When people have had a prolonged deficiency in energy metabolism, sometimes for years, their symptoms are frequently not recognized for what they represent. Because energy is required for every cell in the body, the symptoms are caused by how many cells have become dysfunctional. The brain and heart are the organs that dominate the consumption of energy, explaining why changes in behavior, organic brain disease and heart disease are so common. The symptoms, referring to the complaints of the patient, are all interpretations by the brain. By far and away the commonest symptom is chronic intractable fatigue and the accompanying symptoms have given rise to a common diagnosis called Chronic Fatigue Syndrome (CFS). A patient has been described whose CFS was found to be due to a genetic defect in the mitochondria, the organelles within the cell that produce energy. How often there is a genetic risk is unknown but the new science of epigenetics tells us that genes seldom work on their own. Another factor (malnutrition, stress) usually comes into the equation in order for the gene to be expressed in disease.
Anabolic and Catabolic Metabolism
Metabolism is the name for the sum of chemical reactions taking place in the human body. Because some reactions break large molecules into smaller pieces, while other reactions build up larger molecules from constituents, metabolism subdivides into two categories, catabolic and anabolic. Anabolic metabolism refers to reactions that build up molecules while catabolic metabolism breaks them down. Anabolic processes require energy derived from oxidation of food, while catabolic processes release energy by the oxidation of the molecules derived from constituents as they are broken down. These two functions must necessarily be in relative balance in a fully grown healthy person because, when growth is completed, a steady body weight results. Anabolic function dominates in the growth of a child, becoming balanced when growth is completed. In a lifespan, normal energy metabolism derived from oxidation of naturally occurring food substances gradually deteriorates and during aging, catabolic metabolism begins to dominate the balance, explaining the tendency to shrinkage in the elderly person. Anything that affects the oxidation of food substances in energy production results in an abnormal balance between the two types of metabolism. Thus, starvation, an improper ratio of calories to non-caloric nutrients, or genetically determined factors result in dominance of catabolic metabolism.
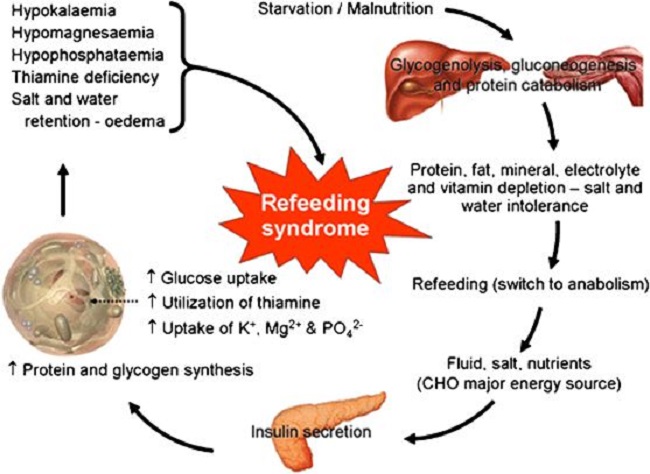
Refeeding Syndrome
Refeeding syndrome is what happens when an individual’s long-standing state of catabolic metabolism is too rapidly treated with the necessary nutritional ingredients to restore the metabolic balance. Attempts to treat the chronic starvation of incarcerated victims in the Nazi -controlled camps after World War II resulted in death in many of them. It is a dangerous condition that occurs with reestablishment of adequate nutrition in malnourished and cachectic patients. More specifically, its occurrence has been reported during oral enteral and parenteral refeeding. I remember the case of a boy who was a “junk food junky”. He had just come down from a rope that he had been climbing in the gymnasium, illustrating his apparent physical fitness, but he then suddenly passed out. He was taken to a local hospital by ambulance when he was given glucose saline intravenously, a standard procedure. He had a series of bloodstained bowel movements and expired. We have known for years that introducing glucose intravenously to a long-standing thiamine deficient individual is dangerous. But how would this come to light in an emergency situation? To prevent the possibility of refeeding syndrome would demand the reason for this young man passing out be known in relation to his junk food diet.
