect. For example, it has long been known that hypoxia will introduce inflammation. My forecast is that the use of nutrients will often correct the genetics by epigenetic mechanisms and this is already under way.
I found the Nobel prize extremely interesting because of a little-known phenomenon that was described by the early investigators of the vitamin B1 deficiency disease, beriberi. They had found in this disease that the arterial concentration of oxygen was low while the venous concentration was relatively high. Arterial blood carries oxygen from the lung to all the tissues of the body. It has to be unloaded into the cells that then use it to produce energy. The venous blood then returns to the lung to be loaded again with oxygen. A relatively low arterial oxygen reflects an inadequate loading at the lung tissues, while a relatively high venous oxygen indicates poor utilization by the cells to which it is delivered. This means that thiamine (vitamin B1) is an essential catalyst in the delivery of oxygen to the tissues. Its deficiency induces gene expression similar to that observed in hypoxia and has been referred to as a cause of pseudo-hypoxia (false hypoxia).
The heading of this article is that sleep requires energy, but I am making the case that being alive and well simply means that oxygen is being consumed efficiently, as long as the “blueprint” of DNA is healthy. It strongly suggests that hypoxia and/or pseudo -hypoxia are the underlying causes of disease and may explain why thiamine and its derivative are such important therapeutic agents.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Image by freestockcenter on Freepik.
This article was published originally on October 14, 2019.















My boyfriend has just been diagnosed with diabetes, high blood sugars, high cholesterol. He is about 80 pounds overweight. He eats a health diet, not much sugar and he is muscular but carries the weight in his abdomen. He was in a high stress law enforcement position for 25+ years but has since left that for the past 5 yrs. He was in GATE as a child-so high intelligence. I see what he eats, not much more than me, but his body seems to store everything he eats. I sometimes comment that it seems that his body thinks it’s starving. He doesn’t dream but usually sleeps all night. He also has sleep apnea and uses a machine, you can hear his breathing pause. He’s tried time restricted eating and other food plans and he always sticks with them. He loses about 5 pounds and then it all stalls out. He works out by lifting weights and looks fit aside from his belly. He was on lots of antibiotics as a child and had asthma. He has exercise induced asthma. He is on no medication and takes a multi b, vitamin d and other misc supplements. I’m thinking it’s a thiamine problem.
Hello!
I have been suffering from major depression, Anhedonia, emotional flatness, anger, major insomnia, depersonalization and chronic fatigue. None of these issues responded to any medication or supplements long term. After advanced testing of my CSF, it was found that I was very low in the enzyme BH4 and low in serotonin and dopamine metabolites. I was told this explains by symptoms, but, after a long time on BH4 replacement therapy… I would only see improvements for a week or so after starting or raising a dose that would then go away. We tested my CSF for amino acids as well, along with b6 which all came back normal. I was instructed to take B1 to help repair the brain from any damage which I have been taking.
Where would you turn if you were me? I have not noticed improvement from the BH4 or B1 (500mg a day). I wish we would have tested my CSF for all B vitamins and essential elements… as I heard complex diseases might be caused by these deficiencies in the brain while our serum levels are normal. We are not sure the cause of the BH4, it could be oxidative stress, it’s really unknown.
Where would you turn if you were me? I was told BH4 is the only solution for my condition.
Dear Dr. Lonsdale
Thank you.
Is it possible to work out a list for functional testing of a l l enzymes of the Krebs-cycle, and the labs able to do that/or the method necessary to measure correct?
When I was 22, I was running 8000 meters with 130 meters of height-difference in 29 minutes relatively comfortable (weight 95 kg)
My anaerobic threshold was around 17km/h at that time (Conconi indoor-test)
I don’t know, how much Lactate I had , and how many Watts per kg this was.
I just know, that I now make zero progress with cycling-training (age 49), at only 0.6 W/per kg weight/ 1.5 mMol Lactate.
I think, HIF 1 is probably upregulated, it feels like hypoxia .
