Iodine is an essential element required for the propagation of chemical reactions that are needed to create the thyroid hormones Thyroxine (T4) and Triiodothyronine (T3). This process can be termed “Organification” whereby an inorganic molecule (iodine) is implemented in organic molecules (thyroglobulin protein). The organification process results in the production of these extremely important hormones. Any reduction of thyroid hormones, commonly through reduced iodine intake, will result in the debilitating symptoms of hypothyroidism. Unfortunately, iodine deficiency or insufficiency disorders affect around two billion people worldwide. In fact, iodine deficiency is considered to be the single greatest cause of preventable brain damage and mental retardation in children. The latter, known as congenital hypothyroidism, occurs during early childhood and results in stunted mental and physical development due to low iodine intake.
Iodine deficiency, however, can affect processes outside of thyroid hormones when the extrathyroidal action of inorganic iodine is disrupted. Extrathyroidal refers to iodine-mediated processes outside of thyroid-mediated organification (T4/T3) and is currently being more appreciated in the scientific and medical communities. The focus on thyroid hormones, understandably, has overshadowed scientific investigations regarding iodine’s role in extrathyroidal processes. As we will explore below, it turns out that other very important non-thyroid cells express receptors to transport iodine into the cell. These receptors can be regulated by the body in a similar fashion to the thyroid glands. That is, the body can increase them or reduce them (i.e. on/off switches) depending on the need.  Some of the functions of extrathyroidal iodine have been effectively implemented clinically in cancer therapy.
Some of the functions of extrathyroidal iodine have been effectively implemented clinically in cancer therapy.
Technical Note on Inorganic Iodine: The term iodine refers to the molecular state of iodine (I2) where two iodine atoms are bound together. The term iodide refers to ionic iodine which, similar to salts (i.e. sodium chloride), it can be found ionically bound to sodium or potassium (i.e. potassium iodide, sodium iodide).
Organification of Iodine Atoms
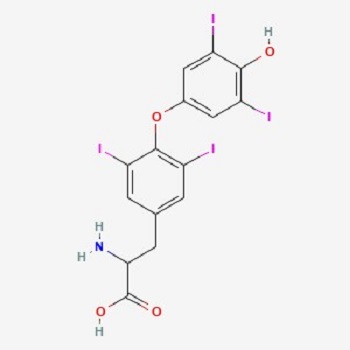
It is known that to make thyroid hormones (T4/T3) the body requires a sufficient supply of iodine. What is important to understand about this statement is that iodine is not just acting as an enzyme cofactor, but it is actually a part of the hormone. Thyroxine (T4) is 65% iodine by weight due to the relatively larger mass of the iodine atom (see PubChem image).
Briefly, the thyroid cells express a receptor called Sodium Iodide Symporter (NIS) which allows iodide to get into thyroid follicular cells from the plasma. The iodide molecule then moves into another compartment called thyroid colloid/lumen by another receptor named PENDRIN. From there it gets oxidized, from iodide to iodine, by thyroid peroxidase (TPO). The oxidized iodine finds a place in a protein named Thyroglobulin (TG) where all of the thyroid hormones are being built. There is a plethora of them on TG which include (T1, T2, T3, and T4). In this case, T4 refers to four iodine atoms present, while T3 refers to three iodine atoms.
Further reactions occur within TG allowing T4 and T3 to leave the thyroid. Here, 80% of the hormone mix is T4. Even though the thyroid glands produce mostly T4, T3 is the more active hormone and is produced from within other cells of the body such as the liver, kidneys, as well as immune cells. This is done by special enzymes called deiodinases that can convert thyroid hormones to multiple forms. In the end, T4 and T3 affect the metabolic processes of cells, which include thermogenesis, gluconeogenesis, glycogenolysis, and protein metabolism.
All of this comprises the hormone/organification process of iodine within the thyroid. Now let us look at the role of iodine in the rest of the body.
Iodine as an Antiseptic
Iodine is one of the best-known antiseptic agents with the least toxicity to human cells. When the term iodine is mentioned many, especially in the medical community, think of antiseptic or wound cleaning utility of iodine such as Povidone-Iodine. Iodine is used in such a manner because of its direct killing effects on bacteria. An example of this would be disinfecting a bucket of water or small wounds. The mechanisms of direct killing also happen within the body and include interference with the electron transport chain in bacteria, which human cells can better defend against.
Next, iodide can enter human cells by the specific transporters NIS and PENDRIN. In this case, the first direct mechanism occurs when the iodide form is converted into bactericidal molecular iodine through the actions of hydrogen peroxide with potential help of copper, as well as enzymes such as TPO and Myeloperoxidase. In this way, iodine is able to kill infections in localized areas (infection sites).
