Migraine is assumed to be a disabling neurovascular disease with various manifestations that affect the vasculature as well as the physiology of the brain. Migraine is categorized either as episodic headache (<15 pain days a month) or chronic (>15 pain days a month). It is also understood that migraine is associated with hyper sensory sensitivities and that about 15% of migraineurs suffer aura migraines. Migraine is strongly associated with metabolic disease1-9. Based on many studies, migraine leads to metabolic disease—either because of migraine prevention medicines or because of dietary lifestyle. Genetic factors also strongly underlie why migraineurs end up with metabolic syndrome. Before we investigate what these genetic factors are and how a migraine sufferer can avoid metabolic syndrome, we first need to understand what migraine is.
So, What is Migraine?
The current scientific understanding of migraine ignores many key factors because most doctors only see migraineurs when they are in pain or have aura, and most research is, therefore, only focused on pain or aura. However, every single migraineur experiences migraines without pain—silent migraines. Silent migraines are usually associated with aura migraines but cyclic vomiting syndrome, irritable bowel syndrome (IBS), and restless legs syndrome (RLS) can also be present. These other syndromes are often precursors of the migraine-brain development (particularly in children) and they come without migraine-pain. If one can have pain-free migraines, it means the pain in migraines is only a symptom. A symptom of an underlying condition that my research and publications have been identifying and describing.
I have written many blogs about migraine and its genetic connections, see here and here and have published a book that details all genetic, neurovascular, and metabolic connections to migraine, which you can find here. In these publications, I discuss how even 2-year-olds can have migraines, how cyclical vomiting, IBS, RLS, and anxiety often precede the presentation of migraine pains by years. Because of this, migraine can appear as “not migraine” for many years and these seemingly independent symptoms may end up being treated separately. In my research, working