As a lifelong jock, athletics have been a part of my life for as long as I can remember and though the sports I have participated in over the years have changed (my current passion is powerlifting), the lifestyle has remained the same. I train. I compete (even at the ripe old age of 51), and I train some more. I enjoy training. I enjoy having goals to reach. For those of you who follow this site, you know that I am also an avid researcher. Research is as much a part of who I am as is athletics and so when the two sides meet, I am thrilled. Sometime back, those two worlds intersected. While reading an article about the molecular mechanisms involved in hypertrophy — muscle gain — this sentence hit me like a load of bricks.
“The synthesis of muscle proteins must outpace the breakdown of muscle protein.”
Well, of course it does. Duh, right? This is so obvious in sports medicine, and yet, so underappreciated in conventional medicine. I’ll say it again. “The synthesis of muscle proteins must outpace the breakdown of muscle protein.” In other words, one has to ‘eat to perform’. Think about it for a minute, what is required for muscle gain? Two things: food/fuel and training. Sufficient fuel to promote protein synthesis and sufficient training that breaks it all down. It is a never ending cycle. If you demand too much, if the breakdown outpaces the synthesis, survival mechanisms kick in, muscles eat (catabolize) themselves for fuel. Lactate builds up and that familiar fatigue and pain ensue. The same thing happens is you train hard but eat poorly. Without sufficient nutrients, protein synthesis cannot happen, at least not appropriate to the demands. No one doubts this chemistry in sports, but in medicine, we seemed to have missed the parts about providing the muscles fuel and activating them to process that fuel. We look for all manner of mechanisms to explain muscle loss in patients, except the most obvious: the absence of fuel and/or activity.
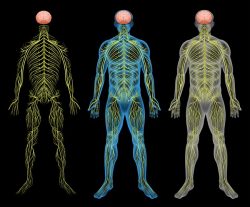
On the most basic level, it begs a question about what is required for protein synthesis in muscles. What are the core substrates, what is the fuel that powers this process? Well, firstly, it requires energy or ATP, perhaps consuming as much as 70% of the ATP produced. That means we need healthy mitochondria. Digging deeper, what do we need for healthy mitochondria: an abundant supply of macro- and micronutrients. In other words, we need to consume sufficient protein, fats and carbohydrates, along with sufficient vitamins and minerals to produce ATP, so that protein synthesis can occur at a rate greater than protein breakdown.
Can we learn some things about neuromuscular pain and injury from sports physiology that we cannot from medical research? I think we can.
Optimum Performance Versus Symptom Management
The research in sports physiology is useful for not only understanding athletic performance, but also, for understanding the limits of health at the molecular level. In many cases, the work in sports physiology is far more detailed and I would dare say, hopeful, than similar topics covered from the medical perspective. In sports research, the objective is to understand and maximize optimum performance. Even in the case of injury, the underlying goal is always to expedite recovery and how best to support the healing process. When athletes are injured or become ill, the question is not if they can train again, but when and how quickly they can return. The prevailing assumption is that they will heal.
In contrast, medical research involves understanding a disease process, and more often than not, any consideration of mitigating that disease process involves only the treatment of symptoms, which are surrogate markers of the illness at best. In medicine we get lost in in the weeds, endlessly searching for this or that aberrant mechanism to pin the ‘disease’ on. Rarely, does medicine ask why a particular mechanism might be aberrant and even more rarely is there any consideration of how to correct the presumed disease process or maximize the health of the affected tissues, organs, or even the human experiencing that disease. Some would argue that approach is emanates largely from of our predilection for pharmaceutical solutions and to some extent, I would agree. I think there is more to it, however.
In many ways, the medical model presupposes a certain futility. It is as if, the disease process, once initiated, can only be managed and never overcome. Health seems to have been written out of the equation entirely. Indeed, that health or illness evolves from a human organism and not just detached mechanisms seems absent as well, but that is a broader, more philosophical discussion for another day.
Returning to our comparison of approaches, as an athlete and a research scientist, I find the more hopeful perspective of sports research entirely more useful not only for athletics but for recovery in general.
Myopathy and Myalgia
What does any of this have to do with treating myopathy and myalgia?