Iodine and Neutrophils
The second mechanism is semi-direct. Here, immune cells such as the neutrophils pull iodine into special cellular compartments called the phagosomes that are choke-full of hydrogen peroxide ready to convert iodide into iodine. This process is used by neutrophils to eventually make a bacterial-toxic compound called hypoiodite. Hypoiodite is even more bacterial toxic than hypochlorous Acid (active disinfectant component of bleach). Hypoiodite is used to “iodinate” bacterial cell walls. Interestingly, neutrophils also make a ton of hypochlorous acid naturally using chlorine atoms in a similar way to iodine. Therefore the neutrophils are given two halogen options (chloride and iodide) to kill microorganisms. Neutrophils will take either chlorine and make hypochlorite (bleach) or iodine and make an even more effective substance, hypoiodite. Chlorine is more abundant so cells typically “bleach” out bacteria or fungus.
Iodine to Treat Infection
Clinical Utility of Iodine in Treating Sinusitis: There have been recommendations by persons such as Dave Asprey (founder of BulletProof) for the use of iodine in treating acute or chronic sinus conditions. These recommendations make sense from what we have discussed above. However, more specifically, studies have shown the effective role of iodine in treating infected human sinus tissue. In this case, patients with chronic sinusitis were examined and were found to have a variety of microorganisms (Staphylococcus aureus and Pseudomonas bacteria & Yeast). Infected sites were extracted during surgery from the ethmoid region and then were exposed to potassium iodide, iodine tincture, or ethyl alcohol to control for the alcohol in the tincture. They used the Baclight assay which allows visualization of intact vs broken membranes of microorganisms via fluorescent microscopy. The findings were as follows:
- Iodine kills microbial pathogens even if they are within a biofilm.
- Treating for 10 minutes had similar effects as 30 minutes.
- Iodine tincture had slightly more destroying power than potassium iodide (SSKI).
The limitation here is that this study was done in vitro (in a laboratory setting), but nevertheless, it used human infected nasal tissue post-surgery. This, with the plethora of anecdotal stories from people who use iodine in this context, supports the importance of iodine in treating sinusitis.
Clinical Utility of Iodine in inactivating SARS CoV: Studies have shown that the direct effects of iodine apply to Coronaviruses. For example, gargling with povidone-iodine for only 15 seconds resulted in inactivating MERS-CoV and SARS-CoV. It is thought that the inactivation was due to inhibition of viral protein synthesis and alteration of the viral membrane. Because of this, it is almost certain that iodine would have a similar effect on the recent SARS-CoV2 virions. Some other researchers recommended the combination of Zinc, DMSO, and Iodide for the treatment of SARS-CoV2 infections and for boosting immune functions.
Iodine Promotes the Function of Human Immune Cells
There is yet a third iodine-mediated mechanism that the body uses to get rid of pathogens. That is, in addition to the direct mechanisms above, iodine can enter immune cells and activate gene transcription. Before addressing this aspect of iodine function, let us first briefly look at a study from the 1980s by Marani et al that alluded to the role of iodine and immune cells.
The study looked specifically at a group of Italian school-aged children in an area endemic of goiters. Out of 607 children, 48% had goiters despite many having normal thyroid values (TSH, fT3, fT4) with no apparent autoimmune reactions to thyroid peroxidase or thyroglobulin. The immune system of these children had deficient “delayed immune responses” as measured by skin testing – in essence, they assessed the adaptive immune response (T cells). It is important to note that some of the school children who were deficient in iodine also had reduced immune responses despite normal thyroid hormone levels. The latter statement is critical which demonstrates that just because your thyroid glands look normal on a blood test, does not equate to iodine sufficiency within the body. This is an important point since it is not common knowledge that inorganic iodine itself is important for cell function (outside of its role in thyroid hormones). For the treatment arm of the study, 215 children were given Lugol’s iodine (a mix of iodine and iodide) at a dose of 2 mg/week for eight months and were compared to controls not given iodine. After eight months, the children who received iodine had a marked restoration of immune responses with the same test compared to the kids who did not receive iodine.
The question stemming from this is how was iodine affecting immune cells? There were not too many studies that followed Marani et al and looked at specific mechanisms of inorganic iodine within immune cells, however, a recent study from our laboratory in 2017 showed some of what iodine is doing. In our study, immune cells were given iodine as sodium iodide or Lugol’s solution and then were assessed for activation at the protein and genetic level (ribonucleic acid [RNA] sequencing experiments). It was found that iodine “energizes” these cells by making them alter their genetic signature (RNA), which then promotes the release of proteins that are very important for immune function, termed cytokines. Within these cytokines, there is a group called chemokines. Chemokines allow immune cells to move better through the body, to kill tumor cells, and to fight infections. Overall, this has large implications for the cells interacting with iodine in the gut and other places in the body like in the blood, liver, thymus, and other cells. Importantly, no alteration of thyroid hormones were observed between iodine treated and non-treated immune cells. Therefore, these effects seen were directly caused by inorganic iodine and not by thyroid hormones.
