It started very slowly; at an almost non-existent rate. My mother, then about 84 years old, broke her ankle. She had been extremely active, playing table tennis regularly in a senior club; she was also a bridge champion almost all her life. She even joined online bridge groups and beat everyone on the internet too. When they asked how old she was, her partners and competitors just flipped that she was in her 80s and a bridge champion. She was sharp as a tack!
The ankle that broke needed surgery with plates and screws. She was restricted to bed for 6 months and then to wheelchair for life. While her ankle was healing she was in bed and could not play bridge, she lost her skills and partner. She was also dependent on others and became depressed. I would rather say she was angry with life for what happened to her rather than depressed but she insisted that she was depressed. She paid a visit to a neurologist begging for an antidepressant.
The neurologist prescribed half of the smallest possible dose of Mirtazapine, a simple serotonin that on its own is capable causing major damage but she received a very small dose. As she started taking the medicine, very tiny changes developed in her personality but they were so mild as to almost unnoticeable. In retrospect, we see what happened – hindsight is always 20/20.
First Signs of the Impending Doom
The first sign that she had too much serotonin in her brain was that rather than feeling calmer and happier she became more agitated; she was unhappy with people around her, criticized everything, nothing was good enough. Then bowel incontinence started and she had trouble holding her stool until she reached the bathroom; her bowel incontinence further limited where she dared going so she felt angrier. She became very easy to irritate and was pissed at the whole world.
What I have just described took four years to evolve so we did not see the connection of all these changes to the serotonin medicine. Then one day as I was refilling her medicine, the drugstore ran out of Mirtazapine and they placed her on an SSRI called Zoloft instead—the doctor changed her prescription.
An SSRI (Selective Serotonin Reuptake Inhibitor) is a very different medicine from the old small dose serotonin my mother received. While Mirtazapine merely provided a small extra dose of serotonin to the brain, Zoloft forced her brain to make serotonin 24/7.
How SSRIs Work in the Brain
To understand what SSRIs do, envision a sink with an overflow hole on the top, in case you left the water running. This will allow the extra water to flow back into the drain and if you have an automated sink that is connected to this backflow, the sink would know it is full and would turn the faucet off. This little overflow hole in the brain cell is called reuptake. It does exactly what the overflow does. If it senses that enough serotonin was made, it shuts down serotonin manufacturing of the cell until it senses that more is needed. However, SSRIs inhibit the reuptake receptor, i.e. plug it up. Just as your sink will flood your house with water if the overflow is plugged up, so does the brain fill up with serotonin as long as the reuptake is inhibited. This makes the brain cell manufacture serotonin forever, regardless how much is needed and how much it already has made. 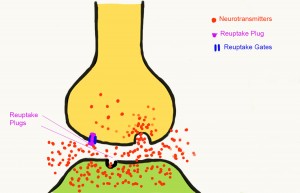
Only a small percentage of serotonin is made in the brain, less than 10%, and 90% is in other parts of the body. The intestinal tract uses most of the serotonin to pass the food through the intestines with proper speed—this explains why having too much serotonin in one’s body causes bowel incontinence. Serotonin also functions as part of memory and cognition, and it is also a vasoconstrictor. Serotonin is a dangerous substance that predisposes the patient to diabetes 2. Thus it is no surprise, in retrospect, that we saw changes slowly from Mirtazapine but very fast changes as my mother was moved to take an SSRI. Suddenly changes took place at a drastic pace:
- Day one of the change to SSRI was a confusion day. She was clearly agitated, confused, and bowel incontinence became a permanent feature
- Day two she was angry staring up at the ceiling all day in bed, refused to eat or do anything. The commode had to be moved into the bedroom though she barely made it that far without accident.
- Day 3 she fought the whole world, nothing was right. She set in a corner totally agitated
- Day 4 she called me on her cell phone at 5 am (we lived in the same house, with me right above her) asking when breakfast was served in this house. I rushed down and found her sitting at the edge of her bed in total confusion. I put her back in bed and told her breakfast will be served at 9 am so she should go back to sleep.
- Day 5 is when the moment of recognition hit me. She called me again on the cell phone at 5 am. I ran downstairs. She was seated at the edge of her bed, totally naked with her bathrobe barely on. Her entire closet was on the floor; she pulled everything off every single hanger and shelf. I ran up to get the blood pressure meter. Her blood pressure was so high the cuff gave me error twice before I was finally able to read her blood pressure. The systolic was over 180 (120 is ideal), I don’t remember the diastolic but it was over 100. I called the ambulance and off she went to the hospital.
In the hospital, I tried to tell every doctor what her history was with the SSRI. I am a medically trained professional in neuroscience and though not a medical doctor but a researcher, I can identify a serotonin syndrome when I see one as long as I know the history that led up to it.
For my biggest surprise, and why I am writing this article, is that physicians rarely recognize serotonin syndrome. No one believed me when I told them that I suspected that my mother was suffering from serotonin syndrome. No one listened to me when I asked that they test for serotonin syndrome. I received comments like this from a psychiatrist: “Your mother cannot have serotonin syndrome, it is too rare.” Serotonin syndrome is not rare but the doctors who identify it are, and he was one of the many who did not recognize serotonin syndrome when he saw it. Another doctor told me that “she may have serotonin syndrome but we cannot test for that and cannot treat for it.” In fact, testing and treatment are both available for serotonin syndrome. The problem is with the doctors who do not ask any questions and only make assumptions based on the patient’s age (she was 88 at this time) using profiling assume that anyone over the age of 80 must have dementia. They diagnosed my mother with Alzheimer’s type dementia (something we were able to see via autopsy to have been the wrong diagnosis). She was misdiagnosed and mistreated with the wrong medicines until she died. There was nothing I could do. I suspect that for those of you who are not scientists like I am, the task is even more daunting. So prepare for the fight of a lifetime.
Unfortunately, the symptoms of many illnesses or conditions resemble that of the symptoms of serotonin syndrome. The surest way of knowing if you or your loved one has serotonin syndrome, is if serotonin medicines have been taken for a long time and symptoms slowly worsened over time or if new serotonin medicine was just introduced. If three of the following symptoms appear, take the patient to the nearest hospital via ambulance immediately, stand guard and get ready for a fight to save a life!
- Agitation or restlessness
- Confusion
- Rapid heart rate and high blood pressure
- Dilated pupils
- Loss of muscle coordination or twitching muscles
- Muscle rigidity
- Heavy sweating
- Diarrhea
- Headache
- Shivering
- Goose bumps
- High fever
- Seizures
- Irregular heartbeat
- Unconsciousness
The importance of this long introduction is that today more people take SSRIs than ever before hence the increased odds of ending up with serotonin syndrome, and that serotonin syndrome is misdiagnosed. More people take multiple types of SSRIs or mix SSRIs and other medicines with serotonin, such as triptans that are so often prescribed for migraineurs. Serotonin syndrome is fatal if it is not attended to very quickly. Unfortunately, it was indeed fatal for my mother. I run a large migraine group and one of the first things each member has to do is answer a few questions via private messaging. One of the questions is about the list of medications they take. I go through every single medicine and provide a full analysis and if I find they are at risk of serotonin syndrome they are given all information to talk to their doctors. A very large percent of the new migraineurs joining take two or more serotonin medicines at once. Checking for possible serotonin syndrome is essential.
Additional information to help you to select a good hospital for your care: Medicare has created a program aiming to reduce mismanagement of patient care. They provide a score to each hospital based on the number of mismanaged cases, which includes hospital induced delirium as well as other cases. Hospital induced delirium is the new name for serotonin syndrome in many hospitals and you may find it listed as the official cause of death. Medicare assigns a score to each type of condition and sums up the incidences of misdiagnosis and mismanagement per hospital. Those hospitals that rank over the 75 percentile receive a reduction of payment from Medicare until they improve the care.