I m taking 3xThiamax 25 mg daily, with additional 3g Magnesiumphosphate
Phosphate is low, and muscle cramps occur often.
I had psychosis 4 times 15 years ago. The last episode disappeared after 3-4 hours after taking around 4 grams of calcium magnesium pills.
Is it possible, that I need more magnesium than Thiamine for some reason?
Dr. Lonsdale,
I have been dealing with complex sleep apnea for a few years now but it seems to be more central recently (and getting worse). I cannot tolerate CPAP due to aerophagia, even on the lowest therapeutic setting (woke up during the night to burp and didn’t get good sleep). My sleep doctor had little alternatives to offer me except for a mouthpiece or a procedure to implant a device to stimulate breathing. I don’t like that idea at all.
I started supplementing recently with benfotiamine and allithiamine but so far, it doesn’t seem to be helping. I also take magnesium (to include the threonate version). Does it take time to start seeing results in my sleep quality?
Thanks!
Kelly
Hello, One of my friends only had success with 1000 mg of thiamine HCl for central and obstructive sleep apnea along with an activated b-complex. He tried allithiamine and benfotimine and neither of them were effective enough to put a stop to the apnea, only the thiamine HCl would stop it.
I have been taking the thiamine along with magnesium and a multivitamin for almost 3 weeks now and I think I might be suffering from severe paradox. At first I was actually feeling much better. Suddenly I developed severe palpitations, an irregular heartbeat, an extremely painful pinching feeling in my chest and overall spacey feeling and this has been continuing nonstop for almost 4 days now. I went to the Dr. and said that if she didn’t know my history she would have immediately wanted to send me to the emergency room because of how my heart was beating. Is this normal/safe? I am desperate to get better but the paradox is excruciating. I was also wondering if in a severe case IV vitamins would work better or help get over the paradox more quickly. Any advice appreciated, thank you.
What amazes me is that question after question is a repeat. My question in response is this: if you have been sick for years (genetics and pollution aside) because of your diet, how can you possibly expect to take a few pills and get well? If your symptoms had been treated properly when they first appeared, your return to health would have been rapid and easy. Over the years, you have been suffering from energy deficiency and you can expect some structural damage to your affected cells. Those cells have to be reconstituted and obviously it takes time. When you start taking thiamine and magnesium, your symptoms are accelerated paradoxically and you have to wear through this until paradox gives way to improvement. Nobody can predict how long this paradox will last but I usually state that it can last for a month or so. Lastly, I would advise anybody wishing to post a personal history to read the many different posts on this website that are capable of answering your question. It is always surprising to me to see how repetitive these histories are.
Just hoping this might help, I could not take magnesium without also taking calcium citrate, because the magnesium helps calcium go to the bones and I was vitamin D deficient so was not absorbing enough calcium from my diet so the magnesium would lower blood calcium and cause low calcium symptoms (heart arrhythmias , even to the point of mild heart failure but it all corrected with vitamin D and calcium supplements added. Best wishes
Commenting on the stages of sleep, studies show that when people are not allowed to enter into REM sleep, they are unable to remember things they were taught before they went to sleep. This study was done by the National Institute of Neurological Disorders and Stroke in 2007. During this REM sleep, your brain uses almost as much energy as it would if you were awake! I am a sleep junkie as well!
Also, that link is broken in the stages to sleep section for the “divided into five stages” article to better-sleep-better-life.com
After I withdrew off an antidepressant I had been on for 13 years (I started at age 5 for mood issues, who knows maybe that was from vitamin deficiencies too) I developed many of the symptoms you talk about, mostly chest pain/palpitations/huge heart rate and blood pressure change when standing up/lightheadedness/severe muscle pain to an extreme degree and was basically nonfunctional for years. I was also anorexic as a teenager and even though I gained a lot of weight during this illness I never felt like I recovered from the deficiencies that must have incurred and my body is incredibly sensitive to any change in diet/food intake. I’m 23 now and have gotten a little better through a low sugar diet but still have days where I’m just exhausted with discomfort and all these symptoms not able to do much.