Clinical features of refeeding syndrome are fluid-balance abnormalities, abnormal glucose metabolism and a deficiency of magnesium and potassium. In addition, thiamine deficiency dominates. Refeeding syndrome reflects the too rapid change from catabolic to anabolic metabolism, is often undiagnosed and some clinicians remain oblivious to its occurrence. Recognition reduces morbidity and mortality but there is no universal agreement as to its definition. A report exploring refeeding syndrome across seven cases found that each showed deficiencies and low plasma levels of potassium, phosphate, magnesium and thiamine combined with salt and water retention. It is interesting that salt and water retention are typical of thiamine deficiency. Similarly, a report exploring the incidence of Wernicke’s Encephalophy with anorexia nervosa found that 8 of 12 cases of anorexia investigated were afflicted with the full symptoms of the thiamine deficiency brain disease known as Wernicke encephalopathy. Anorexia affects 2.9 million people worldwide and is generally considered to be psychiatric loss of appetite. Both its active state and refeeding can be lethal.
Guidelines for refeeding patients with anorexia have been published by the European Society of Clinical Nutrition and Metabolism. Of 65 in-hospital patients studied, 14 were admitted more than once within the study period. Nine patients had minor complications in the first 10 days of replenishment. Four patients had transient pretibial edema (simple pressure with a finger below the knee resulted in dimpling). Three patients had what was described as organ dysfunction and two patients had severe hypokalemia (low potassium in the blood), all of which have been described as typical of thiamine deficiency. In fact, pretibial edema can be the only clinically obtainable evidence of thiamine deficiency. There is a high prevalence of thiamine deficiency in cancer patients. The prevalence of malnutrition is high in head-neck cancer patients, many of whom require artificial nutritional support or refeeding intervention. Refeeding syndrome is commonly encountered in the nutritional treatment of critical illness. However, guidelines and its occurrence in ICU patients remain unclear. Calorie restriction for several days and a gradual increase of its intake has been recommended. Thiamine deficiency brain disease is not too uncommon in parenteral nutrition. It has been reported that refeeding syndrome occurs in 4% of cases of parenteral nutrition, but failure of its recognition occurs in 50%.
Refeeding, Paradoxical Reactions, and Side Effects
Discerning readers of Hormones Matter have probably noticed that the subject of “paradox” has been mentioned a number of times and some time ago there was a comment that an article on the subject might be relevant. “Paradox” is a less severe form of RFS, a term that I have used to indicate that the patient’s expectation of improvement by nutritional replacement is often dashed because the symptoms become worse. Obviously, because pharmaceuticals are the usual and customary form of treatment, the worsening of symptoms immediately gives rise to the patient’s deduction that these are side effects. In a sense, they are indeed side effects, but the mechanism is very different from that caused by pharmaceuticals. The accentuation of symptoms represents a sudden switch from the prolonged state of catabolic/anabolic balance to that of anabolic/catabolic balance, whereas side effects of drugs are a direct effect of toxicity. This accentuation of symptoms seems to be directly related to the chronic nature of the malnutrition. It means that the unfortunate patient has been suffering for an extended period without the symptoms being recognized for what they represent. If the symptoms are correctly diagnosed at the outset of symptoms, the nutritional correction is easy and occurs rapidly. Paradox is because recognition comes after protracted malnutrition and is much more likely with intravenous nutritional correction. I always warned the patient before administration. However, the paradoxical worsening of symptoms may last as long as a month when vitamin therapy is used in oral administration. I have always told the patient that paradox is the best sign of ultimate improvement. For example, I was discussing the common symptoms of high calorie malnutrition with a nurse. She interrupted by telling me that I was describing the symptoms that she had been suffering for years. I suggested the nutrient replacement and she told me later that paradox had lasted for a good month but was then replaced with an absence of symptoms and an energy level that she had never previously experienced.