Immune System Studies within Animals: Another recent study on dairy cows confirmed our laboratory’s results in human cells. The study demonstrated that when dairy cows were given iodine, significant changes were detected in their genomic transcriptional activity (RNA). The authors show that up to 525 genes were altered when cows were given iodine! Some of the significant gene changes were Fc Receptors – these receptors are located in phagocytic immune cells that can “eat up” bacteria. Iodine also caused an increase in genes that activate immune B cells – these are the cells that produce antibodies and protect against a variety of infections such as SARS-CoV2. Antibodies mark cells and foreign invaders for attack and destruction. Again, the increase in immunity was not due to enhanced thyroid hormone synthesis. Therefore, iodine can control specific gene expression in these dairy cows.
For a more in-depth discussion of iodine and different types of immune cells, the reader is referred to this manuscript.
Utility of Iodine in Cancer Treatment
There is no doubt that without an effective immune response, one would be susceptible to a variety of cancers. We’ve already seen how iodine can improve the immune response towards more activity, trafficking, and killing mechanisms. These mechanisms apply to both pathogens and cancer cells that can be located by specialized immune cells. We can then hypothesize that a deficiency of iodine will reduce the immune response (as observed in the Italian children’s study), and thence substantially increase the chances of cancer development and/or progression.
Clinical Utility of Iodine in Breast Cancer Treatment, Study 1: Moreno-Vega et al showed in 2019 that iodine can be very effective in treating breast cancer. They used 60 women who were in early (stage II) and advanced (stage III) stages of breast cancer and then gave them 5 mg/day of iodine along with placebo controls. They relate in their conclusion:
I2-treated tumors exhibit less invasive potential, and significant increases in apoptosis, estrogen receptor expression, and immune cell infiltration. Transcriptomic analysis indicated activation of the antitumoral immune response.
They also found that the five-year disease-free survival rate was a lot higher in patients receiving the iodine. Here we see that the mechanisms discussed above are at play in real patients as follows:
- The immune cells were activated and were able to traffic better to tumor tissue!
- Changes within the tumor cells were seen indicating that inorganic iodine directly affected the cancer cells.
Clinical Utility of Iodine in Breast Cancer Treatment, Study 2: Mendieta et al showed in 2019 that “I2 decreases the invasive potential of a triple-negative basal cancer cell line, and under in vivo conditions the oral supplement of this halogen activates the antitumor immune response”. In other words, iodine inhibited breast cancer metastasis.
Clinical Utility of Iodine in Breast Cancer Treatment Study 3: Another study coinciding with the writing of this discussion (September 2021) showed that I2 induced the immune response by affecting the methylation status in specific sites of the genome [more information on methylation on this blog post]. Some of these genes are cytokine genes such as Interferon Gamma which acts in the anti-tumor immune response. In essence, Interferon Gamma gene regions become “de-methylated” which makes the gene more active in the cell. They also showed increased infiltration (increase) of immune cells named macrophages. These cells are important because they collect information from tumor and infection sites and then relay them to the killer immune cells (T cells).
Other studies have shown similar results using shock wave therapy with iodine. Additionally, there are now clinical trials to further look at these great direct and indirect anti-tumor effects of iodine. There is no doubt from these studies that iodine carries strong anti-tumor properties.
Role of Inorganic Iodine with Regards to Fertility
Analysis of the US population by the National Health and Nutrition Examination Survey (NHANES) has shown that about 35% and 38% of women of childbearing age and pregnant women, respectively, had less than 100 µg/L of urinary iodine levels. This is below the current recommended reference range and demonstrates iodine deficiency. Importantly, approximately 58% of women of the childbearing age had less than 150 µg/L of urinary iodine. The latter number is below RDA for pregnant or lactating women. This should be of major concern for public health given the effects of an iodine deficiency on human health such as mental retardation, infertility, and reproductive failures. This is in part due to lowered metabolic rates from the low production of critical thyroid hormones.