I don’t exactly know if thiamin deficiency is my problem but I am starting to supplement it, another issue is that I have hypersensitivity to almost every supplement/vitamin, is this typical? I can get increased palpitations and all my symptoms become exacerbated, it’s very frustrating. My parents have taken me to literally dozens of Drs and none have a clue what’s going on. This has been so sad for me to lose so many years and I’m just scared that more supplements are going to make me feel worse. A question I also had is, do you need to avoid coffee and tea entirely during this process because they prevent B1 absorption? I want to thank you for all the work you’ve done and even if this doesn’t help me I have learned a ton from reading this info.
This is yet another story that reflects on the appalling ignorance that seems to affect virtually the entire American medical profession. I believe that there are thousands if not millions of people who are languishing with these symptoms and are being discarded as psychosomatic “bad patients”. She had medical issues as a child and I suspect that this was a reflection of bad diet by her mother during pregnancy, or it may be a genetic factor. She developed heart palpitations, rapid heart rate, changes in blood pressure, became lightheaded, developed muscle pains and became anorexic and has suffered from these symptoms for many years. What a disaster! This has all the hallmarks of beriberi. Notice that she complains of hypersensitivity to the intake of all vitamins and is obviously experiencing a typical paradoxical reaction. I also strongly suspect that this individual is highly intelligent, because as I have repeatedly stated, the more intelligent the brain, the more energy is required to run it and thiamine deficiency simply reduces the energy required, particularly to the brain. Your thiamine supplementation should be kept relatively low, say 100 mg a day, together with 125 to 250 mg of magnesium and a well-rounded multivitamin. Keep the dose low until the paradoxical reaction begins to give way to improvement and this may last as long as a month or so. You can then titrate the dose to the symptom improvement. I must emphasize that reading this comment requires a drastic change in thinking about the REAL cause of disease. With insufficient energy synthesis in the body/brain combination to meet the demands of daily living, the brain signals distress to its owner. The commonest symptom must surely be fatigue. The word beriberi is Chinese terminology. Translated it means
“I can’t, I can’t”
Thank you so much for your response. So many more people should have access to this information! The world needs more doctors like you, and you are 100% correct about how rampant ignorance and faulty thinking is among US healthcare. Most physicians aren’t interested in finding the cause of a patient’s complaints (or they believe the symptoms are psychosomatic, or just ‘random’ and a part of life), only covering it up with pharmaceuticals. A total change in mindset definitely is needed when it comes to disease, both physical and mental. Labeling different symptoms as thousands of different unrelated diseases hasn’t helped make any progress or ease peoples’ suffering to a meaningful degree. I believe in the future we will look back on this time as one where we totally misunderstood the cause of disease/dysfunction and overcomplicated things without seeing the big picture.
I’ve spent years trying to find answers to all this and have always believed that my symptoms were related. I can’t tell you how thankful I am to have come across your work, thank you again.
I agree with you completely. I am appalled by the number of people posting a similar history on this website. I suggest that anyone wishing to post their personal history should scan the many posts that exist on this website that may well answer the question.
Yes, I would guess that this is a severe paradox and you simply have to just wear it out if you want ultimate success. You do not say anything about your diet and I do not know whether your history is one of poor diet or whether it is genetic in character. There is no gain without pain
Dr. Lonsdale,
Thank you so much for this heartening information. I have depression and anxiety and I literally cannot fall asleep without med assistance. When my depression gets worse, such as during med adjustments, I feel as if I’m smothering to death. I gasp for air but to no avail. The fatigue is crippling. A day feels like a century, a century in a living hell. It’s frustrating because the people around me tell me I’m having an anxiety attack but I know the difference, it is physical. However, not being able to breathe definitely causes some anxiety, no joke! I also have noticed the smothering, lack of breath feeling intensifies after eating sugar. I have been having muscle aches, nerve pricks/tingling, memory/confusion and agitation and lots of allergies. I’m going to give thiamine a try. How does one go about finding a physician who is knowledgeable, as you are, to help sort these things out? I live in Oregon.