On a daily basis, I interact with dozens of individuals who have been injured by the medical model and the ill-conceived notion that medications lead to health. Inevitably their illnesses involve some degree of mitochondrial dysfunction, and more often than not, core symptoms will include muscle pain and weakness, which in medical speak is myalgia and myopathy. And yet, despite years of failed treatments and endless pain and suffering, when I ask about diet and lifestyle, to say that I am met with chagrin is an understatement. “How could diet and exercise possibly be involved with the muscle wasting, with myalgia or myopathy? Those are legitimate illnesses,” I am sure they think to themselves. Well, let me repeat myself,
“The synthesis of muscle proteins must outpace the breakdown of muscle protein.”
This is something so simple and utterly obvious to any athlete, but completely foreign to most in the medical field. Consider any discussion on muscle wasting (cachexia or sarcopenia) or disorders involving muscle pain and weakness in the medical literature, rarely is there any consideration given to the nutritional demands that drive these molecular changes. Is the patient getting what he/she needs nutritionally to drive protein synthesis? Seems like an obvious first question, but it is not. A second, but equally obvious question would include activity level, and barring conditions that restrict mobility, activity should be a core component of treatment and rehabilitation. If either or both of these factors are ignored, no amount of medicine will promote recovery, and in that regard, the model of disease futility is accurate, albeit self-perpetuating.
I would argue that the muscle pain and wasting we see with many an illness often represents no more or no less than a skewed balance between the synthesis and breakdown of protein. Sure, there are likely some individual genetic components that contribute, but no matter the genetics, if the substrates derived from diet are absent or lacking, muscle pain and weakness will develop and when there is muscle pain and weakness, activity is limited. Similarly, if mobility or activity is constricted or absent, protein synthesis will slow down, even if dietary considerations are met. Muscle requires adequate dietary proteins and adequate movement to avoid myopathy, myalgia, sarcopenia, cachexia. If either, but especially when both of those variables are lacking, the downward spiral of decreased protein synthesis and increased protein breakdown in muscles begins.
I hear the series of ‘buts’ now.
“But Chandler, you don’t understand, I cannot [fill in the blank] because of [fill in the blank].
In fact, every time I comment online regarding the need for either more protein in the diet or the requirement for more (or any) movement to recover, I am lambasted. How dare I suggest diet and exercise are required to maintain health or recover from illness? Admittedly, this flies in the face of modern medical treatments, with too many physicians looking to diet and exercise only as a last resort, and generally, with the very heavily biased assumption that if diet and exercise are involved, then the conditions for which the patient is seeking treatment must not be real.
Of course this is asinine. These disease processes are real, but within the current medical model the realness of a disease is determined only by its connection to a pharmaceutical and the ability of the pharmaceutical to temper some surrogate marker of that disease process. When there are no pharmaceuticals that return the patient to health (because, given the chemistry, how could there be), it is an easy jump to assume the patient is feigning their symptoms. They are not feigning their symptoms. The chemistry involved in the muscle wasting is real, but so too is the solution. The body needs certain things to function, period. When it does not get those things, compensatory reactions ensue and disease processes begin.
Severe Muscle Wasting
Returning to muscle pain and weakness and the more severe process of muscle wasting, we see littered throughout the research, the ‘recipe’ for muscle health: protein and activity. For example, the research involving muscle wasting in critical care patients where immobility is common, do you know what prevents muscle wasting? Movement. That is, the simple act of passive resistance – e.g. someone moving or exercising the muscles for the patient, reduces muscle wasting. This is because a whole slew of mechanosensors in the musculature must be activated regularly so that the cycle of protein degradation and synthesis continues. Immobility, grinds this cycle to a halt. The muscles need to be activated to send the requisite signals that protein cycles should continue. Absent those signals, in other words, absent movement, atrophy and cachexia cycles begin, developing within only a few weeks of immobility.
Similarly, a review addressing various forms of muscle wasting from sarcopenia (muscle lose in the elderly) to cachexia (muscle loss in cancer), found that both providing additional protein in diet and enabling resistance training, in whatever form possible, even passive resistance, decreased muscle wasting and increased function and quality of life.
This tells us that the answers are right in front of us. Dietary protein and activity are requisite to avoid muscle wasting. Absent one or both of these and problems develop. Absent one or both for a sufficient period of time and muscle wasting, pain, and other processes begin. Oh, and the brain needs protein too.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
This article was published originally on July 2, 2018.