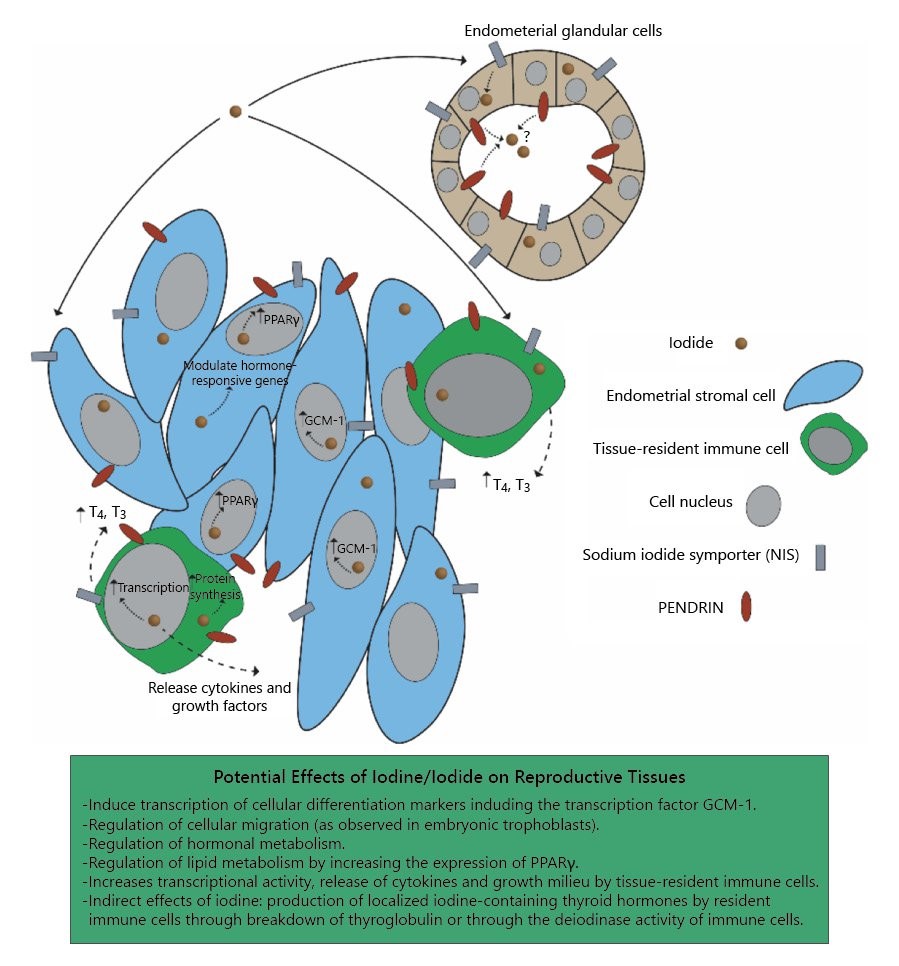
What about extrathyroidal iodine? Similar to immune cells, recent studies from our laboratory (2020) have also shown that the human endometrium can express iodine receptors. This study was performed with the assistance of Dr. David Brownstein who is an iodine expert. Briefly, the study shows gene analysis data (RNA Sequencing) that demonstrate the possibility of localized iodine deficiency in women with reproductive pregnancy loss or implantation failures compared to controls. We hypothesized from these findings that inorganic iodine (i.e. sodium iodide, potassium iodide, molecular iodine obtained from food) is needed for proper cellular function in reproductive tissues, and that iodide transporters [receptors] may potentially be used as a marker for infertility or for probing potential localized iodine deficiency that may not present in a typical thyroid panel analysis.
Can Non-thyroid Human Cells Produce Thyroid Hormones by using Iodine?
One of the questions inquired by the 2017 immune cell study above was if any other human organ or cells can produce thyroid hormones. The classical view is that only the thyroid can do this, and indeed the thyroid bears the weight of making these hormones. However, it turns out that immune cells can perform very similar functions to the thyroid. The same 2017 study showed that human immune cells could uptake the Thyroglobulin protein and then produce from it thyroxine (T4) and triiodothyronine (T3). These cells can also potentially make thyroglobulin and iodinate it using inorganic iodine – although organification of thyroglobulin by iodine has not yet been clearly shown experimentally outside of the thyroid. Nevertheless, the study shows that your thyroid is not the only place where thyroid hormones can be made! In addition, the immune cells seem to be very good at converting T4 to T3 and therefore can help in making you feel more energized.
Recommended Dose of Iodine
The subject of daily recommended iodine intake is extremely controversial even within functional medicine groups. Part of this controversy is due to the fact that a small population can respond negatively to high-dose (> 12-100 mg) iodine supplementation by amplifying autoimmune thyroiditis (increased thyroid antibodies). While this is true in some cases, it is not common and the missing link for that group is probably, in part, deficient antioxidant defenses. This includes reduced levels of selenium, glutathione, and copper. Anytime iodine is ingested, the thyroid ramps up hydrogen peroxide production and reactive oxygen species. If there are no antioxidant defenses, well then the person is left defenseless against thyroid injury and autoimmune antibody production.