I wish that doctors were just as well trained in recognizing serotonin syndrome as they are trained to write prescriptions for serotonin. Since doctors are so unaware on how to recognize serotonin syndrome and because the consequence of that oversight is fatal, it is best to consider your options carefully before accepting serotonin prescriptions. Serotonin medicines are prescribed for everything, but when we look at what they actually help is very minimal.
To get serotonin without medicines, eat those foods that put you to sleep after lunch: turkey has lots of serotonin. Head out to the sun. Sun releases serotonin. If you live in a cold region where sun is rare in the winter, invest in a home sun-lamp. The light it releases initiates serotonin release in your body. Enjoy a pleasant walk; go shopping; watch children play in a park; go to social gatherings. Anywhere full of happy friends or people in general will supply you with feel-good hormones that will help ease any depression. There are many treatments on their way for depression and one of them is the same treatment as for migraine and anxiety. Join my migraine group to learn more.
This article was published originally on Hormones Matter on November 30, 2015.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.













Hey Angela – Do you know about possible reasons behind lasting symptoms following acute occurrences of serotonin syndrome?
Most papers on serotonin syndrome-resulting damage seem to either fall into covering immediate harm in acute instances – usually from the associated hyperthermia, or ongoing symptoms from what looks like more mild cases of an ongoing serotonin syndrome.
I’m 19, & around two months ago I experienced what I think was a moderate-severe case over a few days-1/2weeks most probably due to a combination of phenelzine(irreversible MAOI) + another medication that unknowingly stimulated serotonin release + a few medications with related effects, but to a much lesser extent.
Even many weeks after discontinuation of the MAOI + any serotonergic agents -My immediate working memory and word recollection has worsened to the point of becoming really functionally difficult – and has continued mostly without change in the ~6 weeks since.
Do you know if 5-HT efflux alone is capable of causing damage at a synapse/axonal level such as with a case of SS, or would any damage most likely just be another aspect caused by the associated hyperthermia?
The only two ways I’ve managed to imagine having a chance of diagnosing anything at all would be PET scans for density loss at a receptor level, and EEG/related imagining for communication deficits between regions from a structural viewpoint.
Do you know if there are any easier ways to try and find some form of answer/help, and what potential there is to hope to make a real recovery – I can’t imagine living out a full life with problems that have persisted so far
Thank you!
Hi Daniel,
Unfortunately phenelzine (brand name Nardil) is a really nasty medication. The state of “irreversible” MAOI means that the enzymes must be replenished by your body–and this assumes your brain has the ability to replenish them. This can take 2-3 weeks in a person who has no difficulty replenishing MAOI but you didn’t say what other medications you are taking and perhaps those medications also interfere with the replenishing of these enzymes. MAOI deficiency has similar symptoms to serotonin syndrome: flushing, sweating, headache, diarrhea, sleep disorders, etc.
I have a question: what way do you eat?
The reason why I am asking this is because we now know that depression is really not a serotonin issue. It is a glucose metabolism issue with the mitochondria in the brain. There are some studies but also millions of people with depression, bipolar, schizophrenia, and a host or other brain disorders, including degenerative ones, such as Alzheimer’s, Parkinson’s, MS, ALS, and many more, all respond amazingly well to the very low carbohydrate ketogenic diet and some to a very strict carnivore diet.
Have you tried the dietary approach yet? If you want to achieve a life-long recovery, feeding your brain what it needs will help. The human brain is 85% cholesterol and saturated and omega 3 fat (EPA and DHA). The brain makes its own cholesterol. About 80% of brain energy can come from ketones. Ketones are medium chain fatty acids in the brain (small chain are in the gut). For the brain, think of ketones as rocket fuel and glucose as diesel… you get the picture.
Best wishes,
Angela
I’m someone who’s been reading about health, hoping to find ways to relieve my symptoms of chronic fatigue, weakness, muscle stiffness, headaches, etc. When I was ages 18-30, I had chronic depression, and was prescribed a series of medications that affect serotonin level. Later, I developed what’s been diagnosed as chronic fatigue syndrome, and have been sick with its symptoms to this day (I’m 66). I now take just one medication: gabapentin.
I wonder if you’re aware that depression can be caused by high serotonin, as well as low. Because each neurotransmitter has an optimal range, good health requires the avoidance of too little or too much of any one of the neurotransmitters. Also, did you know that tryptophan must cross the blood-brain barrier before serotonin can be produced? Did you know that what makes this happen is a rise in insulin that occurs when carbohydrates are consumed? A diet composed strictly of animal foods would lower serotonin. Yes, lower it. But that might be just what’s called for, if the depression is caused by high serotonin. Also, a low carb diet would lower the levels of various vitamins and minerals. A lessened amount of these nutrients would tend to lower the level of serotonin, because many of these nutrients help make serotonin.
In other words, the reason why your diet helps treat depression may be because the problem all along wasn’t low serotonin, but high serotonin. If you do a little more research, you may see what I mean.
I’ve only just recently found online these facts about serotonin, and haven’t yet applied them. However, I’ve come to think that my problems are caused by high serotonin, and that I may even have a very mild case of serotonin syndrome. From now on, I intend to consume more animal foods, and fewer carbohydrates. Aside from providing the benefit of keeping insulin from rising very much, animal foods contain tyrosine. It’s important to get enough tyrosine, because it’s needed to make dopamine, which helps balance the serotonin.
Dear Katheryn,
Thank you for your long comment with lots of information. Let me address each point you make.
1) Depression can be caused by too much serotonin and not just too low serotonin:
Although depression is often treated by serotonin medications, to date there is no proof that depression is connected to changes of serotonin levels at all. See “The serotonin theory of depression: a systematic umbrella review of the evidence” foor a strong review of the literature. In modern medicine, the treatment is often based on little or no evidence at all based on trial and error. In fact, there is research pointing to deep brain stimulation (that is electrical stimulation of certain brain regions) that achieve far greater results with true clinical depression.
2) High serotonin levels — this is called “serotonin syndrome” or serotonin toxicity and it is independent of depression.
3) While the presence of glucose is essential to the proper working of serotonin, the consumption of glucose in the form of carbohydrates is completely unnecessary. And that is because our liver continuously produces glucose from foods we eat and fats we store via gluconeogenesis. Have you not wondered why our body stores fat instead of glucose if our body must have glucose? The answers is that triglycerides are a “knotted tied product” of 3 fatty acid molecules with a glycerol cap. Two glycerol caps, that is 2 triglyceride molecules, create a glucose molecule and 3 non-esterified free fatty acids under gluconeogenesis by our liver. As you can see, we get glucose made in our liver so we don’t need to eat it.
It is also better if we let our liver make exactly as much glucose as is needed for body functions and we humans don;t override these metabolic processes. Because overriding them and eating what we “think” we need to eat as opposed to what we actually need to eat can mean the difference in brain health vs sickness.
4) The increase in insulin upon consuming carbohydrates is not helping serotonin increase or reduction in the brain at all. Over 90% of the serotonin is made and used by our intestines, The food “passing through” is guided by a wavelike action of our intestines and that is driven by serotonin in our gut. The more serotonin you have in the gut, the faster and potentially the larger your elimination. It is not connected to serotonin release in the brain.