with thousands of migraineurs over the years in my FB migraine group, I have found that nearly all of them have some form of insulin resistance (IR), which may be exhibited by hyperglycemia (HG) or reactive hypoglycemia (RH), all of which nearly always remain undiagnosed for a very long time. This is particularly important, since contrary to non-migraineurs with metabolic syndrome, migraineurs sport low blood pressure and are often very thin—meaning several commonly used key factors for the classification of metabolic syndrome are not present, based on which medical professionals would even consider testing for metabolic syndrome.
What is Metabolic Syndrome?
If three of the following five categories are met (based on the new revision of the ranges; see original article here), the person is said to have metabolic syndrome.
- Waist circumference > 40 in (males) or >35 in (females)
- Fasting glucose ≥ 100 mg/dl
- Triglycerides ≥ 150 mg/dl
- HDL cholesterol < 40 mg/dl (males) or <50 mg/dl (females)
- Systolic blood pressure >130 mmHg or diastolic blood pressure > 85 mmHg
I repeat here the same in bold striked out the ones that migraineurs don’t typically have:
- Waist circumference > 40 in (males) or >35 in (females)
- Fasting glucose ≥ 100 mg/dl (true for a few)
- Triglycerides ≥ 150 mg/dl (true for a very few)
- HDL cholesterol < 40 mg/dl (males) or <50 mg/dl (females)
- Systolic blood pressure >130 mmHg or diastolic blood pressure > 85 mmHg<.strike>
As you see, migraineurs don’t meet three (and often none) of the above to qualify for a metabolic syndrome examination. Yet, when I ask for an at-home 5-hour fasting blood glucose test, checking for blood sugar fasted, pre-breakfast, 30 minutes after breakfast, and then every 30 minutes after that for 5 hours, I find some very complex IR and RH cases. Below find two common examples:
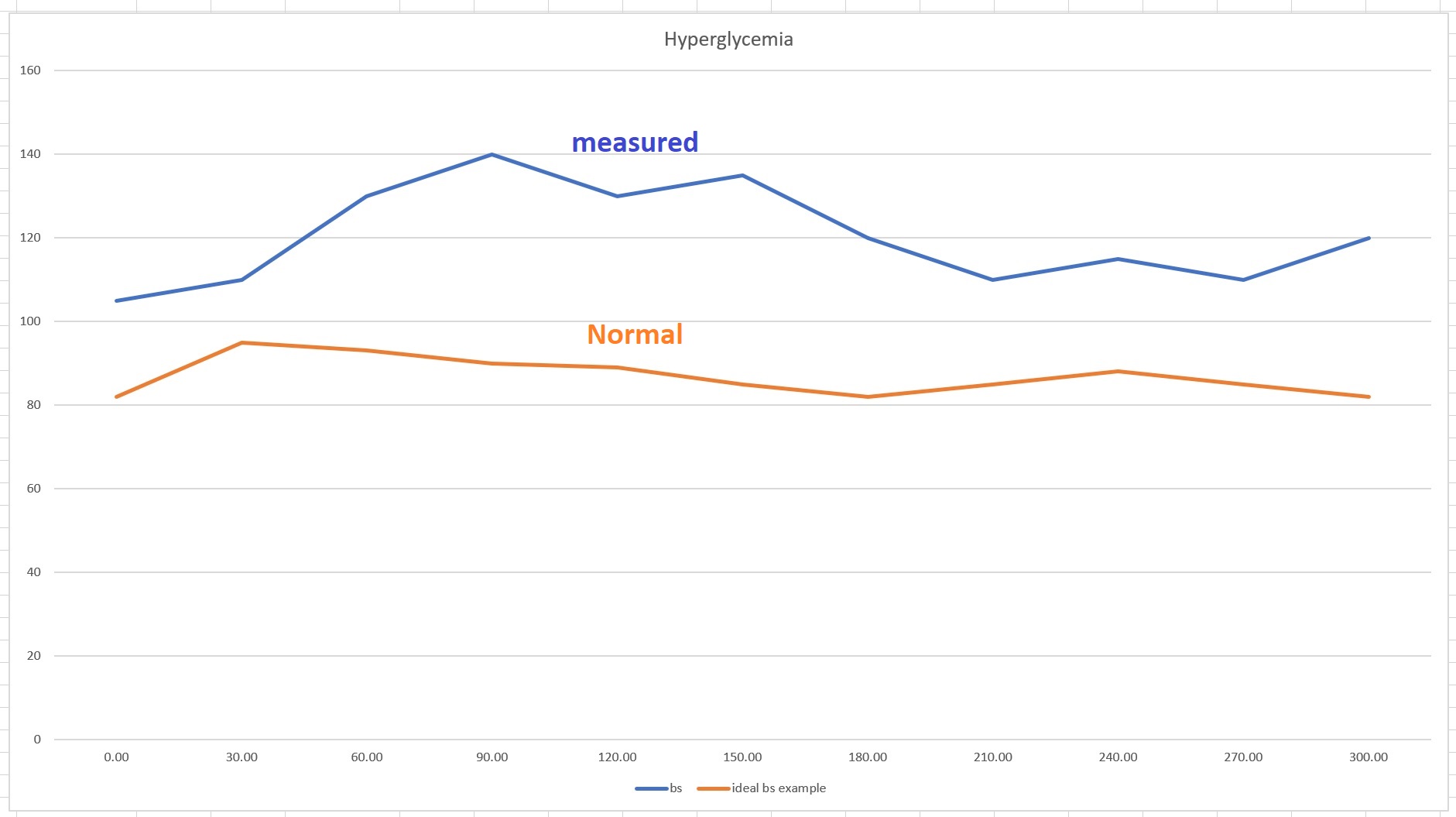
Hyperglycemia (high glucose)—note that the “normal” may appear low to you but my migraineurs are on a low carbohydrate diet where the maximum blood sugar spike should not exceed 20 points. The above hyperglycemia graph shows both an overly large blood glucose spike and a significant delay in the spike, suggesting serious insulin resistance.