Hi Dr. Lonsdale, research seems to suggest potassium is needed when B1 is supplemented especially in wet type beriberi. Do you have clinical experience showing this? If so, do you have a recommended ratio for B1:Mg:K?
I get reactive hypoglycemia when I supplement Mg (I have tried many forms) and it seems to be buffered if I take potassium with it.
Any concerns about depleting B2 and other B-vitamins with higher dose (greater than the RDA) thiamine supplementation?
Thank you!
The present medical model makes it very difficult for people to understand what is being written in these posts. Post after post discusses energy deficiency as the cause of human disease and beriberi is the classic presentation of energy deficiency. It is also the reason that 240 different diseases have been treated with variable degree of success by the use of megadose thiamine. In other words, beriberi is the great imitator. To answer the question here, beriberi can cause a low or high potassium in the blood and is not a reflection of dietary deficiency or excess. Yes indeed, B complex is as necessary as thiamine, but thiamine dominates the picture.It is as though thiamine is the “captain” of a team and although its importance seems to stand out, he other “team members”need recognition.
Hi Dr. Lonsdale, thank you for your response.
How long would you continue high dose thiamine supplementation?
In maintenance, do you recommend periods of higher doses pulsed throughout the week/ month/year?
At what point would you add other vitamins and minerals like Se and Mo in? Do you recommend higher doses of these as well? If so same questions for frequency.
Depends on cause. If it is dietary, depends on degree of reform. If genetic it would have to be permanent. Add magnesium, B complex and a multivitamin–just one dose a day.
Dr. Lonsdale, do you think the reason those with hypoglycemia do not respond to B1 is because of potassium? If not, do you have any other guesses I can explore further? Thank you!
Hi Dr Lonsdale,
I am new to hormones matter, I found out about your fantastic work from the Ray Peat forum. Just prior to that, I came across the study by Italian researchers who gave high dose B1 to 3 cfs/fibro sufferers.
I am 44 with longstanding (20yrs) cfs symptoms, so it grabbed my attention. The very same day, I bought a bottle of 250mg thiamine nitrate from a health store and took 2. It bombed me as you could probably have anticipated. So I halved the dose for a few days, taking before bed (it made me drowsy if taken during day). I slept wonderfully, had great temperatures and experienced very positive moods/motivation and energy. For the first time in years, I could invisage a return to weight training , and simply being able to walk the dog.
After about a week, tired symptoms returned, sleep deteriorated, again I found it difficult to get out of bed, and was experiencing the dreaded air hunger.
Now I knew it had benefited me, but the downward slide was perplexing.
Now having read your redox (paradox) theory, I imagine this is what’s happening. Do you agree that I should continue but with a reduced dose eg 62.5 mg (1/4 tab) daily until improvement, then gradually increase? Does it matter what time of day to take it?
I had some Life Extension Magnesium L-Threonate already so was using that, and a bcomplex. Is there another type of thiamine and/or magnesium that you would recommend?
I have epsom salt baths twice a week also.
Thankyou for your time.
I am sorry, I missed your comment until today. Chronic fatigue syndrome is extremely common and is a reflection of the state of health in America. It is a classic energy deficiency disease and by far and away its cause is poor diet, but in some cases genetics comes into the picture. The fact that you responded to the huge dose of thiamine initially and then fell apart is unusual for paradox. However, you must understand that insufficient research has been performed to throw light on these discussions. You would certainly benefit from reading one of the several books that are available under our name in Amazon books. The timing of the dose does not matter.
Hi Kristy, from our personal experience it is better to use thiamine hydrochloride in this case, i still haven’t tested mega dosages of thiamine TTFD yet (only low dosages) for my wife’s cfs/fibro.
But i can relate a story when we reached 1800mg as per the study my wife was pain free for the first time in decades, and energy improved, when i went to the store to get a larger dosage thiamine i bought thiamine nitrate, all her pain return in 3 days.
