I have addressed this problem before on this website. However, in the Wall Street Journal on Tuesday, March 27: an article appeared entitled “A Study of Sudden Infant Deaths Divides Doctors“. It goes on to say “The finding on sudden and unexpected infant deaths is surprising, says Joel Bass, of the pediatrics department at Newton Wellesley Hospital in Newton Mass”, the first author of the study, who said “that’s more than one newborn baby dying of SUID [sudden and unexpected infant death] a day”. Oddly enough, the article indicates that “among the possible causes, some researchers point to the promotion of certain hospital practices to encourage breast-feeding. But some doctors vehemently disagree with that theory”. Apparently, the theory alluded to the practice of encouraging skin-to-skin care between mother and infant during breast feeding. I had not read the article so I do not understand how this connection was made. What arrested my attention was the reference to breast-feeding, long encouraged by pediatricians as the best way to feed newborn infants. How could skin-to-skin contact be involved? However, an article was published in 2011 in which the author had carefully examined the nutrient content of breast milk in the United States (Shamberger, 2011). It reminded me of an extremely important article that was written in the 1940s.
Breast Milk Toxicity Syndrome
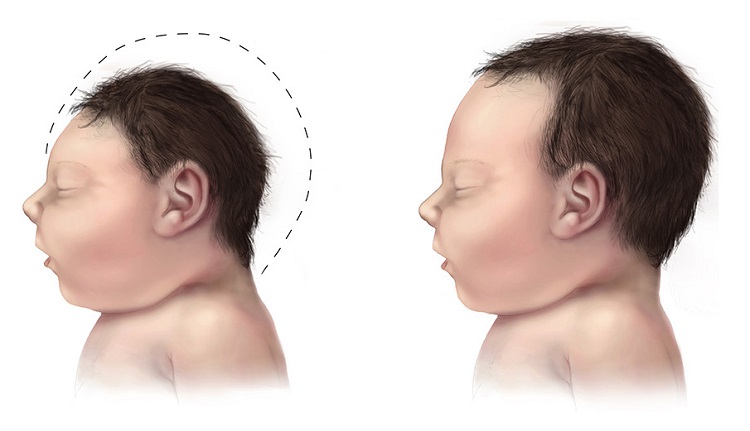
It may be remembered that Hong Kong at that time was a British protectorate. A medical officer of health was sent out from Britain to Hong Kong to investigate a relatively common occurrence of sudden death in breast-fed infants of Chinese mothers. This death commonly occurred between three and four months of age and happened in infants that, from their appearance, were considered to be the healthiest in the family. Fehily, the author, was able to show that the breast milk was deficient in vitamin B1 and it was well known by early researchers of beriberi that this form of infant death was virtually pathognomonic (indication of cause) of the infantile form of this disease. In fact it was well known by these early researchers that there was no other disease of infancy that behaved like this. Fehily herself was struck by the exact likeness to “cot death”, the term used in England for what we call Sudden Infant Death Syndrome in the United States today.
Autism Rates for Each State Connected to Maternal Nutrient Status
The paper published in 2011, referred to above, was in consideration of the cause of autism, not SIDS. The author had studied the rate of autism associated with nutrition. The paper stated that autism rates in the United States are increasing at a rate of 15% per year. The study abstract reported that the design of the study used nutritional epidemiology and an ecologic study design. In other words, he studied public health data and the nutrient content of breast milk. The objective was to try to link the possible cause of autism to nutrition by creating autism rates for the 50 states of America and comparing them with published measures of infant nutrition. These included the duration of exclusive breast-feeding and participation in the Women, Infants and Children (WIC) program. The results were impressive. The states with the highest WIC participation have significantly lower autism rates (P <0.02).
In contrast, there was a direct correlation with the increasing percentage of women exclusively breast-feeding from the years 2000 to 2004. Infants who were solely breast-fed had diets that contained less thiamine, riboflavin, and vitamin D than the minimal daily requirements. Although the author was studying the rates of autism and was not in the least interested in SIDS, his study supports the finding of vitamin deficiency in breast milk, in turn supporting the possible relationship between breast-feeding and SIDS. Of course, the modern medical model would find it objectionable to hypothesize a cause common to two diseases, although both autism and SIDS have a slight male dominance and are diseases that occur during rapid growth, particularly of the brain.