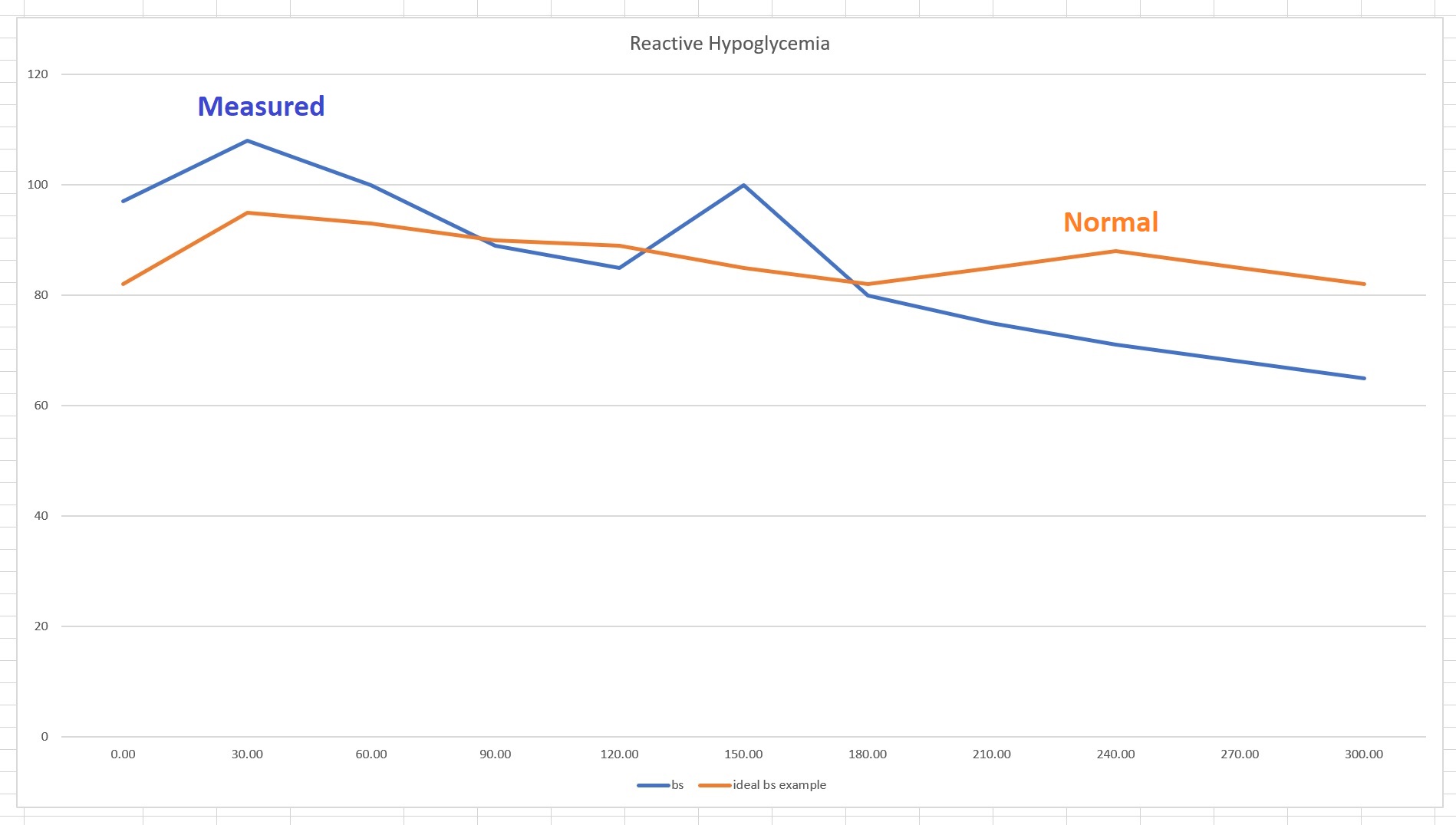
Reactive hypoglycemia is represented by blood glucose level that drops significantly after a meal.
Note that both of the above graphs come from people on a low carbohydrate diets, where breakfast is usually eggs with bacon with perhaps some raspberries with yogurt or a mix of nuts with cottage cheese. So the spike at the 2-hour mark usually represents the conversion of egg whites’ protein to glucose—hence, the spike at 120.00 minutes for the RH and a delayed spike for the HG. Some of the RH migraineurs ended up with such low blood glucose that they were close to fainting (two of them so far reached low 50s). Yet, because they don’t meet the “minimum three” criteria from the five listed above, many doctors flatly refuse to test them for metabolic syndrome. Some even disregard the at-home 5-hour blood glucose test as silly—not sure why, after all, there is no better method currently available. This just shows why migraineurs are never considered as having metabolic disease until it is late in the game, even though there are hundreds of academic articles showing the connection.