Modern Malnutrition
Readers must understand that chronic long-term malnutrition is common in America. However, it is not the same as the kind of malnutrition that is seen for example in Bangladesh, or that seen in advanced cancer, known as starvation. The kind of common malnutrition in America is because of an excess of calories and is often seen as an oxymoron. How can a high calorie diet possibly cause a potentially severe illness? The clinical expression of starvation is that of bodily attrition through catabolic breakdown leading to death, the kind of clinical situation underlined by Mother Teresa and caused by lack of any sort of food. People with high calorie malnutrition look entirely different and often constitute what I call the “walking sick”, because they are commonly seen as “problem patients” in the offices of physicians. They are often obese and their many complaints are most often diagnosed by physicians as “psychosomatic”. Their problem is too much food of the wrong sort. Thiamine/magnesium levels in the blood are usually perfectly normal if they are ever measured, giving rise to a physician’s refusal to diagnose the “absurd idea of a vitamin deficiency”. Thiamine activity is inside cells, so finding it in the liquid part (plasma) of the blood is meaningless. Like a “choked car engine” the non-caloric nutrients are overwhelmed by the excess of “empty” calories. It is energy production that is the core issue and is the reason for the multiplicity of symptoms. This is particularly true for deficiency of thiamine and magnesium because they are so essential to the processing of simple sugars. The indiscriminate ingestion of sweets has become a national calamity. Of course, thiamine and magnesium have to cooperate with many more non-caloric nutrients but their position in metabolism dominates the function of energy production.
So, high calorie malnutrition is an example of the effects of extremes, too much versus too little. The brain, heart and nervous system are the most affected organs because of their high energy requirement. The commonest symptom is fatigue but other common symptoms include “brain fog”, insomnia, a perpetual sense of anxiety or fear, heart palpitations, migraine, tension headaches, poor tolerance to heat and cold, unusual sweating particularly at night, diarrhea alternating with constipation, pins and needles in the extremities and vicarious body and limb pains. Because physicians in America have denied the possibility of vitamin deficiency disease, they usually interpret any abnormal laboratory studies to what they consider to be well-recognized and common diseases such as chronic fatigue syndrome. If lab studies are normal, then it is deemed to be “psychological”, a very unsatisfactory explanation to the patient.
When a person has been consuming simple carbohydrates in the form of sweets, including carbonated beverages and alcohol for a prolonged period, the general efficiency of cellular metabolism gradually declines. The three meals a day in some cases may be perfectly adequate but the dietary excesses may come for that person because of “the goodies” associated with social activities. Because the brain is most affected, the symptoms will be generated by the biochemical and electrical changes that follow. The symptoms are so variable that listing them all is virtually impossible. It has long been known that beriberi, the clinical expression of thiamine deficiency, had a long morbidity and a low mortality. The suffering experienced during its prolonged course was (and still is), however, an abysmal reflection of medical ignorance.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
This article was published originally on July 29, 2019.













This describes me perfectly. I am over weight yet I have severe MECFS and long covid. I was degenerating and becoming cachexic until I took B1 megadose.
I took 5 grams the first day and second day. By the third day only 2 grams seemes sufficient. I have experienced dramatic improvement in my condition however I am eating tons of protein.
I just ate 300g of protein in the last 20 hours. Which I believe is the result of what you mention. Severe catabolism and wasting, to now anabolism.
I’m not sure what to make of this. any advice?
I plan to add a b complex and some minerals soon.
Hi Dr. Lonsdale,
Someone above named Beriti asked this….”I wonder if the diagnoses collagenous colitis is “merely” a gastrointestinal beriberi, and that the world of GI doctors are oblivious of this?”
She said she improved by taking Allithiamine each day. I am curious as to the answer to her question (perhaps you didn’t see her post as you didn’t reply) as my sister also has collagenous colitis and I wonder if she can benefit from B1.
This is a very helpful site and I myself, am just starting a B1 protocol and am having some paradox, so going low and slow! Thank you for all the information which, I’m sure, is helping so many!
Dr Lonsdale, you stated above that:
“I have always told the patient that paradox is the best sign of ultimate improvement”
Do I understand this correctly to mean that a paradoxical reaction is a sure indication of B1 deficiency?
Thank you!
As far as I know, yes.
I am just now learning of thiamine deficiency and trying to understand all of this information. I believe that this is what my 14yo son has been struggling with – for years. He has had mild POTS, oral allergy syndrome, heat intolerance, anxiety, for years! With recent corona virus infection in June 2022 – he’s had lingering gastroparesis. I had narrowed things down to inflammation of the vagus nerve and reactivation of EBV (thought I had not had any testing done – but it made the most sense). Now I am thinking that he has had chronic thiamine deficiency! I started him out on thiamine on a Thursday, by Saturday, he was feeling much better and having more successful bowel movements and less nausea. The next day, Sunday, he’s feeling awful – eye and back pain, nausea, etc…. I am assuming that this is refeeding syndrome/paradox. I want to make sure that I understand what is happening, what I should be doing, etc… – in a nutshell: refeeding syndrome/paradox is a good sign, I am stopping supplementation until these paradox symptoms subside and then I will restart the thiamine at the same dose (50mg/day) until we meet another paradox. Thanks so much!!