My Particular Interest in SIDS
Many years ago, because of clinical experience, I became interested in SIDS. At about that time, the idea of threatened SIDS had become an acceptable diagnosis, whereas previously it had been considered that the death was truly sudden and completely unpredictable. I can remember two parents who had brought their infant to see me. They had observed him in his crib when he had stopped breathing. When one of them picked him up he started breathing again. They took him to the nearest emergency room where he was pronounced completely fit and the situation was dismissed. The parents were so scared that one of them took turns to sit up all night to watch in case this thing should happen again.
This is exactly the clinical situation that I began to experience with other infants. A monitor had been invented that could be attached to an infant that would sound an alarm if either his heart slowed or his breathing stopped. It had become well-known that picking the infant up or giving him a little slap on the buttock would instantly return him to a normal state (SIDS is more common in male infants). To cut a long story short, my colleagues and I performed a lot of clinical research on these threatened SIDS babies. We had found that a machine known as brainstem auditory evoked potential (BAEP) gave abnormal readings . This strongly suggested that the mechanism was an electrochemical dysfunction in the brainstem. This is the part of the brain that connects with the spinal cord and it contains the controls for automatic breathing. Let me explain this a little.
Most of us are not aware that our essential breathing is controlled by centers in the brainstem when we are unconscious, as in sleep. The condition known as sleep apnea is a failure of this mechanism (apnea is a temporary cessation of breathing). It was during my library research that I discovered the 1944 paper by Fehily. It seemed only to be common sense to look at the possible association of thiamine deficiency as the underlying biochemical cause. We treated several infants with thiamine injections that seemed in every case to stop their episodes of apnea. I received a visit from a university researcher in Australia. His group had been studying SIDS and they had come to the same conclusion. I was so impressed by their work that I took sabbatical leave in Australia with Dr. Read who was the leader of the group. Abnormal brainstem responses in infants at risk of SIDS was reported at about the same time. The authors said that this suggested immature development of brainstem. A recent publication found an association between maternal alcohol consumption and SIDS. The relationship of thiamine deficiency in brain and alcohol consumption is well-known. It is not too difficult to imagine that the concentration of alcohol in the blood of the mother would have an exaggerated effect in the brain of the fetus, perhaps injecting a risk factor for the infant after birth.
Conclusion
Can a parent who has not experienced the sudden death of a precious infant at the age of 3 to 4 months even imagine the horror and the enormous stress imposed on such a parent? We now know that there are quite nonspecific symptoms that may appear in an infant who threatens SIDS. They are sometimes unusually irritable and a “runny nose” may be mistaken for a cold, but such symptoms may be so slight as to be ignored. I must emphasize that the lower part of the brain that organizes automatic body functions, including breathing, is peculiarly sensitive to thiamine deficiency. If the infant is breast-fed with thiamine deficient breast milk as the 2011 study suggests, studies that I have reported here would make sense. Even if only a few of the cases were due to this biochemical phenomenon, giving some thiamine on suspicion can do no harm.
A diet history from the mother might offer clues, particularly emphasizing whether there is ingestion of sugar in all its different forms. If I were a physician in charge of such a pregnancy, I would not hesitate to add thiamine supplementation, starting as early as three months of gestation, as advised in the book written by an American obstetrician/gynecologist by the name of John B Irwin, M.D. He had found that supplementary thiamine removed the complications of pregnancy such as toxemia and even prevented premature delivery. It might well provide a nutritional legacy for the infant. Of course, I am not suggesting that alcohol ingestion by the mother is THE cause of SIDS. However, I am suggesting that the present widespread use of unhealthy nutrition may well be at fault for both SIDS and autism. Genetic risk, coupled with some form of stress (e.g. mattress flame retardants, a cold virus) and vitamin deficiency breast-feeding, might be more or less important individually, or more than one of the three items collectively.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.













Dr Lonsdale,
Would teeth grinding be a symptom of thiamin deficiency?