So in our personal experience thiamine nitrite was ineffective.
I wrote up what i did you my wife here: https://www.myrandomtips.com/health/how-to-help-fibromyalgia-pain-naturally/
Hello Dr. Lonsdale and Dr. Mars,
I’d like to tell you about my wife’s ordeal. Please tell me if you, or Dr. Chandler Mars, have any idea of what might be of help.
I’m going to try and give all the information I can so that you can try to put the puzzle together.
My wife has been suffering mercilessly with continuous muscle cramps on both her feet. This has rendered her mostly bedridden since December 2018. At times the pain is so strong that she can only cry in despair.
Unfortunately, this has lead us to a kind of catch-22 situation:
Anytime my wife gets out of home she will get worse, and this worsening won’t get better with rest. This means she can no longer go to Doctors appointments with the fear of getting worse.
I’ll go alone to the neurologist and GP appointments. Fortunately, they are very understanding of her situation. Unfortunately, the neurologist considers that my wife’s symptoms are most likely psychosomatic.
At this moment in time, my wife is taking 900 mg of gabapentin and 20 mg of baclofen 3 times per day. (Daily total: 2700 mg and 60 mg, respectively). She weighs less than 50 kg has she has lost her muscle mass from the waist down. Pregabalin at 350 mg gives her no significant relief compared to the 900 mg gabapentin. Sinemet made her feel more anxious and provided no relief. Other anticonvulsants made no difference in her symptoms.
This all began with a missed step while going down a flight of stairs in late March 2018. This led to a sprained ankle that wouldn’t heal. Eventually, she began having spasms and cramping on both feet. These got progressively worse.
At first, she was diagnosed with complex regional pain syndrome. As her symptoms worsen we decided to go to Italy in May 2019 to do Scrambler Therapy (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6336541/)
She got worse.
Then, as she got even worse, the muscle spasms became clearly visible, which led to the diagnosis of dystonia a few months ago.
Throughout all this time, my wife complained that neither I neither the Doctors were paying attention to what she was complaining about.
Basically, she always said:
1- She felt no neuropathic symptoms — no tingling, no electrical shocks, no burning sensations, no pins and needles. Because of this, she didn’t agree much with the diagnosis of complex regional pain syndrome.
2- What she DOES feel is muscle cramps, like the ones that make you wake up at night in severe pain. Except that she will feel them constantly.
3- These cramps get worse with stress and when she is touched in the feet below the ankle. When she on a bad day, she isn’t even able to endure being touched in the leg.
4- Being touched in the feet doesn’t cause pain. It causes spasms. And the spasms are painful.
5- She needs to wear socks all the time and requires an electrical thermal pad on her feet at all times to keep them warm. Her feet are always cold and slightly swollen from the ankle down. But they have always been slightly swollen since I knew her, even long before her fall in March 2018.
Nowadays, she is trying to follow some exercises adapted from the Feldenkrais method. We also have a Feldenkrais practitioner that comes to our home every week to do Functional Integration exercises (it’s a kind of therapy to teach the brain to better use the muscles).
She’s also being followed by an ND from the USA over skype that has prescribed several supplements and a homeopathic remedy.
Sometimes it seems she’s getting better, but then she’ll get worse again.
We’ve tried so many different things that you wouldn’t believe. In the process, we’ve also wasted away our savings and are currently in debt. We’ve even purchased an expensive PEMF device that didn’t work.
Unfortunately, even though my wife is only 22, she has been through a host of health issues that culminated in this terrible situation. Doctors don’t see a relationship between these health issues.
Ankylosing Spondylitis:
– Her father’s side of the family suffers from ankylosing spondylitis. Her father took 10 years to be diagnosed — he had to wait until the lesions were clearly visible on the scintigraphy for Doctors to take his symptoms seriously. This scintigraphy was only performed when the pain on her back was so strong that he had to me removed from home on a stretcher. Nowadays he does therapy with injectable biologicals, which provide minimal relief.