You should continue thiamine through the refeeding syndrome and when you begin to see improvement. titrate the dose to the symptoms
If your body isn’t converting the sulfur to sulfate and you might need molybdenum. Google it. And ask your doctor of course.
Miryam, try eliminating the nightshade vegetables from your diet. It took only 4 days of abstinence from potatoes, tomatoes, and any peppers or red spices to end my lifelong IBS symptoms. Nightshades affect acetylcholine.
Dear Dr Lonsdale,
I am so grateful for having come across all the knowledge you share with us. My problems is: In 2010 I was diagnosed with “collagenous colitis” with diarrhea 24/7. I was so sick, and lost 12 kilos in a very short period. Last year I came across your literature on Thiamine, and started supplementing Allithiamine 50 mg a day. Now, my gut is so much better, and I wonder if the diagnose collagenous colitis is “merely” a gastrointestinal beriberi, and that the world of GI doctors are oblivious of this?
Best regards,
Berit
Dr Lonsdale, I’m so grateful for you taking the time to share articles like this; it’s really helpful.
1. Do you have any thoughts on thiamine pyrophosphate vs other types of thiamine? I’ve used the one below, though it’s only a low dose.
https://www.metabolics.com/vitamin-b1-thiamine-pyrophosphate-60caps.html
2. I believe some forms of thiamine are liable to destruction by sulfite. Do you know whether this would apply to thiamine pyrophosphate?
3. Do you think there’s likely a preferable form of thiamine for someone who has problems with brassica vegetables and supplements that promote the production of hydrogen sulfide?
4. Akin to refeeding syndrome, do you think that doing things that increase the metabolic rate are likely to increase need for thiamine? I’m thinking of thyroid hormone replacement therapy, Dr Brownstein / Dr Abraham’s high dose iodine protocol, using MCT oils (or coconut oil which is high in MCTs) and maybe fixing a long-standing other deficiency eg calcium & vit D.
I had some problems with the iodine protocol which were related to other nutrients, but I’m now realising that some of the symptoms might have been due to low thiamine as well (I’d not been supplementing). Some of the bromide detox symptoms that are often cited, and some of the symptoms I had certainly look like thiamine deficiency eg fatigue and slurred speech.
A few years ago I had a lot of health problems and had developed protein energy malnutrition and lost a third of my bodyweight. I was taking B6, biotin and magnesium, but – stupidly – not the other B vitamins. My exclusively breastfed baby was 10 months old, but not yet sitting up and not yet showing any interest in solid food. I started taking some thiamine pyrophosphate (only a relatively small dose) and shortly after, had what appeared to be a big oxalate ‘dump’. A similar time after my baby next nursed, he also had what appeared to be an oxalate dump. The next day, he sat up on his own and started eating food. I think he’d been so low in B1 that it had delayed his development but it was something that was corrected surprisingly quickly.
I was really pleased to see you make a reference in one of your other articles about persistent erections being a symptom of thiamine deficiency. My other child had issues with that for at least two years, and when we eventually got nutritional testing and started giving him vitamins, I realised that it was caused by thiamine deficiency, but I’d never heard anyone else make that connection. My child’s labwork also indicated a substantial deficiency of molybdenum and elevated levels of sulfite.
Later, we changed from TPP to thiamine HCl at a high dose and the metabolic specialists treating him (at one of the very best paediatric hospitals in the country) completely failed to spot that he had a functional B1 deficiency because the type of thiamine wasn’t working for him. Things improved dramatically once we changed to using benfotiamine / allithiamine. Symptoms of thiamine deficiency have included anxiety and outbursts of violence / aggression among many others.
Sorry, I’ve just found your posts on the various forms of supplements, so forget all the questions apart from the one about interactions with sulfite – I’m interested in whether elevated sulfite could cause a lack of response to some forms of B1 supplement. Thank you again for all the helpful information you’ve published about thiamine and other B vitamins.