5) Insulin has a completely different role in the brain from the body. In our body sugar consumption spikes insulin becuase high levels of blood glucose are toxic and insulin must quickly remove the excess glucose. In the brain insulin has no glucose-associated roles at all. In the brain insulin helps in the creation and enforcement neuronal connections, thereby helping memory. Insulin also arranges the trimming of unhealthy or unused connections, and it is also responsible for providing the signal of satiety to the brain. Insulin resistance in the brain doesn’t cause diabetes in the brain like it does in the body. In the brain it causes neurodegeneration, such as Alzheimer’s, ALS, Parkinson’s, MS, and a host of other diseases, which are quite preventable.
6) The consumption of more animal foods and the reduction/elimination of carbohydrates are very helpful in all neurological diseases because it removes the need for the mitochondria to burn glucose–a highly thermal substance that creates lots of oxidative stress by the pyruvate conversion process, and moves to burning small to medium chain fatty acids (ketones) in the brain, which is a high energy, high oxygen, low oxidative stress fuel, making the brain work better, more efficient, and no degeneration. I strongly applaud your decision of moving to reduced carbohydrate eating.
Best wishes to you and happy healing,
Angela
I think that you’re missing something very important.
You’re correct when you say in part 4 of your reply that “over 90% of the serotonin is made and used by our intestines.” But you also say in part 4: “The increase in insulin upon consuming carbohydrates is not helping serotonin increase or reduction in the brain at all.” That’s definitely not true.
Serotonin that’s made outside the brain can’t cross the blood-brain barrier. Brain serotonin is produced **within the brain from tryptophan.** Tryptophan can only cross the blood-brain barrier when a rise in insulin forces other competing amino acids into the tissues. Here are a few quotations to back up my statement…
“In order to properly synthesize serotonin, you need sufficient levels of carbohydrates. Tryptophan is only 1% of the amino acids in a standard protein diet and generally takes a backseat to other amino acids in terms of priority… Carbohydrates are responsible for helping drive tryptophan across the blood-brain barrier. As insulin levels increase after carb consumption, cells soak up amino acids without tryptophan.This is because tryptophan binds to albumin, which allows it to remain unaffected by insulin. This increases the chances of tryptophan making its way across the blood-brain barrier and having an effect on the brain’s neurotransmitter levels.” ( https://blog.healthbank.io/protein-for-alertness-carbs-for-sleepiness/#:~:text=In%20order%20to%20properly%20synthesize,across%20the%20blood%2Dbrain%20barrier )
“The consumption of a carbohydrate-rich, protein-poor meal or snack can increase the synthesis of the brain neurotransmitter serotonin; **proteins block this effect.** The mechanism of the rise in brain serotonin involves the secretion of insulin…” ( https://pubmed.ncbi.nlm.nih.gov/2903717/ )
“And only carbohydrate consumption naturally stimulates production of [brain] serotonin.” ( https://news.mit.edu/2004/carbs )
Katheryn,
Thank you for your comment. Let me answer each of your comments.
1) Serotonin made outside of the brain can’t cross the BBB: I wonder what the pharmaceutical companies have to say about this, given the many antidepressants prescribed to people with depression. So yes, serotonin can cross the blood brain barrier even if it is made outside of the brain. Another proof for serotonin’s ability to cross the brain is serotonin syndrome—a topic I cover in this article.
2) The processing of tryptophan into serotonin does require carbohydrates, but we need not eat them. Of the 20 amino acids we eat, 18 are glucogenic, meaning they convert to glucose either in the process of aiding growth functions with insulin, such as protein synthesis, or if too little protein was consumed to start protein synthesis, or if extra remained after maximum protein synthesis is over, these amino acids convert to glucose to support body functions.
3) The human body is quite capable of absolutely healthy living without eating a drop of carbohydrates since in addition to the high glucose levels created by protein consumption, one of the liver’s most important tasks is to create glucose, a process called gluconeogenesis. In this process the liver takes stored fat, which is in triglycerides form, meaning 3 molecules of fatty acids connected with a glycerol cap, and removes the glycerol cap and from that creates glycogen, which is the mammalian starch form of glucose. The brain can use the following fuels: ketones, glucose, lactate, and glycogen, where ketones are short or medium chain triglycerides.
4) The last point you made “And only carbohydrate consumption naturally stimulates production of [brain] serotonin” is completely incorrect. The proof that this is incorrect comes from millions of people who have quit eating carbohydrates completely and moved to the carnivore diet. Prime example is the Lion’s Diet by Mikhaila Peterson, including her family—Jordan Peterson with his long battle of various psychological issues all healed, and her mother Tammy Peterson who was told she had terminal cancer and 10 months to live by all of the big name medical institutions, 5 years ago.
In summary, I appreciate that you do your research and try to explain certain functions of your body! Great stuff doing your research. However, there is so much misinformation out there, that unless you really are familiar with the whole field from top to bottom and all people involved in research and why they say what they say, it is very hard to understand things around you.
We now know that all diseases that are not birth defects, genetic conditions (like sickle cell), accidents, or infectious diseases are caused by nutrition. The excess consumption of carbohydrates, specifically the refined and/or processed carbohydrates, seed/veg oils, grains, and the overconsumption of high antinutrient-containing plants lead to all of these diseases. And this includes depression. It’s not the lack of serotonin—we also know by now that serotonin doesn’t actually help depression. Lots of discussions on this by now.
One can have 100% mental health absent some conditions I listed by simply eating the proper human diet, which is mostly carnivorous, with some fruits (not fruit juices) and veggies in season, fresh or cooked but not bought already processed. Nowhere in the history of humanity has there ever been a society living on as high levels of carbohydrates like humans are today!
Best wishes,
Angela
Can you elaborate on what specific tests will test for serotonin syndrome?
Thank you 🙂
Dan,
There are no specific tests for serotonin syndrome because 90% of the serotonin in our body is actually used by our gut and not the brain. So any blood test for serotonin would just measure what our “below the head” part of the body uses and wouldn’t reflect what is happening in the brain. Serotonin syndrome is evaluated by the symptoms I listed in my article. There are some “indirect” tests via blood that potentially can help. You find these listed here.
Best,
Angela
I recently finished TMS. I have been on Vyvanse and Zoloft, and started having panic attacks. My doctor upped my Zoloft and added Buspar generic. I had hives, trouble breathing, diarrhea, intense fatigue, sweating and severe headache and chest pains. So the doctor has taken me off of Zoloft but wants me to continue Vyvanse and Buspar. I have Major Depressive Disorder and ADHD. How is it possible to use diet to recover from all of this without medications? What foods help remedy or improve these conditions? I’m so tired of being tired and so sick of being sick.
Dear Tiffany,
I am very sorry to read about your deteriorating health conditions. Yes, nutrition can reverse most depression and panic-attack type disorders, and ADHD is very specifically caused by lack of sufficient brain nutrients. The most ideal nutrients for humans are animal products. As the plant-based diet is pushed on people in various countries in Europe, it is fascinating to see an increase in ADHD in children, in complete parallel. The best food for brain health is an all animal (carnivore) diet.
Best wishes,
Angela
Angela,
I had posted another comment about how I think SSRI’s are harmful. I did not know about SSRI syndrome but it makes sense. My brother has been taking SSRI’s and has developed a condition that the doctors say has to do with ALS. He now constantly falls and hurts himself and has trouble with his speech and his nerves. I mentioned to him to look into side effects of his medication but he did not think it was possible. I can’t say the falling and reduced functioning is directly related. I was wondering if you ever looked into SSRI’s causing damage to or interfering with your nerves and body at a cellular level. Would it be possible for it to cause ALS?