One faction of the debate that is not as controversial with a better consensus, is that we certainly need to increase the minimum iodine RDA from 150 µg to around 0.5-3 mg (500-3000 µg). This is because we are understanding more that other body tissues need to utilize iodine as discussed above and that other non-thyroid tissues store iodine. Additionally, therapeutic studies discussed above-used doses in this range and up to 5000 µg. Some others take the middle road and recommend at least 1000 µg. Other very well-regarded physicians who are experts in treating patients with iodine go as high as 50-100 mg per day (50000-100000 µg). Regardless, with any supplementation, one must consider advice from qualified medical practitioners to avoid negative unnecessary side effects.
Conclusion and Future Developments
We can appreciate from recent studies that the human genome is set to respond to iodine and at the same time utilize it for fighting infections. When one is sufficiently replete with iodine, they are able to destroy microorganisms directly but also ramp up multiple indirect and direct mechanisms by the intricate network of the human immune system. Overall, from the above discussion we can conclude the following:
- Iodine can directly kill microorganisms such as bacteria, viruses, and yeast by interfering with their electron transport chain, protein synthesis, or cell membrane.
- The immune system can utilize iodine in powerful compounds such as hypoiodite to kill microorganisms.
- Iodine and iodide can enter immune cells and affect gene transcription and the function of immune cells. These effects have been shown to enhance the immune system in human cells as well as within large animals.
- Iodine has been used successfully to treat cancers. Part of its anti-tumor effects are both direct (on tumor cells) but by also activating the immune system.
- Some women with infertility or recurrent pregnancy loss seem to have low iodine levels in their reproductive tissue.
- Immune cells are able to produce thyroid hormones given the proper environment.
- “Normal” thyroid blood tests do not necessarily correlate with complete iodine body sufficiency.
Certainly more studies are underway to define the role of extrathyroidal iodine in all body compartments. For example, the author speculates that iodine is important for liver detoxification. This is because cell culture studies showed that iodine can increase levels of Cytochrome P450 enzymes which is likely to also occur in the liver in response to iodine replenishment. While it would be difficult to attain a complete review and consensus regarding the recommended daily doses of iodine, the research presented above suggests that we certainly need more than what is currently recommended.
Further Recommended Reading
Bilal MY, Dambaeva S, Kwak-Kim J, Gilman-Sachs A, Beaman KD. A Role for Iodide and Thyroglobulin in Modulating the Function of Human Immune Cells. Front Immunol. 2017 Nov 15;8:1573.
Bilal MY, Dambaeva S, Brownstein D, Kwak-Kim J, Gilman-Sachs A, Beaman KD. Iodide Transporters in the Endometrium: A Potential Diagnostic Marker for Women with Recurrent Pregnancy Failures. Med Princ Pract. 2020;29(5):412-421.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, and like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Feature image created using Canva AI.
This article was published originally on September 20, 2021.















Hi,
Thanks for your article.
i have been thinking about using SSKI to treat periodontal disease.
Long story short, I have had very High TPO ab for years (first tme I had those tested 4 years ago they were about 3.600 and the last time about 2.000).
TSH went from suppressed to 1 in 3 years over the same period.
Thyroid hormones are in range.
i am a 46 year old male, very prone to stress.
My 2 cents is that all stems from a severe gut disbiosys and this Is why I’d like to give SSKI a try but I am wary of a potential increase in ab.
Thanks in advance,
Roberto
Hi Roberto,
Thank you for your comment. My general opinion on this is that I would not go into SSKI or other forms of high dose iodine with your current condition before addressing other factors. I would recommend the person to first utilize co factors (selenium, copper, magnesium, vitamin C, and B vitamins, zinc). This doesn’t mean a long wait, but more of a month or two of replenishment. As you probably know these assist your antioxidant system when reactive oxygen species are created during thyroid hormone synthesis (including hydrogen peroxide and superoxide in the thyroid).
You mention that your thyroid hormones are normal, how normal are they and what fraction of the hormone was measured (free T3/T4 vs Total T3/T4)? Your TSH may have been suppressed due to thyroid injury releasing stored hormones. Therefore you may have vacillated on the border of hyper/hypo at some point.
I agree with you on the gut inflammation/infection being related to your thyroid disease. If someone has been diagnosed with SIBO, or other related gastrointestinal infection then I would guide them to contemplate on the immediate use of Oreganol P73 (super strength) and Oregamax. Later on, Iodine can also be included in therapeutic forms. That type of oregano (which is the only type I recommend for internal use) can also be used for other types of infections… However it sounds with all these issues (stress, infections in gut and other locations, thyroid) that you may need to tackle this problem from different angles in addition to therapeutic nutrients. That person may also want to consider altering their diet, at least temporarily (grain free and/or dairy free) in case this problem caused malabsorption of nutrients required for a healthy thyroid.