Hi Dr. Lonsdale,
I’ve gone down to 400mg magnesium, but the diarreah/IBS continues…
REGARDING DIARREAH/IBS:
1. Due to this craziness with the diarreah, I took a blood test. The only anomalies were high whole blood B1 (378.7 nmol/L) and very high B12 (1914 pg/mL)! Is that because I am not absorbing them into my cells? Could that be the cause of my diarreah/tummy upset? (I had not taken a B-complex when starting the Lipothiamine, but had been supplementing the methylated types of B9 and B12, as per previous blood work/instructions from Angela Stanton. She does not recommend complex or multi and i was/am following her migraine protocol.) As you wrote in another article, regarding all the Bs having to work together, could the introduction of the Lipothiamine have triggered other B issues (with B12 or others that the blood test did now show), hence the diarreah? (please note, I had not had a problem with diarreah before Lipothiamine.) Did i mess myself up by not taking a B-complex and multivitamin, at the start of Lipothiamine supplementation, as per YOUR instructions? Should i now stop the B9 and B12 and retake blood work? Or just take a B-complex and multivitamin regardless of this and future blood work? Im afraid of taking too much in a complex and multi, especially since i don’t know if/what I’m absorbing and what’s triggering all this GI garbage…:(
REGARDING ALLITHIAMINE DOSE TITRATION AND PARADOX:
I thought my paradox had subsided with 50mg, so i went up to 100mg and then 150mg and had a bit of paradox with each increase. I THOUGHT i was ok on 150, so i went up to 200 (split 100 twice a day) for a week, and my POTS went unbearably crazy! Yesterday i took 150mg, and today was still not ok, so i took 100mg, but what should i do moving forward? You keep telling everyone to ‘stick to minimal dose until paradox ceases and then titrate up to symptom relief,’ but i dont understand, because each time i think paradox is over and go up in dose, there is more paradox! Should I go down to 100mg or 150mg and stay there for how long? How do i know when I’m ready to move up, as i thought i was ready for 200mg, but my body was apparently not? Is it normal to have paradox subside and then come back with each increase? How long to stay at what dose? THANK YOU SO SO SO MUCH FOR EVERYTHING!!!!!!
A high B1 is compatible with a mild to moderate deficiency. A high B12 is also compatible with vitamin B 1 deficiency. If you escalate the thiamine dose and get paradox, go back to the previous and test again later. You have had a long time in a state of biochemical decadence and must exercise patience in reversing it.
Reduce the magnesium. It is probably the cause of diarrhea
Thank you so much Dr. Lonsdale!
I’m going to go back to 100 mg until I’m absolutely sure there is no more paradox…
In regards to supplementation: do you advise ignoring bloodwork and just taking a b-complex and also a multivitamin? Should I worry about overdoing certain vitamins in a complex/multi? Absorption issues? Also, as B1 dose increases, should I increase the dosage of complex and multi? Thank you!!
Hi, Can you please tell me if I would get any benefit from Benfotiamine for thiamine replenishment? I realise it doesn’t cross the BBB, but would it still be a good place to start? I’m not ready to take on the paradox effect, as I don’t have good medical support (GP). I’m afraid of the scary side effects.
Thank you
You have to be aware that when you start thiamine in any form and you have been long insufficient, you will get paradox whether you like it or not. Paradox can last as long full as a month or so and it is nothing to do with side effects. It is because you are trying to change from catabolic to anabolic metabolism. Start allthiamine at a low dose and suffer the consequences until paradox gives way to improvement. There is no gain without pain.
Dr. Lonsdale,
When I consume any form of thiamine but thiamin cocarboxylase I get thiamine deficiency symptoms (dizziness, severe adhd). Is it possible that I have a tpk1 problem or an enzyme deficiency that does not convert the thiamine to the active form since I paradoxically feel worse after thiamine even after weeks on it? Have you seen such a thing? It’s almost like a thiamine allergy.
Stick with cocarboxylase. That is OK
Thank you for this article!! And thank you also for the Thiamine book, which I have been finding fascinating, and my health is much improved since B1 supplementation.
Any suggestions on how to avoid Refeeding Syndrome in someone who has been bedridden for several years and is malnourished due to sensory sensitivity and very limited diet? This young woman is 25, suspected ASD. She has lately been suffering phobia of doctors and pills (even vitamins) due to too many ill-prescribed meds by her doctors, and too much mis-diagnosing.