Given that migraineurs end up with metabolic syndrome (with most of the five points eventually) later in their lifetime, and since they are undiagnosed prediabetics for a very long time, could it be that migraine is actually a metabolic disease? Since IR, HG, and RH are part of metabolic syndrome and nearly all migraineurs have them from a young age, shouldn’t we investigate what the connection may be?
Observing that migraineurs end up with metabolic syndrome is one thing; finding if migraineurs have predisposition to metabolic diseases as a result of their genetics that includes metabolic gene variants within their migraine gene variants, would be an entirely different thing. Shall we go and find these genes?
The Genetics of Migraines
As a migraineur who is also a scientist, finding out as much as possible about migraines was easier for me than for those researchers who never had migraines. I knew what to ask and what to look for and could also tell what made sense and what didn’t. While most everyone’s first instinct is to say, “what works for one person may not work for another,” hold that thought! In the case of migraineurs this isn’t true. Over the many years of research, I found that migraineurs are like siblings. Nearly all of their symptoms and reactions to treatments are identical. If you want to fully understand why, you need to look at the genetic variances of migraineurs—all of these variances are identical or at least very similar to each other among migraineurs. How do I know this? Many migraineurs had genetic testing and shared their genetic data with me so I could compare their genetic variances with those “average” variances listed for migraine-genes.
True migraines start with a hormonal disruption as a result of overstimulation of the sensory neurons and end in electrolyte dysfunction that prevents action potential in some part(s) of the brain, which results in what is referred to as cortical spreading depression. This is well understood by studying the genetic template of migraine, where the first 30 or so genetic variances are all associated with ionic channels operating electrolyte management and maintenance. Other key genetic variants of importance among migraine genes are glucose transport, renin-angiotensin-aldosterone system (RAAS)10; see variants associated with RAAS as AGT, AGTR1, AGTR2 and BDKRB2 in the migraine genes and here the same associated with type 2 diabetes and here with hypertension, ATP binding, glucagon receptor, and several mitochondrial variants all with very high score in migraine genetic variances. These variants collectively lead to one key problem all migraineurs eventually face: metabolic syndrome5,11. Is it possible then that migraine, while it is clearly genetic, with its metabolism and energy associated variances, is actually a sign (symptom) of metabolic syndrome? In other words, does the genetic makeup of migraineurs lead directly to metabolic syndrome? The answer to this is likely yes. The reason? When migraineurs change their nutritional regime by excluding or greatly reducing all carbohydrates, they reverse their metabolic health condition, achieve full remission, and with that their migraines also disappear.
Clearly, migraineurs’ genetic makeup is such that factors responsible for type 2 diabetes are major components of their migraines. What are those factors? Metabolic syndrome in migraine is not diagnosed until the migraineur had the disease for many years because as we described, migraineurs don’t carry three out of five typical metabolic syndrome traits. The one common variable is chronic insulin resistance (CIR). While academic literature is quite a war zone when it comes to the causes of CIR, in migraineurs the cause is very simple to determine and the condition is easy to reverse.
Reversing Chronic Insulin Resistance in Migraineurs
All people with chronic insulin resistance have common symptoms when they are late with a meal or skip a meal: feeling grumpy, nervous, ravenous, sometimes shaky, sweaty while cold, anxious, and may even faint. Feeling hungry when blood glucose levels are above the body’s preferred 99 mg/dl (about 1 teaspoon of glucose in the entire body) is not normal but those with hyperglycemia feel hungry even when their blood glucose levels are way over 100. To understand the importance of this, we should understand what hunger actually is. I am not covering the biochemical and hormonal elements of hunger. Hunger is a state in which the body is running short of glucose for whatever reason. If the blood glucose level is way above normal, feeling hunger is not warranted. This sort of hunger actually signals insulin resistance because while the blood has plenty of glucose to feed the organs that need glucose, glucose doesn’t get there. It cannot get there because insulin is resistant—meaning it is not sensitive enough to pick glucose up to carry it to the cells. Therefore, eating when hungry while the level of blood glucose is still high, causes more trouble and the hunger will not be sated.
Reversing this type of insulin resistance (hyperglycemia) is very simple: stop eating and keep on checking your blood glucose levels. My migraineurs are asked to not eat until their blood glucose levels dips well below 99 mg/dl—preferably between 70 and 95 mg/dl. Getting down to this low blood glucose may take several days of not eating! If a migraineur is not on any psychotropic or heart medicines, the ketogenic diet I specifically formulated for migraineurs is the best option.
