Fitness and survival are by nature estimates of past performance.
George Wald
Reconsidering Genetic Mutations: What is Baseline?
Each person possesses a set of genes that belongs to that person only. It is not possible to state what the “baseline” human genetic makeup is; we can only look at phenotypes (observable characteristics or traits) and the genetic makeup of what, on average, we are today. We use the average of these genetic commonalities to establish the baseline from which each person differs to some degree. How we interpret what we end up with using such averaging is the question of this paper. In my view, the genetic commonalities of today’s humans are not a baseline since it implies that everything that came before the current form is ignored; or if that form shows up as a result of atavism, we consider that as mutation (in a negative sense) away from the “norm” that needs to be medically treated. There is something wrong with this.
What is baseline as far as genetics are concerned is an important question. It determines how we view genetic differences e.g. whether those differences represent negative or positive changes or no changes at all. This question came up in my research looking at genotype and phenotype variances associated with migraines. Migraine is considered to be a neurological disorder that is treated with dangerous drugs that don’t cure migraines, and only try to reduce symptoms. These medications often leave migraineurs with permanent side effects.
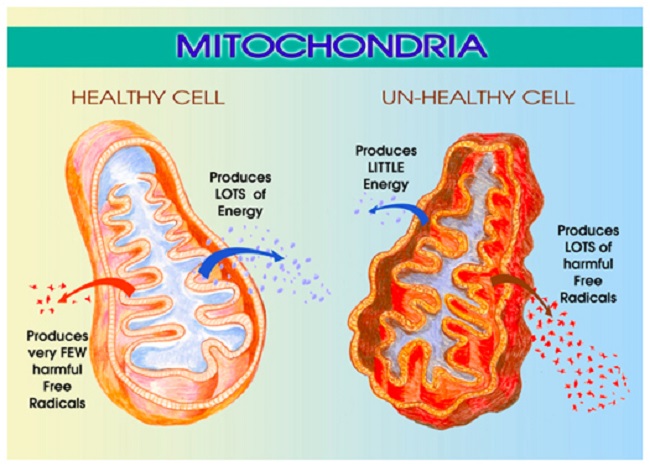
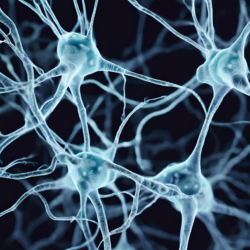
Migraineurs are very sensitive to their environment because their sensory organs (nose, eye, ears, touch, taste) are more sensitized. Such hyper-sensitive sensory organs and the associated sensitivity (1) are considered to be disorders in childhood and phantom hallucinations in adulthood (2) that need medical treatment. Yet these are not hallucinations. Hyper-sensory organs are more sensitive to stimulation and detect smells, sounds, sights, tastes, and touch more vividly than those without such neurons. Unfortunately, migraine also comes with disabling prodromes, pain, and postdromes that place migraine into a disorder category. While research is focusing on medicines to reduce or prevent pain, why not focus on the cause of and reason for the pain? After all, this highly sensitized brain must have yielded evolutionary benefits to have become the 3rd most prevalent illness in the world, representing 15% of the (diagnosed) population.
Over the many years of my migraine research, I have been able to teach thousands of migraineurs (myself included) to induce, abort, and prevent migraines without the use of any medicines. If a condition can deliberately be induced, aborted, and prevented, it cannot be a disease. It certainly comes with a host of genetic differences from those without migraines, but differences need not be disorders. This prompted me to ask a very important chicken or egg question: Did the hyper-sensory “on alert” brain of migraineurs or the less sensitive brain of non-migraineurs come first? This question doesn’t aim to establish what is normal but it certainly aims to establish the baseline. If the baseline brain is the hypersensitive brain (my hypothesis), then why not learn to feed the nutrients it needs so that it experiences no pain?
We consider evolutionary adaptations as those genetic changes that improve the survival chances of the organism. The brain that smells hears, and sees better is a survival advantage. In ancient times, it was important to smell a lion in the bush miles away or feel weather changes by barometric pressure change or the movement of a single leaf even if the actual change was far away in time or place. The hypersensitivity of the migraine brain is similar to the hypersensitivity of the mammalian brain, where not being alert is equal to becoming food. Alertness is not just mammalian—all wild creatures have hypersensitivity to their environment. Based on mammalian facts, my theory is that the brain of migraineurs is the original brain and those without migraines had the good fortune to adapt to changing lives as a result of a series of genetic variances that became adaptations. Does genetics support my hypothesis?
Mutation, Adaptation, Variant, Trait, and Epigenetics
In the GeneCards database, one can search for the many genes associated with traits and health conditions. However, a gene may be associated with many unrelated traits and health conditions. There are several genes connected to migraines—each of these genes has a different representation in those without migraines. The trick is to understand what the differences may mean and how those manifest themselves in a population.