Dear Marie,
Let me respond to your shorter comment first: yes, SSRIs can cause ALS. There are articles on that, here is one. ALS is a mitochondrial dysfunction disease. Mitochondrial dysfunction is not well understood by the scientific community, but it is very well understood that our modern dietary lifestyle leads to mitochondrial dysfunction. Even type 2 diabetes, a highly modern disease caused by too much processed foods full of sugar and seed oils, is considered to be a mitochondrial dysfunction condition: “Type 2 diabetes is associated with both impaired insulin action at target tissues and impaired insulin release. Defects at both levels are evident early in the course of the disorder, and evidence suggests that mitochondria play a role in both processes.” (see here.)
Why this is so requires a very long and complicated response, so I am not going to attempt it, but it would benefit your brother to try to read some of the diseases associated with our modern diet: all diseases that are not infectious, genetic diseases, or accidents are nutritional and are in some way connected to mitochondrial dysfunction. As is ALS.
In terms of how SSRI may play a role in this: SSRIs block off a vital neuronal function, the “reuptake” protein, which would tell the neuron to stop and rest, there is enough serotonin already in the synapse.
What SSRIs do is destroy this communication, and the neurons are forced to produce serotonin 24/7 day and night, whether there is enough serotonin or not. This causes mitochondrial damage because there is not enough nutrients for the mitochondria to produce energy nonstop like this–without mitochondrial energy, there is no serotonin created. And so the mitochondria are literally overworked and damaged/killed off.
Mind you, there are millions of people who had clinical depression, clinical bipolar, and a host of other mental conditions that all have improved or were cured by a change of diet, often a 100%% animal-based diet.
And this makes sense: our brain is 85% fat and cholesterol. Of the fat, 35% of it is DHA (from fish or pasture raised eggs, dairy), and the rest are saturated fats. in other words: there is nothing in plants that supports human brain.
And plants have a lot of antinutrients that block nutrients from plants, and animal protein and nutrient absorption as well if the animal products are consumed with plants.
Unfortunately this is not an open access article, but you can read from the abstract that an all animal-based diet can provide all the vitamins and nutrients a human needs, including vitamin C.
In summary: there is a highly likely case that no one on this planet needs to take an antidepressant under any condition, meaning the clinical presentation of depression is usually caused by nutrient deficiencies. Therefore it is preventable and at best it is reversible without medicines. But it takes dedication and strength to give up carbohydrates, which are extremely addictive, please read my most recent article here.
I hope my answer helps you and your brother,
Angela
This response is severely misleading. The article you cited to back up your claim that SSRIs can cause ALS does not conclude that at all. In fact, the author stated, “There is currently no strong evidence to link any medication use with ALS risk”. The article found that there were some studies that found a link between antidepressants and a higher RISK of ALS, but in no way shape or form should this be considered causation. It is some evidence that there is a correlation.
Secondly, SSRIs work by inhibiting the reuptake of serotonin. For anyone who doesn’t know, what this means is that the SSRI blocks the transporter proteins that take serotonin away (usually back to the neuron that it came from). There are many reasons why a neurotransmitter (like serotonin) may not work as it should. For example, the brain could be producing too much or too little, the neurotransmitter could be reabsorbed too quickly. The monoamine deficiency theory posits that depression is caused by the brain having depletions in neurotransmitters like serotonin, norepinephrine, and dopamine. SO, all of that is to say that the SSRI’s job is to block serotonin from being reabsorbed, or taken away. This means that there is more serotonin available for the brain to use. Since a theory is that depression = too little serotonin, an SSRI is a solution for that. Serotonin syndrome is caused by having too much serotonin. Certainly, taking too many SSRI pills can cause this. But so can taking St. John’s Wart, antiemetics (anti-nausea), L-Tryptophan (not naturally occurring, found in poultry and dairy, etc.), L-Dopa (Parkinson’s med). Point is, many things can cause serotonin syndrome, but it is most commonly caused by combining medications that contain serotonin like migraine meds and antidepressants.
Dear Marissa,
Thanks for explaining what SSRI is and what it does with as a reuptake inhibitor, you just repeated what I wrote in the original article. The neuron uses the reuptake to judge how much serotonin it needs to make based on what’s in the synapse, which is information the reuptake is supposed to transmit. Since the reuptake is plugged up (inhibited), it is unable to relay any message and the neuron doesn’t know that there is plenty of serotonin in the synapse. This forces the neuron to make serotonin 24/7. This is what I explained, to which you wrote it is misleading. It’s not at all misleading. I explained the same thing you did.
Edit: you are responding to a response. I couldn’t see that.
Association is not causation but a strong risk association. There are many articles on the connection of antidepressants and increased risk for ALS. Since there are no other drugs associated with strong risk of ALS other than antidepressants, while not “causal” but the connection is explained in this paragraph:
Neither my article nor my response earlier is misleading.
Cheers,
Angela
This is very insightful and I’m glad you wrote about this. I’m concerned about what is happening in the medical community as well as how mental illness or feeling agitated or just not yourself will warrant a visit to a psychologist. They will then prescribe an SSRI without even really knowing a person or doing any tests, yes they ask you questions and yes they spend time with you but they never really know you, they only know what you tell them. They can only go on what the person tells them. I was told I was depressed by my family who are not medical professionals and should not be casually diagnosing others. I was then convinced that I was mentally ill even though I wasn’t eating properly or sleeping well and I had problems with my blood sugar which affected my energy levels. What I was dealing with and feeling was temporary, I had just lost a loved one and had to grieve. During times like this sometimes people don’t eat or sleep well and Had i been taking better care of myself I would not have felt tired and cranky and this would have passed. With time I would start eating and sleeping better and would return to myself. Instead I was given a false diagnosis because I walked in to a Dr’s office and said I have depression.
Here’s what happened: I was put on a very strong SSRI by a nurse practitioner and given a generic version. These medications are very, very strong even at low doses and I believe other methods should be implemented before resorting to this route. I don’t believe SSRI’s help people, they block a part of your brain and you sometimes are unable to access your emotions. What happened to me was my doctor increased my dose. I told him I was not comfortable with the meds and did not agree with him but he was the professional and he convinced me the dose should be increased (we’ll tweak it and see if that works, trial and error approach) and I became almost catatonic, the meds went from like 25mg or 50 mg to triple digits, I began suffering from headaches and the medication did not agree with me and as I mentioned earlier I was not mentally ill and did not need medication. I wound up meeting my fiancee at this time and fell in love. This is key here because it was almost as if I could only watch myself from afar and not access how I truly felt although I sensed that I was supposed to feel more. I had not been on this medication all my life so I knew the difference between being numb and actually feeling things. So now it had blocked my emotions and I was not able to deal with them even though I was trying to sort them out. I realized that I wanted to feel my emotions and needed to. Feeling numb was not normal and I did not have a severe problem. I really think these meds should be reserved for people who can not function and are very, very ill. Not for every-day people. I’m now hearing little 15 year olds and 18 year old girls say: “I was feeling “anxious” and something is wrong with me so I got on medication” When you are this age your body is going through hormonal shifts and you will feel anxious because of that but that does not mean you should be put on an SSRI. These medications also have very strong side effects and that should not be taken lightly. If you are put on an SSRI with an anxiety med like xanax, now your ability to function will change again. You will be lethargic at work and sleepy and if you drink it can cause you to become incredibly confused to the point where you could not know where you are. This happened to me at a work event and I could not get home. The best thing that happened to me was my fiancee said “stop taking the meds” you don’t need them. He was right I did not need them. I stopped taking them but had to deal with anger issues afterwards and feeling horribly irritable. My personality changed and I had muscle spasms and shaking. I then went through intense withdrawal and just stopped taking all medications, anything that affected my hormones (like birth control) or my ability to think I stopped taking. I went through an intense withdrawal process and stayed home until it passed. Right before this my body became so depleted that I got shingles so I was already forced to rest. After stopping the meds I am now healthy and fine today and there is absolutely nothing wrong with me. In life we go through different seasons and circumstances we are not shown or taught how to deal with our emotions or what they are for. We will need to use our emotions and our brains to deal with these things. Anger tells us that we might be afraid and if you channel it into something positive it can motivate you towards a goal, depression and feeling low tells us that we are not coping well and could be due to constant stress and that needs to be changed, you need relief and to take care of yourself or to get support. Harsh upbringings and circumstances will cause changes in the brain. This should be addressed. I don’t believe we should just label people with depression, or adhd, or npd, or whatnot. Take a look at their circumstances, help them cope instead of giving them a pill and saying see you next week.