If the migraineur has reactive hypoglycemia, fasting is not an option, since their blood glucose level can drop below healthy minimum levels, endangering their lives. In this case, the migraineur moves to the zero carbs diet (all meat and fat, ratio dependent upon certain factors). Without any exogenous easy glucose, the liver must convert glucose from protein for all of the body’s glucose needs and this reduces insulin, since insulin is not spiked by glucose in this case.
Normal hunger is *just hungry* and no urgency. Normal hunger is healthy, and you can continue being hungry for several days without eating without any problems. That’s normal. A normal hunger doesn’t affect your blood sugar in any shape or form, because the liver manufactures the proper amount of glycogen via gluconeogenesis and ketones for the ketogenic metabolic process. Migraine is 100% preventable by a metabolic process that doesn’t use carbohydrates at all or only in minimal amounts. Since a large body of science suggests that metabolic syndrome is driven by excess carbohydrate intake12 (see here and here and here), and it is reversible by carbohydrate restriction (not caloric restriction), it follows that migraineurs recover from their migraines because they are able to reverse their genetic predispositions to carbohydrate intolerance and glucose sensitivity.
Since migraineurs are carbohydrate intolerant and glucose sensitive, they end up with metabolic syndrome if they continue to consume the – for them – offensive substances. This also suggests that each migraineur should be scrutinized by medical professionals to eliminate all opportunities for the development of metabolic syndrome by educating them to remove carbohydrates from their diet.
Support Hormones Matter
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Additional Sources
1 Bhoi, S., Kalita, J. & Misra, U. Metabolic syndrome and insulin resistance in migraine. The Journal of Headache and Pain 13, 321-326, doi:10.1007/s10194-012-0416-y (2012).
2 Casucci, G., Villani, V., Cologno, D. & D’Onofrio, F. Migraine and metabolism. Neurological Sciences 33, 81-85, doi:10.1007/s10072-012-1047-4 (2012).
3 Fava, A. et al. Chronic migraine in women is associated with insulin resistance: a cross-sectional study. European Journal of Neurology 21, 267-272, doi:10.1111/ene.12289 (2014).
4 Guldiken, B. et al. Migraine in metabolic syndrome. Neurologist 15, doi:10.1097/NRL.0b013e31817781b6 (2009).
5 Sachdev, A. & Marmura, M. J. Metabolic Syndrome and Migraine. Frontiers in Neurology 3, 161, doi:10.3389/fneur.2012.00161 (2012).
6 Salmasi, M., Amini, L., Javanmard, S. H. & Saadatnia, M. Metabolic syndrome in migraine headache: A case-control study. Journal of Research in Medical Sciences : The Official Journal of Isfahan University of Medical Sciences 19, 13-17 (2014).
7 Shaw, S. W., Johnson, R. H. & Keogh, H. J. Metabolic changes during glucose tolerance tests in migraine attacks. J Neurol Sci 33, 51-59, doi:10.1016/0022-510X(77)90181-2 (1977).
8 Sinclair, A. J. & Matharu, M. Migraine, cerebrovascular disease and the metabolic syndrome. Annals of Indian Academy of Neurology 15, S72-S77, doi:10.4103/0972-2327.100015 (2012).
9 Winsvold, B. S. et al. Migraine, headache and development of metabolic syndrome: An 11-year follow-up in the Nord-Trøndelag Health Study (HUNT). PAIN® 154, 1305-1311, doi:https://doi.org/10.1016/j.pain.2013.04.007 (2013).
10 Atlas, S. A. The Renin-Angiotensin Aldosterone System: Pathophysiological Role and Pharmacologic Inhibition. Journal of Managed Care Pharmacy 13, 9-20, doi:10.18553/jmcp.2007.13.s8-b.9 (2007).
11 Bhoi, S. K., Kalita, J. & Misra, U. K. Metabolic syndrome and insulin resistance in migraine. J Headache Pain 13, doi:10.1007/s10194-012-0416-y (2012).
12 Volek, J. S., Fernandez, M. L., Feinman, R. D. & Phinney, S. D. Dietary carbohydrate restriction induces a unique metabolic state positively affecting atherogenic dyslipidemia, fatty acid partitioning, and metabolic syndrome. Prog Lipid Res 47, doi:10.1016/j.plipres.2008.02.003 (2008).