The word mutation is often used to describe genetic changes, although change has a neutral meaning whereas mutation doesn’t. “A Mutation occurs when a DNA gene is damaged or changed in such a way as to alter the genetic message carried by that gene.” (source) A mutation is permanent. Mutation is either damage or adaptation. Damage, of course, is a mutation with negative consequences to the organism. Adaptation is a long-term change in behavior, physiology, and structure of an organism such that it becomes suited to the environment, and the traits acquired are passed on to future generations. An adaptation is thus an improvement in terms of the fitness of the organism. Adaptations imply evolutionary beneficial changes to the species. Major changes are made up of many small changes over time that remain and collectively create an adaptation or a mutation.
These small changes, and variations, occur all the time to each of us. Many modern variations (also called variances or variants) lead to negative consequences, because they may modify the fitness of the species without adaptation or mutation. Variances are transfers of a single nucleotide in the DNA sequence (adenine A, cytosine C, guanine G, or thymine T), such as an A changed to a C, for example. Variances are often referred to as variants or SNPs in the medical literature. A single variant may or may not bring about any change, depending on its inheritance or mechanism. In some conditions, a single SNP can make a difference (autosomal dominant) or not if recessive. A collection of SNPs may lead to specific traits that are observable by physical attributes (such as hair color or height).
Many modern health conditions, such as diabetes mellitus (type 2), are made up of many thousands of SNPs and without becoming an adaptation or a mutation are passed to future generations. This is a health concern that evolves as a result of epigenetic forces acting on the SNPs. Epigenetics greatly influence SNPs and can cause an endless variety of changes based on the available chemicals in the gene’s environment. Epigenetics need not exert its influence from the external environment but can equally (and more likely) do so from internal stressors, such as insulin resistance in response to carbohydrate consumption by those who are sensitive to or cannot digest glucose or fructose.
The Case of Red Hair: Mutation? Adaptation? Variance?
The MC1R gene, which some of us carry, is important for the red hair trait. Is red hair a mutation, an adaptation, a variant, or none of the above? If the MC1R existed in our ancient relatives that are now extinct, such as the Neanderthals, then it cannot be considered a mutation in modern humans since it happened before humans existed. As it turns out, the Neanderthals had the MC1R red hair genes, thus the MC1R variant is part of our human baseline (3). Red hair does not come from the MC1R gene alone but the variants of 1994 genes participate in the creation of red hair (4). The importance of this is the length of time that passed between the first appearance (as far as we know) of the variation of this gene and the number of variances it takes to create red hair. That is because older traits that have been with our ancient relatives, and are still with us today, have very few variances; they are stable.
The question then is as follows: was the MC1R a prehistoric mutation some of us still carry? If so, its definition of mutation in modern human genetics is incorrect. MC1R existed before modern humans, and therefore it is not a mutation but a baseline trait. Those who don’t have the MC1R gene are perhaps the ones who mutated, adapted, or changed. Red hair is still found today, but no medical authority suggests that we should medicate against red hair.
It appears that the more ancient a trait, the slower the variance rate (fewer variants), thereby indicating that a closer state to baseline is one with fewer variants: more ancient traits moremore ancient have fewer variants either because they are more stable or they represent a sub-population with a common ancestor. While this statement may find many opponents, the EDAR gene study, searching why an East Asian sub-population has different traits from the rest of East Asia, noted that it
“is striking that there are only 35 nonsynonymous variants in our entire list of candidates. Based on the genomic coverage of the 1000G data, we estimate that there are no more than 38 candidate causal nonsynonymous SNPs in the 412 candidate selected regions we analyzed… These data suggest that only a minority of recent adaptations are due to amino-acid changes and that regulatory changes are likely to play a dominant role in recent human evolution.” (5)
The EDAR gene, a single gene, with its SNPs affected a multitude of changes in a population, providing the East Asian sub-population with strong hair, smaller breast, different sweat glands, and a host of other differences over 10,000 years ago. In this case, a single functional genetic variant was deleted from the genome and that brought about a major change that acts on many traits. A variant like this is neither a mutation nor an adaptation. On the other hand, there are conditions in which hundreds or thousands of SNPs are required to bring about a single change, such as cleft palate (1855 genes)—possibly since this is an undesired trait for fitness and many dominoes must fall in place to inherit the entire set of variances to end up with cleft palate.