Some of these reactions and “conditions” are the brain’s way of protecting us. If we are anxious, we should pay attention to our needs. Taking pills does not solve anything and can actually cause more harm. We need to remain in touch with these things so we can take care of ourselves as they are cues to what is going on in a situation. If you lose touch, you won’t be able to react properly, people will treat you differently as well and you won’t be in touch with what is going on around you and your reaction time will slow down. Many people don’t realize this. Then there’s stimulants they sometimes prescribe and that will cause rage attacks and high blood pressure. These meds are being give out like candy, all you have to do is ask for it.
I just want to add that people don’t always live in healthy ways, they don’t have healthy lifestyles. If you are going out drinking heavily every night, then waking up not eating, drinking only 4-5 cups of coffee and eating at 3pm only, and then doing this again the next night, you are going to feel “depressed” your brain is not getting any nutrients, your body can’t cope with this. People will never tell their doctor this and they’ll say oh i’m so depressed give me medication. Until you start being healthy your life and feelings won’t change. I mean drinking heavily causes vitamin deficiencies and I can go on and on. I’m just saying all of this needs a different perspective and mental health is not one size fits all.
Dear Marie,
I couldn’t agree with you more! Unfortunately the whole medical system is set up to treat symptoms rather than help people heal. Medications, such as SSRIs or any other antidepressants, treat symptoms, but not the underlying cause. And symptoms are very important for us to see and feel because they tell us that something is not right. The goal of the symptom is to help us find the cause. Remove the symptoms, and there is no chance to find the cause.
It is also important to mention that many people think medicines are important and essential part of life. I received an email from one of the readers of my articles and this person wrote in response to my suggestion of changing her diet:
(typos are in the original.)
As you can see, not everyone has the kind of mindset and understanding of the world around them as you do. Most people want the easy way out and to just pop a pill, even if they know it’s not helping them. It is easy and convenient, and it lets them live the way they always lived, which caused the problem the first place.
I must say, that why I disagree with doctors prescribing pills for everything, I understand why they are doing it. In my article here I described the death of my mother but originally, when she got her first antidepressant, which was just a simple one and not SSRI, she begged the doctor to give her one!! The doctor, I think, understood that what she had was a temporary depression as a result of her broken ankle and not a clinical depression, but she didn’t give her doctor a chance! She most certainly wasn’t listening to what I said. She wanted an easy solution that then ended up taking her life.
I admire your courage of standing up for your health, quitting all medications, and understanding that what you had were symptoms of a major loss in your life, after which depression is quite normal. You understood it with delay, but you understood it, and now you can live your life healthy as a result. I wish other people could reach this level of understanding and give their body a chance to heal itself!
Lots of hugs to you,
Angela
Most of these stories have the same fix. Old people need aggressive physical therapy as soon as possible (a couple days after surgery). A therapist will sit them up in bed, move them to a chair, stuff like that. They lose muscle mass really quickly and probably won’t get it back. Then they get bed sores and infections. Muscles are used to regulate body temperature and are metabolically active. They also develop blood clots that can cause a stroke, if they don’t occasionally move.
Watch your supplements and tell your doctor everything you’re taking. Unless you understand the biochemistry of each ingredient in all the supplements, take a regular daily vitamin at the most.
Why do you say these medications contain serotonin? It doesn’t cross the blood brain barrier and isn’t how serotonin is made in the body. 5HTP does cross the blood brain barrier and is past the rate limiting step. It turns into 100% serotonin. It’s safe on its own because the body degrades serotonin incredibly quickly.
Dear K,
I think you have not read the blog article at all. Serotonin medication do cross the blood brain barrier–I never wrote anywhere that they don’t. Not sure what you are reading. The whole article is about how serotonin increased in the brain out of control as a result of the serotonin medication. So not sure if you read my article at all.
Also, my mother, of whom this article is about, had no surgery. And none of the medical symptoms and elderly weakness you mention are relevant in my article. not sure what you mean.
As for where serotonin is made and used in the body: 10% is made and used in the brain and 90% is made and used by the intestines. And no, it is not safe to take serotonin is=n any amount. If it were safe, there would ne no serotonin syndrome, now would there be! Clearly your information is incorrect.
Best wishes,
Angela
Isn’t Mirtazapine a 5ht 2A and 2c inverse agonist? Correct me if I’m wrong, but wouldn’t that mean that Mirtazapine is an anti serotonin medication as far as mechanism of action?
It hits those two receptors but in the opposite way of serotonin.
Thanks for clarifying!
Hi Dan
“It has been shown that both noradrenergic and serotonergic activity increase following mirtazapine administration. The results of these studies demonstrate mirtazapine exerts antagonist activity at presynaptic α2-adrenergic inhibitory autoreceptors and heteroreceptors in the central nervous system. This is thought to lead to enhanced noradrenergic and serotonergic activity Label, which are known to improve the symptoms of depression and form the basis of antidepressant therapy.
Mirtazapine is a strong antagonist of serotonin 5-HT2 and 5-HT3 receptors. It has not been found to bind significantly to the serotonin 5-HT1A and 5-HT1B receptors Label but indirectly increases 5-HT1A transmission.
In addition to the above effects, mirtazapine is a peripheral α1-adrenergic antagonist. This action may explain episodes of orthostatic hypotension that have been reported after mirtazapine use. Label Mirtazapine is a potent histamine (H1) receptor antagonist, which may contribute to its powerful sedating effects. The pain-relieving effects of mirtazapine may be explained by its effects on opioid receptors.” from here.
Sometimes “hitting” the opposing side can lead to a bigger effect. This is the secret behind the various benzodiazepines and how they differ in what they do and to what levels as well.
Best wishes,
Angela
My husband was diagnosed of Parkinsons disease 2 years ago, when he was 59. He had a stooped posture, tremors, right arm does not move and also a pulsating feeling in his body. He was placed on Senemet for 8 months and then Siferol was introduced and replaced the Senemet, during this time span he was also diagnosed with dementia. He started having hallucinations, lost touch with reality. Suspecting it was the medication I took him off the Siferol (with the doctor’s knowledge) him on PD natural herbal formula we ordered from TREE OF LIFE HEALTH CLINIC, his symptoms totally declined over a 3 weeks use of the TREE OF LIFE HEALTH Parkinson’s disease natural herbal formula. He is now almost 61 and doing very well, the disease is totally reversed! (w w w. treeoflifeherbalclinic .com)
Hi Mary, can you leave the name of the formula you tried? That web site is 404. I have a colleague in his 60s at work who is showing signs of all of this, he is an older single man who doesn’t have an advocate, and I am certain he is not getting the kind of advice which reversed illness in your husband (well done you!).
Thank you so much for writing this. My condolences, I’m so very sorry for what happened to your mother. It’s wonderful that you can, however, use your experiences to help others, I thought I was alone in this and it turns out there are a lot of stories like mine. Thank you, again.
Dear Amy,
I am very sorry to hear that you also got hurt. I wish you a speedy recovery!