– My wife’s grandfather already has his cervical vertebrae “glued” together.
– When My wife and I got married she begun high-dose vitamin D therapy and that put an end to her ankylosing spondylitis pain until recently. We’ve stopped vitamin D supplementation because due to her current situation, she’s unable to do blood tests as often as she requires, and she’s unable to do exercise (required to promote calcium reabsorption in her bones).
Low-blood pressure:
– when my wife was 14 she began feeling dizzy when standing up, this lasted for a week, always during summer. Then would get better. During this time she felt tired like if her brain was shutting down, she would stay quiet even though she is a talkative person and didn’t feel like herself. The Doctor that saw her was shocked at her blood pressure measurement. Unfortunately, my wife can’t recall anything else from that consultation, except that the Doctor said that “her values were too close together” and that it was very dangerous. She was told to rest for a full week.
– At this time my wife also was suffering from severe acne and was being treated by a host of different creams and antibiotics, including birth control pill. I have no idea of the names of the drugs, though.
– Eventually, she got better, but will still have occasional bouts of very low blood pressure.
– Nowadays, she feels dizzy when standing up, however, this got worse with teh high dose gabapentin and even worse with baclofen. So Doctors associate her symptoms with side-effects from these drugs.
Thyroid:
– Her mother has Hashimoto’s and my wife had two nodules on her thyroid – last time she did an eco was about a year ago. However, Doctors say this is not a problem since her thyroid hormone levels are fine.
Skin:
– She still has acne. It came back after she stopped taking birth control pill. We decided on stopping birth control pill because of all teh side effects.
Breasts:
– When she was 19 she began complaining from pain in her breast. It was found that she had a big lump on her left breast. This was removed surgically and it wasn’t cancerous. She was told not to worry about this and that there was no need to follow up on it.
Cognitive:
– My wife has trouble with words. She is very intelligent, she got 19 out of 20 in Math in some highschool tests but she’s unable to write a full composition in Portuguese without obvious grammar errors which mess up her school grades mean. She thinks in pictures and has trouble finding the right words that describe what she’s seeing in her mind’s eye. She’ll often have to wait for her brain to find the words. She says that she can use correct grammar, but it takes up so much brain energy that she feels wasted afterward.
Sleep:
– She always needed to sleep more than 10 hours a day to be able to function. Sometimes she’ll even have to take a nap. This continued despite her being bedridden. It’s as if her body was unable to do whatever it needs to do while we sleep.
Stress:
– She has very low tolerance to stress. Even before falling, stressful situations made her cry and start to shake. And she begins to sweat a real lot. She will easily get stomach ulcers. Also, the pain and the spasms get a lot worse.
– She also went through bullying at school.
Diet:
– Even though we live in Portugal, when she lived with her parents they ate mostly the American Standard Diet: Their dinner was often icecream and other threats. They ate a lot of junk food.
– At the time of her fall, in March 2018, we were actually trying our best to have an healthy diet. First, we tried Paleo and then vegan. However, we were the kind of vegans that ate mostly potatoes and meat substitutes like seitan. My wife wouldn’t eat brewers yeast because she couldn’t stand the flavor of eating.
Now that my wife is bedridden and I have to make all the food, we eat a lot of tuna, potatoes, codfish, bread, mushrooms and lots of meat, eggs, and pasta. I make all the food and we don’t eat much junk food or sugar but we don’t eat many greens at all.
Medication:
– I don’t know how relevant this is, but she once was prescribed a drug to kill a fungus infection. The Drug was so strong that she was to take only a single pill. It worked and she didn’t had to take it anymore. We don’t know the name of the drug though.
So, here we are, at wit’s end. A panel of Doctors that evaluated my wife decided that she was fit for work so she stopped receiving money from social security a long time ago. Many people around us say that she should “try harder” despite the fact that she gets worse when trying harder…
Unfortunately, people, even Doctors, are very fast at describing symptoms they don’t understand as being psychosomatic as if it meant you could will your symptoms away.