I suspect she has Thiamine deficiency, (and it may be affecting her mental state!) but even a small amount of topical B1 cream makes her feel very unwell. And the same happened when she managed to try a Lipothiamine tablet.
Any suggestions or advice on how I can help her would be greatly appreciated.
You can’t avoid paradox. Just keep up the low dose until paradox (refeeding syndrome) abates and hints of improvement occur. There is “no gain without pain”
Dr. Lonsdale, I am trying to improve long term dysautonomia symptoms, mostly inappropriate sinus tachycardia/POTS, sleep/fatigue and GI issues from too much noradrenaline flooding my body (according to my EP cardiologist) etc… (i’m a very grateful, 43 year old, now migraine-free follower of Dr. Angela Stanton, s/p SVT and PVC cardiac ablations). I initiated Lipothiamine 50 mg 5 weeks ago and had an immediate and sustained increase in POTS symptoms. Last Saturday I thought paradox subsided somewhat, so i upped to 100 mg, and my body has basically felt like I’ve been on overdrive (increased HR, sweating, as if i took multiple cups of caffeine etc.) since.
I understand paradox/refeeding is good news for ultimate success, but want to know:
1. Do paradox symptoms increase EVERY time the dose is raised? Should that be expected?
2. is it safe to just keep increasing dosage without waiting for current dosage paradox symptoms to subside/improve somewhat? would that get to my goal faster? if im suffering through paradox with each increase anyway, can i increase faster to get paradox over with? or is increasing only safe with resolution of each increased dosage’s paradox symptoms?
3. with all the paradox symptoms, how will i know proper final dosage/how high i need to go for my personal needs/long term dysautonomia dysfunction?
Thank you so much for everything!!!!!
The trouble is that the science behind refeeding syndrome is not fully understood. I rather expect that even some holistic doctors give up a vitamin treatment under the false impression of “side effects” as with drugs. The length of RS or “paradox” is extremely variable, but if you increase the vitamin dose before paradox is completed, you can expect paradoxical worsening of symptoms. Please remember that this approach is very new in the modern world and you are virtual “guinea pigs”. However, I am appalled at some of these devastating medical histories. If the symptoms were recognized at onset, the treatment would be easy, fast and cheap. Lasting for months and years and treated as “psychological” makes them expensive and we never know whether there is permanent damage. Try to spread the word.
Thank you so much Dr. Lonsdale! Can you or Chandler explain what would be the symptoms of sensitivity to alpha lipoic acid, vs. regular paradox symptoms? How do I know that my symptoms are paradox and not from the ALA? Im currently at 6.5 weeks of my Lipothiamine paradox. Im now at 100mg for the past 3.5 weeks, with the first 3 weeks at 50mg. I still feel horrible for the first few hours after taking it (sweaty, wired but tired, increased HR/palpitations), POTS symptoms overall are still bad and my sleep maintenance insomnia is worse! Im totally committed to seeing this through, just want to know if this is still paradox, or a possible reaction to something else? I so appreciate any guidance!!! (btw, I can’t take Allithiamine due to the pork)
Hi Dr. Lonsdale, I hope you receive this message!
I’m really uncomfortable and don’t know what to do!
I’m up to 150 mg Allithiamine (switched from Lipothiamine 2.5 weeks ago, as i wasn’t sure if i was reacting to the ALA in the Lipo), and although cardiac paradox symptoms have subsided, my IBS symptoms are much much worse (since starting the Lipo back in August)! My entire life, I’ve been ‘IBS-C’, but symptoms were under control with the Carnivore diet (year and a half) and 800mg magnesium/day (no probiotic, as per Angela). However, since initiating the original 50mg Lipothiamine , diarreah has joined the chorus, alternating diarreah and constipation/bloating/gassy etc. I think my tummy got inflamed when starting the Lipothiamine, and doesn’t now know how to calm down/so irritated? I follow Angela Stanton’s migraine protocol, with Carnivore (dairy and meat) my way of eating and being very careful with my hydration. For the past year or so, I’ve also been supplementing B9, methylcobalamin and D3 (after blood tests demonstrated deficiency). My IBS was stable on Carnivore, with upwards of 8000 mg sodium (for POTS and migraine) daily, the 800 magnesium (i cannot go down on magnesium or will get severely constipated!) and the B9, B12, D3.