Angela
I’m going through this right now. Every time I go to the er they just get my heart rate down and marvel at how rare this is then send me home. My primary took me off all meds that cause it except wellbutrin. Some days are kinda ok. Most days are intolerable with my high heart rate, chest pain, light and sound sensitivity, migraines and twitching. I’m miserable.
Dear Anna,
I am very sorry to hear. You know, the migraine part is completely preventable. I focus on migraines and have tens of thousands of people who have learned how to become migraine and medicine free. Please join my Facebook group here and also read my book here.
Best wishes,
Angela
Dr. Stanton,
I hope you can help me. I read about your Mother and the Serotonin Syndrome. It sounds exactly like what happened to my husband. I have a Wrongful Death claim against the hospital. I was told I have no chance to win because I need an expert witness Pharmacologist.
I am 81 years old. My husband was 84 years old. When my husband died my income was cut right in half. It costs thousands of dollars to have a Pharmacologist look over his medical records and write a report. I need a report by a licensed medical expert. In June 2019 my husband exhibited the exact same behavior he did in March 1998, confusion, agitation, did not recognize me or our daughter, sweating, so hot he ripped off his gown, ripped out whatever was attached to him, trying to escape out of his bed, trying to escape out of the hospital, and kicking his legs like he was running a race, flailing his arms.
Patients don’t have their regular doctor, who knows their medical history, check on them in the hospital. A Hospitalist checks on them. He may see them once, twice and then never again. The Hospitalist told me my husband had Delirium. He explained to me that old men have Delirium when they are in a hospital setting.
My husband was born with Gerstmann’s Syndrome, damage to the frontal parietal temporal lobes, his right side of his body was slightly underdeveloped and his right hand didn’t function. He was very intelligent. In 1970 he had an industrial accident and suffered for 50 years with severe back pain. Ten years ago he developed kyphoscoliosis. His 6′ 2″ frame was now 4″5″. His right rib cage rested on his right hip bone. But he was still productive, though he moved slower, and as you said about your Mother, he was sharp as a tack.
He was knocked down by the dogs and fractured his hip. He was fine after the operation. He was given oxycodone APAP 10-325, which is what he took at home for his back. The hospital had given him Morphine Sol. Inj. Then they decided to give him Dilaudid IV, not knowing he had adverse reactions to Dilaudid. He became nauseous, So they gave him Zofran. Our daughter told the nurse her Father could not have Dilaudid. They gave him more Dilaudid the next day. He told the nurse he didn’t want the Dilaudid, he asked for Percocet.
In March 1998 he had a bleeding ulcer from his pain medication. They gave him Demerol and Ativan.
I tried to explain to the Hospitalist that because of his brain damage his brain and body couldn’t process many medications that were prescribed for him. That he can’t take medications like most people can. That he can not have any antidepressants, antipsychotics or psychotropic medications. The Hospitalist just looked at me and said “Brain Damage? What about the brain damage?” He did not know about the March 1998 event and didn’t seem interested. He insisted he had Delirium.
My husband had pain medication every 4 ½ to 5 ½ hours for 50 years for severe back pain. The Hospitalist prescribed Seroquel for him. My husband did not have a pain pill for over 10 hours. He yelled in pain. A different doctor gave him half of the regular dose of oxycodone. He was dead in 2 hours.
What can I do? I have to have something in writing to hand into the Arbitrator by the first week of January 2021. I have to proof that the hospital breached the standard of care. They claim they did not.
Sincerely, Patricia Hanson
Dear Patricia,
I am very sorry to see what happened to your husband. Unfortunately I cannot be of help because I don’t know what to do. I am not an attorney and I clearly have failed in my attempt at trying to prove wrong-doing in the case of my mother. I am not in the position to advise you since whatever I did was not sufficient. The only thing I recommend is that you consult with an attorney and I hope you find a good one, who will handle your case.
Best wishes!
Angela
Jesus, talk about depressing. Just because you think you failed your mother, does NOT mean that you automatically fail everyone else. I hope you have gotten to feeling better in the past 2 years. That comment was sad to read.
Devin, I didn’t fail my mother. I had no opportunity to fail my mother. Her doctors, healthcare professionals like you, with PhD or MD in psychiatry (you have a PhD in psychology, so similar) are the ones who failed my mother. I am not an MD and could not have possibly prescribe medications for her. And I was not the one who forced her to take them–in hospital, often typing her to the bed to give her medications!
I didn’t fail her but your system did. Just don’t push this on the patient… push the responsibility to those who should have known better and should have recognized the serotonin syndrome.
Would you have recognized her serotonin syndrome?
Cheers,
Angela
Hello Angela,
I am hoping you can help me. I have been suffering from mild depression for years. It runs on both sides of my family. My mother has severe anxiety and mild to moderate depression and refuses to take any antidepressant or anxiolytic meds. Her condition has caused many, many issues over the years.
This year my anxiety and depression are getting worse. I fear I am following in my mother’s genetic footsteps.
Due to some additional symptoms such as forgetfulness (possibly associated with stress and depression) and the fact that I bawled my eyes out in her office when she asked if I was dealing with any stress, my MD thought it might be a good idea to try Lexapro. We ran a number of labs to make sure everything was ok and they all came back normal.
I have fought the idea of taking an antidepressant for years (I’ve tried supplements, SAMe, etc.) but am finally starting to cave in and am seriously considering trying something in hopes that it will help. Due to this, I have been doing research on Lexapro (that is how I found your article) and have found a few disturbing articles on long term effects of Lexapro, one entitled, My Brain after Long Term Lexapro: Chemically Induced TBI (from this website). I’ve always been fearful of taking antidepressants due to info like this. I am not sure what to do. Is there a safer antidepressant or should I just keep trying to deal with this on my own?
On a side note I used to take Vyvanse and have been off it for approximately eight months and was debating getting back on it. My MD said that taking both would be fine.
Dear Willow,
I am so sorry to read what you are going through but am very glad you found this website, read my article, and also doing your research on your own. What you are doing is half the battle! <3 Here is my take on this, which is my opinion, my personal experience, my experience with those who took medicines for depression and anxiety, and also some research I have done both in literature as well as nutrition. None of what I write here is medical advice, so don’t use it as such.
My personal experience first: I was diagnosed with general anxiety disorder (GAD) when I was 19 years old. I was placed on Valium (diazepam in generic). It helped and luckily some competent doctors decided to check on my vitamins and discovered that I was almost zero in B12. So, in addition to Valium, I was also placed on B12 IV. I recovered very well, but since I was only 19 and was a rather clueless 19-year old, I have not paid much attention, I had no understanding and didn’t desire an understanding at that time. I was on and off Valium and they put me on all kinds of other drugs, but, of course, nothing was working. Valium did, so I am still on Valium (now age 67), though I am now massively tapering and nearly off. I expect to be completely off in 2021. It’s a very slow taper after so many years.
You may ask why and how I am tapering: I discovered the nutritional route cause of my anxiety when I started to experiment with nutrition to resolve my migraines! Little did I know that resolving my migraines I will also resolve my anxiety!! But I did! So, my personal experience is concluded in the finding that anxiety is a nutritional (metabolic) problem. I never had depression though, so that required more digging. So here let me connect to my experience to people who took medication for anxiety and/or depression: it doesn’t work. So far all the people I have ever met with clinical depression (meaning reason is not specific to any particular cause, such as the death of a loved one, etc.,) or bipolar or anxiety responded amazingly to nutrition as well. I will explain the connection in a moment. However, I would like you to search out Mikhaila Peterson, whose entire life has been one giant depression from birth and is now completely depression free simply using nutrition.