It seemed really obvious to me that my headaches/migraines are related to metabolic syndrome but I recently got a blood glucose monitor and my fasting glucose is around 4.8 mmol/l, which is below the 5.5mmol/l that you state. I have started to take walks after I eat and that seems to help so much! I am worried about going fully keto because of all the saturated fat and so I’m just taking in carbs around where I’m most active. In the morning before I go to work, I don’t eat any carbs but for lunch and dinner I do and then exercise after. Do you think saturated fat is something I need to worry about when going fully keto? Heart disease runs in my family and so I don’t want to clog up my arteries. I am even worried about eating eggs daily… I just haven’t seen many research papers on long term keto and literally every health organization doesn’t recommend to have a high fat intake. This is why I’m so hesitant. Any direction with what I have brought up would be amazing. These headaches really are affecting my life. Vitamin B2 seems to be helping the most, further validating it’s a metabolic problem…
Dear Dustin,
Fasting blood glucose is not a good measure of metabolic disease because the blood glucose levels are kept low by active–often very high levels of–insulin. The first few stages of type 2 diabetes are NOT high blood glucose but rather high blood insulin. It is a very big mistake that insulin is rarely if ever checked by medical professionals, since that is much more telling than fasting blood glucose. In fact, if you read the book “Diabetes Epidemic & You” by Joseph R. Kraft MD MS. FCAP, you will find that over 85% of the people with full blown type 2 diabetes have completely normal fasting blood glucose!
To evaluate whether you have a metabolic disease or not, you really need to get the following blood test, all fasted tests: insulin, c-peptide, CRP, triglycerides, HDL, eGFR, and blood pressure. Depending on the lab you are working with, ranges tend to differ, so let me give you a guideline so you can understand your blood test result even if your doctors and lab mark OK for all, because 99.99999999999% of the times they will mark “normal” when, in fact, it is not normal.
Insulin: ranges vary but if the range is 22-40 your insulin should be around 23-25. If 2-22, your ideal is around 2.5-4. If higher, you have high insulin.
C-peptide: this measures how well your insulin is being released. The range may be 0.51 to 2.72 or 0.17-0.90. The ideal is 0.6-1 in first case and 0.18-0.2 in the second case
CRP: this is c-reactive protein, which is associated with vascular inflammation. Normally I see ideal 0-3 but I have seen different ranges. If this is the range you get, you need to be <1, typically <0.5
Triglycerides: represents the amount of triple-fatty-acid chain capped by a glycerol cap in your blood. The liver deposits this as fat and is also using this for gluconeogenesis to create free fatty acids your body uses as fuel, and the glycerol cap is what then formulates glycogen. This should be 0.508 – 0.9 mmol/L (45-80 mg/dL).
HDL: This is high density lipoprotein and it should be >1.56 mmol/l (60 mg/dL), ideally >20.7 mmol/L (80 mg/dL)
The modern risk score can only be calculated by mg/dL numbers: triglycerides/HDL and ideally this number is 0.6 < 1, if it is 1 -< 2 it is OK, and 2 -< 3 it is acceptable. >3 is trouble
eGFR: this is the measure of how well your kidneys filter your blood. This number is usually reduced to show >60 when [people are metabolically compromised. Ideally this number is >90, though this is only reported this way in very few countries. In most Western places, and especially in the UK, it is noted as >60 is OK but that is actually stage 2 kidney disease but no kidney damage yet.
Blood Pressure: the ideal blood pressure is noted as <120/80 but of course 0 is less than 120/80 so clearly this is false. Thus the good range is 90-120 in systolic (first number) and 50-80 the diastolic (second number), and equally importantly there should be 40 point difference between the systolic and diastolic.
So if you pass these tests with flying color and also have a good fasting blood glucose, which is considered good between 3.61-5.6 mmol/L (65-100 mg/dL), but actually the ideal is between 4.5-5.5 mmol/L (80-99 mg/dL), then you can say you have no metabolic disease. You may also consider and oral glucose tolerance test (OGTT).