Many thanks for taking the time to answer so quickly and in detail.
When saying in range, I mean to refer to FT4 (1.16) and FT3 (3.34). Total T4 and T3 have not been measured.
The only injury that I can think of is the potential harm from trying nascent iodine a few years ago or maybe the EBV infection (not sure when it occurred but ab were positive the only time that I had those ab checked).
As regards stress, you are spot on. I am a perfectionist and an overthinker to say the least and maybe the combination of stress, EBV and gut issues could provide an explanation.
Thanks to Dr Lonsdale and the beatiful Dr Chandler Marrs, I have been using TTFD and B complex, although not regularly and I’ll definitely try to follow your suggestions re co-factors.
As for the oregano, those supplements are very difficult to find in Europe but let’s see. Maybe they will help tackle the persistently elevated neutrophils (80%).
Finally, abstainig from grains for an Italian guy iid the most difficult one but maybe it would be worth to try.
Thanks and regards,
Roberto
Hello! I am having trouble re-acclimating to my Armour Thyroid. I was one it, and Endo put me on T4 only, due to heart palps, and long story there after (went hyper with severe horrific reactions and much damage to my body now), but back on my Armour. Still having massive nerve issues and heart palps. I believe all underlying due to B1 deficiency. I want to start using B1, while waiting on my SpectraCell results due back in 2 weeks. My question is, have you found anyone has had to lower their thyroid med while starting on B1 therapy? I do have an underlying heart condition, Cardiomyopathy and LBBB. Figured to be caused by prior viral damage. If I take even a quarter of a 150 Bentfomine capsule I can feel it make my heart beat stronger within 15 minutes. So I don’t want to whammy my heart too much. Thank you,
Hi Penny,
My apologies for the delayed response. I am not aware of studies or anecdotal evidence showing B1 to increase thyroid production in the immediate sense. Perhaps discuss with your doctor lower doses of B1 (Thiamine HCL instead of benfotiamine) as a starting point. What did your spectracell results indicate? As you may know B1 requires other cofactors as well (magnesium, riboflavin) that you may want to consider.
Many thanks for taking the time to answer so quickly and in detail.
When saying in range, I mean to refer to FT4 (1.16) and FT3 (3.34). Total T4 and T3 have not been measured.
The only injury that I can think of is the potential harm from trying nascent iodine a few years ago or maybe the EBV infection (not sure when it occurred but ab were positive the only time that I had those ab checked).
As regards stress, you are spot on. I am a perfectionist and an overthinker to say the least and maybe the combination of stress, EBV and gut issues could provide an explanation.
Thanks to Dr Lonsdale and the beatiful Dr Chandler Marrs, I have been using TTFD and B complex, although not regularly and I’ll definitely try to follow your suggestions re co-factors.
As for the oregano, those supplements are very difficult to find in Europe but let’s see. Maybe they will help tackle the persistently elevated neutrophils (80%).
Finally, abstainig from grains for an Italian guy iid the most difficult one but maybe it would be worth to try.
Thanks and regards,
Roberto
Hi
I am sceptical to the claims of the Marani 1985 study. I cannot assess it anywhere. I want to see the children’s thyroid levels myself. So many scientists don’t know what are normal, healthy thyroid levels. They mistakenly believe, it’s within TSH reference range. As do many doctors. This is a big flaw in so many studies on the thyroid. Children have higher levels than grown ups, their FT3 should be quite high in range. I don’t think they even tested these children’s FT3. Have you read the whole study yourself? Have you seen the thyroid results? I find it very unlikely that that many should have goiters without thyroid issues. I am well aware, that one can have a goiter without thyroid issues. But I would want to see it with my own eyes. If you have only read the abstract, don’t take the author’s conclusions at face value. If you have the study, please post the thyroid results.
Hello Liv Stang-Lund,
Thank you for your questions, these are great points.
First, I completely agree that many scientists (physicians included) are not aware of the dynamics, continually in flux, thyroid/TSH/T4/T3 loop. It is treated as an algorithm but its rather dynamic and sometimes hard to poinpoint because what the “normal” blood shows is different from symptoms (including goiters – see below). As you can see, in my conclusion above I listed [“normal”] to indicate ambiguity of these ranges. Specifically, I’ve questioned optimal ranges and whether these numbers confirm/exclude iodine deficiency and tissue level hypothyroidism. Here, when I state “normal range” I refer to the ranges used by conventional medicine to diagnose hypothyroidism or an iodine deficiency – on which I am not particularly in full agreement with. So I think we may be in agreement that these ranges are not optimal nor sensitive to hypothyroid status or an iodine deficiency.