This clearly makes the statement that modern diseases (Alzheimer’s, cancer, etc.,) are not easy to genetically replicate and pass on to future generations. To do so, epigenetics must push its force of influence on many genes to produce variants. Epigenetics can become an undesirable force by, for example, what we eat, how much sleep we get, or what medicines we take. Our modern diet is over-saturated with sugar and grains, placing a giant pressure on our immune system—neither sugar nor grain metabolism was part of our ancient original set of genes and so they force variances that can be random. The ensuing health conditions make the roulette wheel spin, stopping anywhere and causing SNP-based changes.
Modern diseases have a very large number of SNPs that are disadvantageous so they cannot be adaptations (cancer, Parkinson’s), whereas adaptive changes have few SNPs (source). This makes a lot of sense since changes that are advantageous to the species need to be stable to easily pass on from generation to generation, whereas disadvantageous changes would be selected with a very large number of SNPs such that passing on the trait becomes difficult. For example, the research found that lactose tolerance adaptation occurred by several human groups around the globe about 3,000-7,000 years ago independent of whether a particular group drank milk or not. Lactose tolerance (lactase tolerance) and lactase persistence have only 20 and 26 SNPs, respectively. Contrast this with breast cancer and its 7,487 SNPs, a modern disadvantageous condition best not be passed on to future generations.
With all these complications, how do we establish if a trait is ancient or modern? And how do we know if it is a mutation, a variance, or an adaptation? This is a much more complex question than it appears and an answer to this is not straightforward at all.
Genetic Variance and Genetic Baseline
There are conflicts within the theory of variants and establishing the default—the baseline. For example, a study suggests that brown eye is the default from which the changes went in the following direction:
brown (904) ==> green (781) ==> blue (1092)
where SNP numbers are in parentheses. Note the number of SNPs would hint that green eyes may have been the default and so based on the number of SNPs, the most stable would set the baseline and give rise to variances from there on:
green (781) ==> brown (904) ==> blue (1092).
The interpretation of what SNP means is not clear for all, nor is it clear how to interpret SNPs when some point to one thing and others point to another. The only thing that we can reliably state is that it hints at the age of the variance but we cannot draw any other conclusions.
Is the Migraine Brain a Mutation or the Baseline?
Migraine is the baseline because of the small number of variances. Returning to the subject of my interest: the similar traits of migraineurs, whether migraine is a mutation (as it is referred to and medicated as a result) or the baseline for the human brain based on the brains of our ancient ancestors. You need to be a member of the Facebook migraine group to appreciate how much migraineurs are like siblings. Sometimes we run surveys. Migraine has 1293 SNPs.
Two recent surveys:
- Ehlers-Danlos Syndrome (EDS), which is associated with hypermobility and vascular differences, was a fascinating find. EDS is very rare, found in only 1 out of 5000 (0.02%) people in the US. Yet over 60% of the surveyed migraineurs have at least one type of EDS (there are several types). EDS has 121 SNPs. The overlap between EDS and migraine SNPs is also significant: 43% (52 out of 121) of EDS SNPs are also found in migraine SNPs. The conditions must be related—perhaps a common ancestor.
- Raynaud’s syndrome is also rare; it is present in 1 out of 20 people (5%) in the US. Yet over 70% of the migraineurs surveyed have Raynaud’s. The SNP count for Raynaud’s is 88; 68% of the SNPs in Raynaud’s are part of the migraine SNPs. The two conditions must therefore also be related–perhaps common ancestor here too.
EDS and Raynaud’s also overlap with each other; 16% of the SNPs in Raynaud’s are also in EDS and 12% of the EDS SNPs are found in Raynaud’s. It appears that the two conditions are also related and both are related to migraine. While I can certainly explain the reason for the evolutionary benefit of the genetic adaptations for both Raynaud’s and EDS, I have a different point to make here.
Note that Raynaud’s phenomenon has 88 SNPs, EDS 121, and migraine 1293. These are small stable numbers (blue eyes 1092!), indicating how ancient they are and that they may indeed be related to one another. After my lengthy introduction, this is my point: Raynaud’s, EDS, and migraine are not mutations but are variances that over time turned into adaptations that in ancient times served a benefit. The percentage of people afflicted with migraines is too large and they have too many similar traits to be considered a random mutation. If the hypersensitive migraine brain is an adaptation that serves an evolutionary benefit, why do we medicate it rather than feed it the way an ancient brain would have been fed? During the ancient time when migraine brain, EDS, and Raynaud’s were important and beneficial, there were no soft drinks, smoothies, cakes, bread, and pasta on every corner. We need to respect who we are and eat for our brain.
Conclusion
Migraine is specific to a population subgroup with ancient traits that were essential in our ancient past. Today, many of the benefits of a migraine-brain are troublesome (hypersensitive sensory organs that use more voltage) and migraine is associated with glucose (6) and fructose intolerance that lead to migraineurs’ metabolic syndrome (7-10). By getting rid of glucose and fructose in the migraineurs’ diet, migraine can be completely prevented. We need to re-evaluate the medicating of migraineurs by downregulating their hyper-sensory organs. Migraine pain is fully preventable without any medicines by simply feeding this ancient brain ancient type food!