I’ve been working so hard (months of paradox) to move up to the megadose of Allithiamine i need for all my dysautonomia issues, but my belly is such a mess i dont know what to do! Please advise!
Thank you so so much in advance!!
That is a huge dose of magnesium and the only effect of an excess of magnesium is diarrhea. Try cutting down the dose
Dr. Lonsdale, I’ve tried cutting down the magnesium dose and then just get constipated! And it’s not just diarreah. It’s alternating constipation/gas/bloat with diarreah and only started with Lipothiamine initiation (only change in diet/supplementation that i can think of…I’ve tried cutting back on magnesium and even the other B vitamins but there is no change.) Can the lipothiamine/allithiamine cause the microbiome to get so altered that even months later, I’m still suffering? Or trigger something to cause other B vitamins to get out of whack? I need to go much higher on the Allithiamine for my dysautonomia, but I’m sort of stuck. Thank you!
IBS is a typical effect from cellular energy deficiency. You need thiamine, magnesium, B complex, vitamins C and E and a multivitamin. IF you are taking sugar or alcohol, stop both
I was also wondering if the worsening ‘IBS’ symptoms could be from the sulfur in both the Lipothiamine and Allithiamine? Im trying to read through comments on other articles, and was wondering if this could be the case? If so, what other form/type of B1 can i take that is equivalent to the Allithiamine as i titrate up? I understand the LIpothiamine and Allithiamine are superior forms, but can i hope for the same relief with other forms? Also Im not sure about ‘splitting dosage evenly,’ as i titrate up? And ‘titrating evenly?’ What does that mean?
I so so appreciate everything!!
Dr. Lonsdale, thank you for your posts on hormonesmatter.com. I have read through many of them along with Dr. Marrs writings. I’ve also ordered and read your book on thiamine deficiency which I found fascinating.
I’ve ended up on this site as a “victim” of metronidazole toxicity. I took it several weeks ago for unexplained gastrointestinal complaints. Since then, I realize my doctor should have never prescribed this and i deeply regret taking it.
Interestingly, i’ve been profoundly unwell since January of 2017. At that time, I was a 25 year old healthy male who worked out frequently and held a full time job. That January, very unusual gastrointestinal symptoms manifested. More specifically, the symptomology consisted of constant bloating, inconsistent bowel patterns, stomach acid issues, and constant throat clearing. Strangely, other symptoms accompanied those that were not GI related. These were POTS, lightheadedness when standing, extreme fatigue, tinnitus, and eventually my palms no longer perspired! All of these symptoms preceded my prescription to Flagyl which was just 2 weeks ago.
I went to many doctors for these symptoms from my primary physician, GI, neurologists, functional health, etc. I even went to the mayo clinic in March of 2018 hoping their gastrointestinal team could find the problem. I had no infection or inflammation in my colon and all blood tests i’ve had show me as perfectly healthy! It’s difficult to convince doctors just how sick i’ve been when all labwork checks out normal.
In the year preceding January of 2017, my daily routine consisted of about 3 cups of coffee in the morning followed by bagels and fast food in the afternoon. Due to always having a lean build and normal blood pressure, I didn’t believe this lifestyle was hurting me. Having consumed the literature that you and Dr. Marrs put together I’m starting to believe my coffee habits and bad diet depleted my thiamine stores long before I took Flagyl.
I’m writing to you today to say that I have begun a high dosage thiamine protocol. I understand you recommend a physician oversee this however I have had bad experiences with physicians the last several years. For the past 8 days I have been taking allithiamine with magnesium. I’m up to 300 mg a day allithiamine and have not seen any side effects. A few days ago I received an intravenous B-complex and had no issues with it. It left me with a slight head pressure, less than a headache. I intend to boost my allthiamine to 600 mg this week and I’m going to pursue this protocol to see if i make improvements. I’m going to take mega doses of allithiamine daily for months to see if i have a paradox reaction or any symptom improvement.
Can I ask you, does my symptomology appear to reflect beriberi?
Do you think that its possible I could reverse these symptoms even though I’ve had them for several years? I’m a 27 year old caucasian male and i know you do not do consults. I’m just curious what your thoughts are in my case.