Second, my analysis was not based solely on Marani. I linked them here as they were one of the first to observe this discrepancy between goiter formation and thyroid biochemical status (T3/T4). In addition, they have concomitantly measured the immune response in relation to iodine. Their in-vivo studies matched my own in-vitro experiments with iodide-induced immune responses. Nevertheless, you are correct, I’ve also had trouble getting their actual data but I did manage (in 2017) to get their letter-to-the editor. Let me know if you want this document and I can send to you.
After assessing Marani’s claims, I found other studies showing actual data with a similar pattern to Marani’s 1985 statements, including:
1. In 1975 Chopra et al demonstrated that serum T3 and TSH were no different in subjects with or without goiters – including adults. In other words, having normal TSH or T3 does not always imply normal thyroid states as seen by goiter presence (in my opinion, it is indicative of iodine deficiency) https://pubmed.ncbi.nlm.nih.gov/1117981/
2. Bhattacharjee et al, in 2013, found that serum TSH was found in “normal” range in 90% of goitrous children (total 140 subjects). Additionally T4 and T3 were in the normal range for most of the children (albeit with different stages of goiters). Here the authors claim that the studied-region was known to have a moderate iodine deficiency within the population. This author links to other studies showing similar observations. An example quote “The serum levels of T4, T3 and TSH are in the normal range in most of the children with different grades of goiter suggests that these are relatively less sensitive marker for iodine deficiency”
[Serum thyroid hormone and thyrotropin levels in school children from goiter endemic sub-Himalayan tarai region of Eastern Uttar Pradesh,India.]
3. Krzyczkowska showed that even though pregnant women studied had normal TSH and total T4, they still had low urinary iodine levels. https://pubmed.ncbi.nlm.nih.gov/8055806/
Can the standard thyroid ranges affect part of their conclusions? Perhaps maybe in some studies, but again, part of my point is that these ranges should not be used to fully conclude normal thyroid state or extrathyroidal tissue-level iodine sufficiency – because clinical symptoms don’t match. Part of the reason, intuitively, is that an iodine deficiency will precede hormone disturbances due to thyroid stores and so the thyroid may enlarge prior to apparent “plasma hypothyroidism”. The thyroid then with highly specialized iodide metabolism will tend to get the bulk of already low dietary iodide from plasma, leaving disturbed non-thyroid functions, including immunity.
Hi
Thank you for your reply, and your comment on my blog. Which I will reply to in a few days.
I had not seen your reply. I don’t know why not, as I went back a few days after leaving my comment. You might want to consider activating the “sign up for future comments” function.
I am so glad, that you are aware of the fact that thyroid levels within range does not mean, one is not hypothyroid on tissue level. I have several studies on what are normal levels here https://thyroidblog.com/en/optimal-thyroid-levels/
Thyroid healthy people don’t vary that much on their levels, and a normal TSH is 1.5 to 1.8 for white people. Black people have a lower TSH. It’s very simple to assess eutyroidism on tissue level by temperature, pulse and blood pressure. If all doctors did this, we would not have millions of hypothyroid thyroid patients. Which we do have.
Of course, it makes sense that many children with goiter have normal thyroid levels. They haven’t had a goiter for long. I totally agree with your description of the progression when one is iodine deficient. The body also manages to keep the Ft3 level up for a while, despite low Ft4 levels due to the deficiency. But when the goiter is caused by iodine deficiency, one will always become hypothyroid in time. I just am always sceptical when I can’t see the labs with my own blue, as it’s more the norm than the exception, that the subjects are too low. I am working on a post on symptom load and antibody levels at the moment. In almost all studies on the subject, the subjects are hypothyroid. In one, some are hypo and some are hyper, with a ft3 ranging from 3,1 to 7,5 pmol/L. Of course, one can draw no conclusions from such a study.
I have read their letter to the editor. It does not include any thyroid results. Personally I would not include a study I haven’t read, or I would at the very least, inform the reader of the fact. I do that sometimes, if it is a very well known and important study. But one I cannot get into.
Thanks again for your reply, and I apologize for not having seen it. It’s great with scientists who take the time to interact with their readers. As I wrote, I will reply to your comment on my blog later. In the beginning of the week probably.
Reg. LIV
You are welcome. Your analyses of the literature and your blog posts are much appreciated! Thank you for your work.
I was diagnosed with thyroid issues and was given Armour thyroid about 10 years ago. It seemed difficult to regulate as many doctors altered the dose based on blood tests however I never felt well. At the start of the pandemic I was unable to obtain my medication due to a number of reasons and discontinued its use. Within one week I noticed many positive changes such as reduced racing of my heart, puffiness, less bloating and other issues I was experiencing. Concerned about my thyroid health I opted for iodized salt and started a thyroid supplement containing 100 mcg of Iodine. ( Gaia). I feel much better overall with occasional tired days. I still do quite a bit and am in my early 60’s. It makes sense to me my thyroid as a 60 year old would function slower than that of someone half my age and that this would be normal. I have been off Armour for over a year and think it was not as helpful as touted. Mostly due to a racing heart. This article is very technical for a lay person but made me wonder if the 100 mcg is enough or if I need more iodine? Any feedback would be very much appreciated.