In terms of the rest of your questions about exercise and carbs: if you eat carbs when you are most active, it is guaranteed that your muscles will be burning glucose instead of fat. If that’s your goal, by all means, just note that your body’s primary fuel is actually fat. This is why the liver keeps carbs in the form of triglycerides for future use. The only organ in the body that needs glucose is the red blood cells and nothing else! The heart, for example, prefers fat over all else and gets into trouble from having to use glucose (in anaerobic state it must, so avoid exercises like spin classes with long anaerobic state. A great way to get the heart damaged).
As for saturated fat and your family:
1) Your family: your family history is not your genetics. That history shows that they all ate similar foods and thus all ended up with similar diseases. Neither heart disease not diabetes is genetic; the predisposition to these is genetic! So if you change what you eat relative to your family members, your health outcome will differ.
2) Saturated fat: Humans evolved eating saturated fat. It’s not like we had soy oil or avocados we could eat all day long hundreds of thousands of years ago–especially because there was also a giant ice age, which our ancestors lived through and painted on the cave walls what they ate. The foods they painted are all herbivores–aka red meat. We evolved eating that. If it were unhealthy for us, humans would have gone extinct ages ago. What causes heart disease is metabolic disease and that is caused from all these completely unnatural carbs and vegetable/seed oils in our lives that have not existed in our evolution.
If you want to be healthy, avoid carbs like the plague–you can eat fresh leafy veggies if you like but avoid all starches, grains, sugar and other sweeteners, processed foods, junk foods, low fat foods. Eat healthy whole foods that you cook from scratch, and which contain lots of meat and eggs and a ton of saturated fats, also eat fish/seafood for its nutrients. Our body fat composition in terms of what fat we are made of: saturated fat. your brain is over 85% fat and cholesterol. Don’t fear eating fat and cholesterol. Your entire body needs it.
As for long-term keto: you were in ketosis in your mom’s womb, were born in ketosis, and remained in and out of ketosis through age 10! Read this article in which I listed academic articles you can read on the matter.
Good luck to you,
Angela
I felt like a lot of things you said made sense. I am the mother of a 16 year old who has suffered from severe migraines since she was 9. Hospitalized 3-4 times a year with status migrainosus. Skinny fat, BMI of 18… with almost 29% of body fat. low blood sugar, high estrogen, etc. we have tried everything. Currently on gabapentin as a prophylactic, metformin. Neurologist, Nutriologist and endocrinologist working together. 0 carbs on diet . Feeling desperate ! We live abroad and are looking for help as we have exhausted all options. I appreciate if you can suggest where to seek for help.
Dear Johanna,
I am very sorry to hear about your daughter. But there is hope, since in my Facebook migraine group there are lots of parents helping their children, and you can too. Please join my Facebook migraine group here. And you should read the book: “Fighting The Migraine Epidemic: Complete Guide: How to Treat & Prevent Migraines Without Medicines” that is sold on amazon–the e-book only from amazon US.
I am looking forward to seeing you in the group! 🙂
Angela
Thank you so much for taking the time to get back to me. I will join your group for sure !
I was interested by this article because I recently cured my roaring tinnitus and deafness and dizziness (vestibular migraine?- sudden onset, weekly bouts of vertigo lasting 6 hours,) with vitamin e supplementation, having lately resolved life long joint pain in knees and lower back and NAFLd with keto diet, have suffered hypoglycemia for ever, (used to consume a kilo of sugar weekly, eating carbs makes me feel hungry immediately) had migraines with cyclic vomiting as a child and wondering if all these are linked through a metabolic syndrome. My daughter started having TL CP epileptic seizures at 14 years, ( now 24) never fully controlled, occur around menses and ovulation and more lately periodic muscle spasms / loss of muscle tone throughout body. Spasms and muscle tone loss occurs after eating carb rich meals. Really determined to get to the bottom of this and grateful for any suggestions of further research published in this area.
Dear Richard,
Migraine is caused by electrolyte imbalance, which is exacerbated by glucose from carbs. Migraineurs are carbohydrate intolerant and glucose sensitive. I have not yet found a migraine sufferer who also didn’t have metabolic disease. So the two tightly interconnect. I have a couple of migraine groups on Facebook (protocol group here and keto group here) and a book (here) that explains what migraine is. I recommend you and your daughter read the book and join the migraine group(s) to help guiding you/her further.
Best wishes,
Angela