She has begun taking 3000 mg of Thiamine HCl about a week or so ago. Together with chelated magnesium glycinate and a B-complex vitamin by “Dr. Best” brand. (I used what we already had at home because I will be able to buy other things next month) but she doesn’t feel better. In fact, she has been having more spasms… but we never know if it’s from what she’s taking, from stress, diet, from the medications or from trying to walk more than she should (she will walk to and back from the bathroom – about 20 meters)
I’ve also been looking into iodine. Apparently, fibrocystic breast disease is a sign of severe iodine deficiency. And there might be a relationship between iodine and thiamine.
You describe a typical case of energy deficiency from sick mitochondria. She is experiencing what is known as “refeeding syndrome” because she is trying to switch from a prolonged catabolic state to an anabolic state. There is virtual certainty that there is a genetic factor involved. This chaotic state of chemistry in brain is usually diagnosed by mainstream docs as psychosomatic and the more shame to them. She needs a thiamine derivative called Lipothiamine from Ecological Formulas in California and I suggest that you call Bonnie Fields at (international code 1 800 275 3495). She should start on 50 mg twice daily together with 125-250 mg of magnesium taurate or a similar salt. She can also start baths with a handful of Epsom salts in the water. Maintain this treatment until refeeding syndrome (paradox) gives place to improvement. Order of fading of symptoms is unpredictable. Then titrate the dose to symptom relief. There is no toxicity.
Many of her symptoms sound familiar to my symptoms. I had a little relief from thiamine but had a massive improvement when I added biotin. The Drs Best only has 600 mcg. I took 50 mg the first time and got very immediate improvement in symptoms. I had intended to start with 5 mg. Right now I’ve increased to 300 mg and symptoms are further improved.
Obviously, I am not a Doctor and not offering medical advice, just sharing my experience.
Dr Lonsdale,
Thank you once again for a topical and insightful article, tying together theory, clinical perspective, this year’s Nobel prize winners, and more.
My daughter, currently in her mid-20s, has suffered for her whole life with attentional issues more akin to “brain fog” than classic ad(h)d. Several years ago, after reading your research, she began taking 150mg/day of allithiamine, which significantly improved her working memory and mental stamina. However, during the past year she developed an aversion to the light scent of the allithiamine capsules, to the point that she would become quite nauseous. For that reason, several months ago she switched to 150mg/day of lipothiamine, which seems to have solved the queasiness but does not seem to be helping her as much cognitively.
I am curious whether you have seen this differing response before, which I gather is idiosyncratic?
And also, assuming she cannot stomach a return to allithiamine, can you comment on whether a trial of raising the lipothiamine beyond 150mg/day makes sense?
Thanks so much for your work, your book and your continued support of the health-seeking community.
Jacalyn
Lipothiamine is enteric coated and the coating has to come off. That MIGHT be a problem. It is non toxic so the dose can be titrated to symptom resolution.
Thank you Dr Lonsdale. As we titrate up, can she continue to take it all in the morning, or do you recommend splitting the dose? Jacalyn
Split the dose and escalate evenly.
This is a very interesting and important comment. There is a relatively recent discovery of a genetically determined condition called biotin-dependent- thiamine dependent basal ganglia disease. Basal ganglia are a part of the brain. A thiamine transporter is missing. It appears in children and its appearance in an adult suggests another solution. Years ago a researcher by the name of Scriver published a report of a child with a genetically determined carboxylase deficiency that responded clinically to thiamine. Carboxylase is an enzyme that requires biotin, not thiamine, obviously producing a biochemical riddle. Scriver offered an explanation that depended on a thorough knowledge of energy metabolism that is far beyond the scope of my answer here. I don’t know where Terry got the idea of a biotin supplement but he “struck oil!”. I am conversant with the science and it is very intriguing because it suggests that biotin would be an important addition to thiamine supplementation as indeed,Terry found. This once more emphasizes that we cannot diagnose disease without understanding the biochemistry involved. Thank you Terry !