My literature search on depression came to the findings that clinical depression may be helped by some of these medicines for a very short time and only a very small percent of the people respond. And that’s because the cause of depression is not understood and while most drugs provide serotonin either by adding it into the brain or by forcing the brain to make it 24/7, as Lexapro does, it is unclear if serotonin is the thing or the only thing that would be needed. There is no strong evidence to suggest that any of these drugs provide long-term solution, but there is very strong evidence that all of these drugs are harmful and degenerate the brain.
Back to my experience now with some people who have claimed to have depression, but also had migraines, so they came into my care because of their migraines. The changes they made to prevent their migraines, inevitably always lead to the elimination of their depression and anxiety as well. So here is what I do with people who come to me for help–and again, I am not a medical doctor. And I don’t treat anyone but suggest solutions that I have experience with.
The first thing I do is request a blood test from their doctor. However, I am the one analyzing this blood test, not their doctor, and I request very special test!! Most doctors find many of the things on the test request and “overreach” but in time they realize that what I asked for was essential. So you need to get a test–the test is in my group and you are welcome to join my group for help. My analysis of the test is different from the analysis of regular doctors because my ranges differ greatly from the standard.
I also have all the Facebook group member change their diet to be mostly or completely animal-based. And the reason for this is many-fold, but one of the most important elements is that all of the neurotransmitters our brain needs to make require animal proteins. We need to consume all amino acids (plants don’t have all, except for soy, but it is a goitrogen and destroys the thyroid, so we don’t eat soy) and animal products have the correct amino acids and the correct ratios to one another such that tryptophan, a most common animal amino acid, can convert to serotonin in the brain. Plant enzymes and anti-nutrients block most animal product nutrition, so basically I place most members in the carnivore diet. It is a huge change. However, everyone recovers.
I also have everyone increase salt consumption. Salt is essential for the brain to fire its electricity properly. There have been some experiments on deep brain stimulation (with electricity) for those with depression, and it worked. Well then, depression, in at least some cases, is a voltage problem. And what helps to generate voltage? Salt. There you have it. It is really quite simple. All people in my group come off of all their medications and all are pain, anxiety, and depression free, full of energy, become metabolically healthy as well. We also supplement some minerals and vitamins, based on what I see on the blood test.
If you wish to try a completely natural way of healing, I recommend you join my team and try it out. It is very healthy nd can only help you. And if you find it doesn’t work, you can always start the medication. However, I know it works. 🙂 It workd for me as over 10k people so far. So join us!
Angela
Have you tried genetic testing to see what medications mesh well with your DNA. I had it done for my son and myself we both suffer from depression, I was tired of the doctors telling us try this medication and now this one!! It was the best thing we ever did. We also found out our bodies needed a type of folic acid that is a mood stabilizer that helped our depression immediately!
who do you get dna testing from?
Before I start I just wanna say that I’m only 25 years old, I was 22 when this happened. To make a very long story just a little bit shorter, the reasons I was on the medications that I will talk about in my story are because when I was 21 I was diagnosed with stage 2a cervical cancer. The radiation basically melted my colon and bladder and just made a colossal mess in my lower stomach and groin area, so I’d been on lots of medications for pain, ptsd, depression and more. Anyways so I was in the hospital one of my many stays in those few years, and I was on methadone which was my main pain medication, and I was on celexa which was my antidepressant. I’d had a doctor put me on mirtazapine to help me sleep while I was a local hospital close to home a couple months prior(my main doctors and hospital was 3 hours away since I had cancer). Anyways I’d been at the hospital a couple days and my sister was staying with me. She kept noticing that I was agitated and couldn’t remember anything whatsoever. I was twitchy and luckily I had a colostomy bag because my bowels were constantly just going nuts. So one morning I wake up and I keep trying to talk but I just stutter. I woke my sister panicking and crying which only made the stutter worse, trying to ask her what was wrong with me. So I calmed down enough to stutter out what I was trying to say. My sister called the nurse, which was basically a friend because I stayed there so often they all became like family to me. She was going over my medicines from the night before trying to figure out why I had the stutter because everything else we had just assumed was a normal part of me being sick, I mean I had cancer which comes along with a zillion side effects. So anyways she gets to the mirtazapine and she says who the hell prescribed you this? And I told her that when I’d been sent to the ER at home they prescribed it to me to help me sleep. She. Was. So. Livid. So she calls the doctor in there and shows him what she found and they are talking and the doctors finally tells me that they shouldn’t have ever given me that medication with me being on celexa and methadone. They didn’t use the name Seratonin syndrome, but that’s exactly what it was. It’s just so crazy to me that a doctor who had seen me before and knew what meds I was on, prescribed me this medication and obviously didn’t know, or care one, how dangerous it was. And my nurse was the one who caught it. I’m just thankful I was in a good place with smart doctors, and especially smart nurses. You talked in your article about how they just basically dismissed what was wrong because she was an elderly woman and they didn’t even care to try and see if it could be something else. When I got sick, right before I found out that I had radiation necrosis, I had a doctor tell me multiple times that i just had a bug and I’d be fine in a few days. He said that severe radiation damage didn’t happen to otherwise healthy 22 year old girls. But before I was diagnosed with cancer and my pap came back as abnormal I was also told them that 21 year old girls just didn’t get cervical cancer because I didn’t meet the criteria. It’s amazing how many doctors we have in this world that are so ignorant.
Dear Hannah,
I am so sorry about what you have been going through. Thank you for sharing your story And, indeed, I said the same thing you said at the end: “21 year old girls just didn’t get cervical cancer because I didn’t meet the criteria“. It is very sad that some (many) doctors have such narrow view of their patients. I no longer expect that my doctors remember anything about me. I can see how difficult it is. I now have about 8,000 migraine sufferers in my two Facebook migraine groups and I am starting to have a hard time remembering who is who… yet I talk to many every day, and most of them at least once a month… still, it is very hard to remember.
So, please keep vigilant and keep on reminding your doctors what meds you are taking, what you had bad experience with, where you stand with your cancer–even 20 years from now when even you barely remember… it must be added to the list for every doctor visit. It is very fortunate that one of the nurses knew you so well and it is an even bigger luck (and hugs to that nurse) that she knew which drug was trouble and why! rare nurse and rare friend! And hugs to your friend for staying with you in the hospital–also very rare!
Best wishes to you,
Angela
Oh my goodness my poor mom. This is what happened to her! Oh how awful, it brought back the worst meteorites. She passed away almost two years ago. Hospital induced delirium! Explosive diarrhea which made her faint in the toilet over and over while we held her. Confusion, anger, falls, Very high blood pressure. Omg.
Dear Lydia,
I am very sorry to hear about your mom! And now your daughter too is getting on a serotonin drugs. I think she should look into alternate options. I don’t know why she started Zoloft, and there may be a reasonable explanation for some rare cases, but my personal take is that drugs like this are the absolute last resort, when all other options have been extinguished.
Best wishes,
Angela
First off, thank you for publishing this article. Since trying to wean off of Effexor 9 years ago (and failing miserably) I’ve been acutely aware of the seriousness of withdrawal and other effects of taking Effexor XR.
I do have a question for Dr. Angela, if I may, regarding Serotin Syndrome and Triptans for migraines. I will provide a short background to help explain myself:
I have been on Effexor XR continuously for the past 14 years (for depression/anxiety). I tried to wean down over the course of 7 weeks in 2009 to prepare for pregnancy, but the withdrawal was so terrible, I stopped 7 weeks into the weaning process when the symptoms were too much to bear. (I went on to have two healthy babies (one of which is 10 now) and so the Effexor did not seem to have any detrimental fetal effects, thankfully.)