Marjorie,
Thank you for sharing your story which will resonate with so many reading this. 100 mcg (ug) of iodine is not enough, even with currently established guidelines (150 mcg, and ~300 mcg for pregnant or lactating women). These guidelines need substantial review and amendments in-part due to reasons mentioned above. Therefore, at the moment, It would not be a problem raising your iodine intake to 300 mcg. In my opinion you need a lot more, but I would encourage you to discuss this with your informed medical doctor along with the following (if you haven’t done so already)
1. Discussion on your current general thyroid health (hashimoto’s?)
2. Discussion on the basic deficiencies which, in-part, can be inferred from routine blood work (CMP, CBC, etc…). This is because the thyroid, though requires iodine, will not be optimal is you are low in other factors (B vitamins, copper, zinc, selenium). You want to optimize these first.
3. Most importantly to attain more information I recommend reading the following books:
-Iodine : Why You Need It, Why You Can’t Live Without It (By Dr. David Brownstein)
-The Iodine Crisis: What You Don’t Know About Iodine Can Wreck Your Life (By Lynn Farrow)
Thank you! I recalculated my iodine intake as I neglected to include iodine in my multiple vitamin. It is 150 mcg so combined with that of my thyroid support of 100 mcg, I’m getting 250 mcg. Brings me closer to the 300mcg goal. Taking one additional multiple (Shaklee) in the afternoon is something I’m going to add. Not just for iodine but for energy. My thyroid diagnosis was Hashimoto’s. It evolved after UFE intervention for a very problematic fibroid. Tumor has shrank by over 90% since. I am sort of working with my doctor who has suggested labs. I will follow up but am very hesitant to start thyroid meds again. I felt horrible on them. Focusing on food sources too. Thank you so much for your response, so greatly appreciated!
Thank you. When you mention skin testing for immune response, do you mean IgE , like at the allergist?
Wonder if a lab for T cell response we can ck on. or the T1,T2… or if matters.
Might your article be related to those who have genetic snp for reduced T4 to T3 conversion.
It sounds like adding more mineral foods (selenium, copper, iodine…) might help ones health.
Have been using lots of iodine tincture topically on recent bug bites and wondered
how else to use tincture of iodine.
Hi Lynn, Thank you for reading and for your comment.
The skin testing that they have done was not the IgE (Type I hypersensitivity), but rather delayed immune responses (Type IV T cell and cytokine mediated). This is similar to the TB skin testing, except what they did was tetanus toxoid skin testing.
That is an interesting point regarding T1 and T2. But I think more research is needed to be done on these pre-thyroxine compounds to see if they correlate with iodine deficiency, for example. At the moment there may not be a major role for them other than act as a precursor to thyroxine or T3. They may also act as iodine “storage” around the tissues.
With regards to the other minerals (selenium and copper), I would first test before supplementing. Here is another blog-post on copper and thyroid (https://www.hormonesmatter.com/copper-for-mitochondrial-immune-and-thyroid-health/).
As an admin of an iodine community on FB consisting of 25K members I really appreciate this article and am very thankful for addressing this controversial topic. There are a lot of misconceptions concerning iodine and its optimal intake out there. We need more similar articles / posts / podcasts in order to clarify this topic, refute the misbeliefs step by step and eventually make people’s lifes better by ensuring their iodine sufficiency. Thank you very much once again, wish you good health!
Dear Balint,
Thanks a lot for what you do and for helping untangle the knots of misconception through your group and by spreading factual information. The good news is that I have been noticing a new wave, in the past 7 years, with iodine research including basic sciences and clinical. The cancer studies mentioned here are part of this research and are very promising.
Wishing you the best health!
Very nice explanation of whole body iodine. And am glad to see you included a resonable dosing amount up to 5 mgs. It’s unlikely a standard diet supplies anywhere close to that. Thank you for taking the time to pull all this together.
Thank you Lynn! I completely agree, we certainly need a lot more than currently recommended. In fact, in this manuscript we (including Dr. Brownstein) relate body iodine stores and that the current RDA range was not based on total body needs such as immune cells, ovaries, endometrium, etc… (https://www.karger.com/Article/FullText/508309).
Nice that you were able publish it open access! Looking forward to reading more of your work…..it’s needed. Thanks again.
Really well-written article. Thank you!
D. Gregory Olson, MD, PhD, APH
The Nevada Clinic
Thank you so much Dr. Olson.