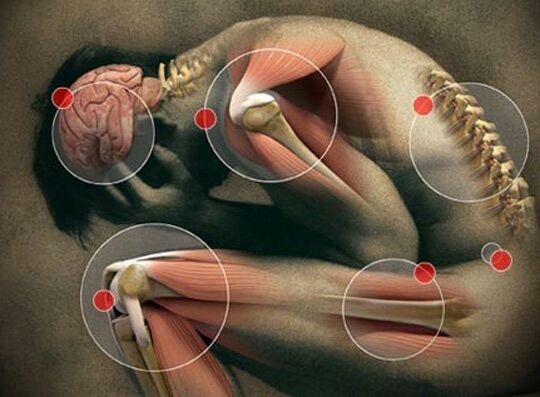
Fibromyalgia affects roughly six million Americans, mostly women. Its symptoms include all-over muscle and tendon pain, increased pain sensitivity, chronic fatigue, sleep disturbances and brain fog. Fibromyalgia is often reported as feeling like a flu that never leaves. Similarly, symptoms of Chronic Fatigue Syndrome (CFS) overlap with many of those of fibromyalgia and the two conditions are often co-morbid. With chronic fatigue, however, the predominant symptom is a fatigue that never lets up versus all-over muscle and tendon pain.
Both fibromyalgia and chronic fatigue are co-diagnosed frequently in women with endometriosis, especially those who have had Lupron treatments. Similarly, we are finding a high incidence of chronic fatigue and fibromyalgia post Gardasil/Cervarix and post fluoroquinolone. All over muscle and tendon pain, coupled with never-ending tiredness seem to be common symptoms post medication or vaccine reaction. Could they be linked to a broader problem, specifically, thiamine deficiency?
What is Thiamine?
Thiamine or vitamin B1 is necessary for cellular energy. It is a required co-factor in several enzymatic processes, including glucose metabolism and interestingly enough, myelin production. We can get thiamine only from diet. When diet suffers, as in the case of chronic alcoholism where most of the research on this topic is focused, when nutritional uptake is impaired (leaky gut and other GI disturbances), or when other factors inhibit the enzymes necessary to carry out intracellular reactions, thiamine deficiency ensues. And thiamine deficiency can elicit a whole host of problems that are consistent with the current definitions of chronic fatigue and fibromyalgia.
Thiamine and Fibromyalgia – A Few Hints
A recent case study suggests that what is currently diagnosed as fibromyalgia and/or chronic fatigue may be attributable to thiamine deficiency. A very small case study (n =3) from Italian physicians found a significant reduction in fibromyalgia symptoms in patients given high dose thiamine. Researchers found:
- Patient 1: 71.3% reduction in fatigue; 80% reduction in pain.
- Patient 2: 37% reduction in fatigue; 50% reduction in pain.
- Patient 3: 60.7% reduction in fatigue; 60% reduction in pain.
Thiamine and Chronic Fatigue
In a little bit larger study – 17 patients with Chronic Fatigue, researchers found a functional reduction of the enzymes involved in vitamin B metabolism (aspartate aminotransferase -pyridoxine, glutathione reductase and transketolase) compared to healthy controls, suggesting thiamine deficiency.
What This Means
It’s way too early to tell if thiamine deficiency is at root of fibromyalgia and/or chronic fatigue symptoms, or if adverse reactions to medications and vaccines can elicit the symptoms of fibromyalgia and chronic fatigue, but there are hints pointing in that direction. Much more research should be done. In the meantime, if you suffer from fibromylagia or chronic fatigue or undiagnosed neuromuscular pain, why not consider testing for thiamine. And while you’re at it, since many of these symptoms overlap with those of hypothyroidism, particularly of the autoimmune Hashimoto’s sort, why not get tested for that too. If you test positive for either of these, tell us about it, it will help other patients find solutions. To learn more about thiamine deficiency and other topics, search our growing library of research and patient stories here on Hormones Matter.
We need your help.
Hormones Matter needs funding now. Our research funding was cut recently and because of our commitment to independent health research and journalism unbiased by commercial interests, we allow minimal advertising on the site. That means all funding must come from you, our readers. Don’t let Hormones Matter die.
Yes, I’d like to support Hormones Matter.
This article was first published on Hormones Matter in October, 2013.













I have been a health researcher and keen observer for decades (hobby not professional). I have turned around many conditions with natural means personally and friends/family.
There is a new kid on the block which completely changes everything we know. EMF.
My personal battle started with local cell tower and digital meter against our will. It not only affected me and family, but affected the animals and plants. I found some remediation that worked and exercised and all was getting better.
A year ago they massively put up additions and full blown fibromyalgia hit. I now have to walk with two canes. We have massively increased remediation on house but it is only a band aid. Two more towers are now within a few miles of us. It is hell.
Rural area, small town. All decided to install huge solar farms outskirts and in town. I tried to warn them, they won’t listen.
Now migraines everywhere. People complaining of pain- same early stages I went through. I have never seen so many people using walkers and canes of all ages. Never.
I was in impeccable health. Pristine diet. Very well supplemented with natural supplements when needed, which was not often. I had tons of energy, no problems walking or running at all, and extremely active. No coffee, no sugar or refined foods. Limited carbs of healthy natural sort. No alcohol. No medical additions of any sort from pills to needles. Fantastic water.
We were all doing beautifully.
The towers seem to create a deficiency in B1, magnesium, etc so the body is either blowing through it or cannot longer absorb it.
Our area around just this tower- suddenly every house has cancer in it, some have lost ability to walk for no apparent reason, neurological diseases hit fast and our immediate neighbor died this past year from neurological disease.
All of these conditions do seem to be connected to some degree with low B1.
We can not move, but even if we did they have put up 100 towers in our part of the state in the last year. This is inescapable. That is not to mention solar farms and wind turbines which also do similar damage.
I just wanted to mention this as it is significant. If this much damage can happen to my family, who lives ultra healthy, it will be even worse for those who don’t.
I an currently doing b1 therapy very slowly and it is extremely difficult with paradoxical reactions. I am doing 1/4 thiamax a day w b vitamins and trying to keep all other things in balance too from potassium to electrolytes etc. If this was just regular life, I would have no issues, or few. The added hell of emf radiation is uncharted territory and it is very difficult to gage my plan of action and what is going on due to this added factor.
Sorry for the following question, if it seems obvious, but I am really interested in understanding:
If a blood test revealed low aspartate aminotransferase (ASAT) (between 0.11 and 0.16 microkat/L at various times, while reference range is 0.25-0.6 microkat/L), would that then indicate a need for B6 or B1 supplementation? I am guessing both, but what is the mechanism for their respective involvement?
The internet is not at all helpful as to the meaning of low ASAT, can only find info regarding high ASAT.
There is no lab that correctly tests for thiamine deficiency anymore, correct?
Not that tests it correctly that we aware of. If you learn of one, please let us know.
So roughly 1 out of 100 Caucasians are heterozygote (Carriers) of Homocystinuria. CBS homocystinuria heterozygotes have an intrinsic deficiency processing B6 (Pyridoxine) which is needed for all the B vitamin enzyme reactions. This makes the heterozygotes more susceptible to overt deficiency symptoms when suffering from malabsorbtion or hypothyroidism.
Do you have a reference/citation for the B6 deficiency?