Unfortunately a highly repetitive story and absolutely typical of an acquired mitochondrial failure. There are many clues but it is fascinating for me to read that the start was a typical example of gastrointestinal beriberi, later to affect the nervous system. Thiamine deficiency means anything less than the full biological requirement. It can be so slight that the symptoms are ignored or misdiagnosed. However, a relatively mild injury or an infection demands an energy dependent adaptive response and can precipitate clinical thiamine deficiency. The ensuing symptomology is usually attributed solely to the injury or infection, whereas it might be a combination of the two. POTS (postural orthostatic tachycardia syndrome) is now known to be an energy deficiency disease and at least some cases have been published as thiamine deficient. Note the diet here that was so innocently ingested. He was quite right: he already had thiamine deficiency when he took Flagyl. It seems that medical ignorance of this common state might even be a threat to our culture and in one of my books, I compared it with chronic lead poisoning that was partly to blame for the collapse of the ancient Roman empire. This sounds like overdrive but lead leached out of the lead glazed jars in which the ruling classes kept their wine. The lead made the wine very sweet and encouraged their bachanalian feasts. Lead poisoning was well known to them but they didn’t know why! Today there is insufficient awareness of how common thiamine deficiency is and don’t forget the magnesium. I think that a high degree of emotional sensitivity can result from their combined deficit, possibly precipitating violence on top of a perceived injustice and possibly providing an explanation for the epidemic of shootings that have decorated American culture for too long. Are we all half asleep?
Thank you for your response Dr. Lonsdale. I want to ask another question. Is gastrointestinal beriberi not recognized as a problem with gastroenterologists?
As I mentioned in my original post, i had gone to the Mayo clinic in 2018. I truly believed at that time that my health would be in good hands but after some tests, the dr threw his hands up and said he couldn’t find anything wrong. vitamin deficiencies were never mentioned when it seems like they would have to consider that as a possibility. How come major institutions aren’t looking into the nutritional status at a cellular level? these things seem like something that GI docs or any docs would consider to be of great importance in disease.
Dr. Lonsdale, I posted the following to the fb group and Dr. Marrs asked me to post it here for you to answer, thank you!:
Dr. Chandler Marrs I just finished reading yours and Dr. Lonsdale’s thiamine book- great piece of work, thank you!
You mention multiple times in the book that those with hypoglycemia did not appear to respond, and even responded negatively, to thiamine supplementation. I have: non medication induced hypoglycemia (after hpv vaccine and a hospital stay that was diagnosed reactivated EBV leading to GBS but I think was possibly an acute B1 and possibly other deficiency), pots (after hpv vaccine), brain fog, leg edema (lower leg especially started around puberty), seborrheic dermatitis, hEDS (started around puberty too) I believe caused by deficiencies. My hypoglycemia has become more periodic since giving birth last year. I tend to have my low lows (90 down to 30s) around ovulation and right before my period. I know B2 is used a lot during these times for tissue remodeling. I also have a hard time fasting, doing keto, carnivore, etc and produce ketones way faster than most seem but I seem to urinate them out vs using them.
I wonder if the negative response is because something else needs to be repleted first? B2 possibly? I have been working on B2, I, Se, Mo, Fe, and B12 repletion and want to start adding B1 but am hesitant.
If you have any thoughts I would greatly appreciate it! Your book definitely brought a lot of insight as to why doctors continue to find “nothing wrong” and everything else I have been going through. I have been recommending it to everyone ?.
Others in the fb group have commented that B3 and biotin may be an issue as well.
This is a very typical story of thiamine deficiency, almost certainly with a genetically determined cause. I would suggest that you have absence of one of the genetically determined protein transporters. The best supplement for you would be Lipothiamine from Ecological Formulas.Start with 50 mg a day together with about 200 mg of magnesium taurate but beware of “paradox/ refeeding syndrome” that is discussed in the post. Lipothiamine will provide the body with thiamine and does not need the transporter. This needs to be done under the care of a knowledgeable physician because paradox can last for as long as a month or so or may not occur at all. This is a new form of treatment and few doctors are aware that your “psychological” symptoms are those of beriberi.
In a person gradually increasing a dose of ttfd would refeeding symptoms reoccur every time the dose is increased?
Maintain a low dose until paradox ceases.
What if you already feel poorly before taking Thiamine? How would you know if you are having a paradox reaction if you simply continue to feel poor after taking the Thiamine?