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Image by Pete Linforth from Pixabay.
This article was published originally on April 6, 2017.
References
- Schwedt TJ (2013) Multisensory Integration in Migraine. Curr Opin Neurol:248-253.
- Coleman ER, Grosberg BM, & Robbins MS (2011) Olfactory hallucinations in primary headache disorders: Case series and literature review. Cephalalgia 31(14):1477-1489.
- Lalueza-Fox C, et al. (2007) A Melanocortin 1 Receptor Allele Suggests Varying Pigmentation Among Neanderthals. Science 318(5855):1453-1455.
- Science WIo (2017) The Human Gene Database. in GeneCards: The Human Gene Database, ed Science WIo (Weizmann Institute of Science, Internet), The Human Genome Database.
- Grossman Sharon R, et al. (Identifying Recent Adaptations in Large-Scale Genomic Data. Cell 152(4):703-713.
- Mohammad SS, Coman D, & Calvert S (2014) Glucose transporter 1 deficiency syndrome and hemiplegic migraines as a dominant presenting clinical feature. Journal of Paediatrics and Child Health 50(12):1025-1026.
- Salmasi M, Amini L, Javanmard SH, & Saadatnia M (2014) Metabolic syndrome in migraine headache: A case-control study. Journal of Research in Medical Sciences: The Official Journal of Isfahan University of Medical Sciences 19(1):13-17.
- Sachdev A & Marmura MJ (2012) Metabolic Syndrome and Migraine. Frontiers in Neurology 3:161.
- Bhoi SK, Kalita J, & Misra UK (2012) Metabolic syndrome and insulin resistance in migraine. The Journal of Headache and Pain 13(4):321-326.
- Guldiken B, et al. (2009) Migraine in Metabolic Syndrome. The Neurologist 15(2):55-58.










Incredibly informative and interesting article! Thanks to it, I discovered a lot of new information for myself. In fact, I suffer from migraines from early childhood. I even believe that from my birth) I am very sensitive to weather changes, as I feel in advance any weather changes through the prism of migraine and overall poor health. But the worst thing for me is the duration of a migraine. It can last from one to three days! These are unbearable torments for me. I use the medicines that my doctor prescribed for me, but they only help for several hours.
By the way, thanks to your article, I understood why I am very sensitive to the environment, especially through my nose and eyes. It turns out that this is all interconnected. I did not know about this before.
Thank you for your researches! I look forward to new articles)
Dear Menopause Relief,
Thanks for your comment. It seems your migraines are the most common “classic” migraines that last for 3 days. Please join my Facebook migraine group so we can help you learn how to prevent them.
Best wishes,
Angela
I’ve suffered migraines since childhood. My mother would give me salt. I never understood until now. Almost all female members of my paternal family suffers migraines. My 9 ur old granddaughter was diagnosed last month at Childrens Hospital St. Louis with super Imposed migrains.
I came you while researching serotonin syndrome. I am having great difficulty reading your article. I am kicked out every half paragraph, unable to enter back into the subject at all. So i tried by looking up by author and found this. Very insightful. At 58 yrs with many neurologic “manifestations” that i’m dealing with. I’m looking forward to more articles.
Thank you for you research
Dear Amanda,
Sounds like your mother was way ahead of her time (and ahead of all medical research and doctors even of today!). I am sorry you had a hard time with the webpage. Sometimes the internet is just that way. Let me know if you would like me to email you a PDF copy for easier reading.
As for your daughter, there is never a better time to start her on a nutrition plan that will be migraine preventive. Adding salt to the diet is great–adding salt after a meal is even better (use salt capsules if she doesn’t like the taste of salt and can swallow capsules). The most important thing though is cutting out all sweets. It is not nearly as hard on children as we adults think it is. They really do listen and pay a lot more attention than we give them credit for. They are also a lot smarter than we think!
I had proof of that this past weekend when my granddaughter (almost 13) pulled my son out of a migraine (after eating chocolate) by having salt packets in her little purse!! I only treated her with salt once in her life for a tummy ache and headache after eating too much sweets (salt reestablishes electrolyte) and look how she now carries salt and was able to help her dad!! They are really clever.
So start early with you daughter; she will learn really quickly what she can and cannot eat. <3
In terms of serotonin syndrome, I have an article on that as it killed my mom. And here are some additional articles on migraines: here, here, and here. I will have more coming up in the future so keep an eye on this blog. 🙂 I write on both migraines and nutrition.
Best wishes to both of you,
Angela