Upon weaning my daughter from the breast in 2016, (approx. 24 months after her birth) I developed what turned out to be chronic intractable migraine that I’ve had ever since. My neurologist was glad to see I was on Effexor as it could possibly help, he said, and then had me adjust my birth control with the help of my Gynecologist to something that keeps my hormones from fluctuating as much (Lo Loestrin FE), and we tried Triptans (sumatriptan and rizatriptan were tried) to help quell the migraine. With the Triptans, I immediately began feeling like I was entering some type of horrible drug interaction with my Effexor XR. I felt horrible: nauseated, SEVERELY agitated, sweaty, clammy, and a strange feeling in my head that felt almost like my head was swelling or something. I could not stand to be in my own body, it was so uncomfortable. I did a little bit of internet research and came up with information serotonin syndrome when discussing effexor and triptans. I called my pharmacist and he said that his resources said that while a possibility, it was not likely but to stop the triptan if I was having so much trouble. I spoke then to my doctor and he refuted the idea of serotinin syndrome being an issue and that I would be much sicker. I tried to mention that I stopped the triptan usage as soon as I felt awful after speaking with the pharmacist but he was seemingly uninterested in discussing serotinin syndrome (or even some other type of interaction that wasn’t serotinin syndrome but still a contraindication between the two drugs.) I am still suffering from migraines today and am now seeing a new neurologist in another state and when I mentioned that my Effexor did not interact well with Triptans he said that he was also unaware of this and that there should not be an issue.
I suppose I am looking to see if this is indeed and issue, whether related to serotinin syndrome or another type of contraindication between the two drugs. I understand the dismissive tendencies of physicians but I also understand that sometimes the information has not been gathered, tested, or published yet and so just because one doctor refutes something does not necessarily make it false.
I currently receive botox for migraines and it mitigates the symtoms well for the most part. I take Fioricet when the migraines break through.
Any thoughts on interaction between triptans and Effexor (or other SSRIs) would be appreciated!
Dear Jill,
The first thing I did was pop Effexor and a most typical triptan (sumatriptan) into the drug interaction checker to see what that tells me. You can do the same by typing “drugchecker” into your search bar (as one word, so no spaces), and click on the option that takes you to the one at http://www.drugs.com. This is the only way to find it as far as I know. The following is what popped up:
I highlighted the important part in bold. So it can create serotonin syndrome. You may want to show both your doctors and your pharmacist how simple it is to find out if drugs interact!! I am unsure why no one is every considering to look at the official source!
I am glad you have stopped triptans, and please continue to not take those. While Botox may initially help, so far, on the long term, it hurt every migraineur I know. One of the most important problem with Botox is that it weakens those neck muscles that then later–after Botox no longer works and you stop–cause cervigogenic headaches, which then lead to migraines.
Let me say this loud and clear: Migraines are 100% preventable without a drop of medicines!
To learn how to prevent migraines requires a lifestyle change. I find that many migraineurs literally reach suicidal state before they are willing to give up their beloved carbs, and so by the time they make the change, it is double or triply as hard. I have worked with close to 10,000 migraineurs by now over the past 6-7 years and all I can say is that those who start early, and are willing to do the lifestyle changes, are 100% migraine free within weeks and those who start later, after many years of migraines, medicines, and bad eating habits, can take 2+ years of recovery before they become migraine and medicine free.
The sooner you start, the better. I recommend you join my Facebook migraine group here, but if you prefer not to, at least read my book to guide you.
I am looking forward to seeing you in the group,
Angela
Jill, and Angela,
I too was given Efexor, even after expressing my concerns to my gynecologist , who wanted to prescribe for anxiety. I had taken Zoloft once for depression years ago and had a horrible reaction, muscle rigidity vomiting etc.. so come to find it later they’re related!!!. So to make a long story short, I decided to give it a try, took it at 9 p.m. as directed to take before bed, woke at 1 a.m. to a huge flash of lightening inside my head, broke out in a profuse cold sweat,then became ice cold, started vomiting, diarrhea and then i looked and my pupils were dilated. I rushed to the ER and the doc told me it was not seratonin syndrome because he expected me to be worse. Dismissed me sent me home without performing any blood work, testing or even asking me what meds I was on, besides this. I was so frickn pissed. I had lethargy and a general feeling of illness for a week thereafter. I tried to go after the hospital. Pointless. No attorney would take my case . I’d say look for whatever herbal remedies and healthy nutrition, limit stress, spend time in nature, no news watching, heavy metal detox, eat organic and raw as much as possible, try yoga, and deep breathing is vital to our health. Best wishes!
Dear Heidi,
I totally agree. I am so sorry that you were so ignored and mistreated. Yes, going to the hospital with a complaint is absolutely pointless. It is best to not get on any of these medications and indeed: proper nutrition, yoga, medication, proper vitamins and minerals–I don’t recommend herbal supplements because they are medicines only we don’t know much about them, so one can get into serious trouble with them as well. We now know that a lot of people with anxiety and depression are simply sensitive to modern carbohydrate-laden nutrition and can’t get enough vitamins from them for their brain. I recommend a diet very heavy in meat–especially red meat–which is very rich in amino acids that are the precursors of neurotransmitters, such as Tryptophan is for serotonin. Egg yolks are full of choline, a main neurotransmitter. Nutrition heals. The problem is the misinformation about nutrition even more than about medicine. We are forced to eat plant-based and plant release very little if any nutrients for us. We must eat meat.
Best wishes,
Angela
Angela,
Thank you for sharing such an extremely painful and torturing experience with the public just to help others. Bless you. Your mom is very proud of you. Bless her and her angel wings.
Thank you for your pain enveloped in generosity and selflessness.
What do you think of Cymbalta?
Dear Kat,
Thanks for your lovely comments on my mom! <3
Unfortunately I have a very bad opinion on Cymbalta. It is an SNRI, which is a serotonin–norepinephrine reuptake inhibitor (read about it here) and here is the important part:
I bolded a few important parts: “thought to be“… this means that drugs like this are used as guessing… “monoamine hypothesis of depression, which asserts“… “Norepinephrine may be related to“…
I don’t know about you but I just highlighted 3 hypotheses based on which these drugs were created and prescribed, and no one is actually sure if they work at all. And from experience of those I talk to who take these, they don’t work. On Facebook, based on the search “Cymbalta” in groups I found 28 groups, all helping people quit, one with 25,000 members (Cymbalta Hurts Worse)
From my experience with helping people who are reducing Cymbalta, I can tell you that it is probably the worst drug ever to try to stop, because it affects so many functions that drive the brain. If I were you, I would stay far from this drug. Knowing what I know from those with depression and anxiety, these drugs don’t really work–if they do then only for a short time–and have huge side effects. I have not yet met anyone who would not have been able to start an improved lifestyle in stead of taking this drug–or other drugs in this class. And that’s because all health conditions that lead to people taking a drug like this are caused by lifestyle–usually diet–that can be change.
I strongly recommend you consider that.
Best wishes,
Angela
I’m curious if the risk for serotonin syndrome is lower if the doses for the combining medications are also low? I’m 30 years old and my doctor just prescribed me 10 mg prozac every third day for the two weeks leading up to my period (for pretty severe depression from pmdd). My concern is i’m already on 10 mg of vyvanse and 2 mg of subutex (embarrassing) a day. It seems the depression is from the drop in serotonin leading up to my period but I know that still doesn’t exclude serotonin syndrome from happening. Basically I really want to start the Prozac because of how the pmdd really affects my life half a month every month but I’m not sure if the vyvanse should be stopped first. Thank you for the help!
Dear Elizabeth,
Reduced dose of anything will cause less damage but it still causes damage. I would recommend you search the internet for depression and diet connections. There are thousands (if not millions) of people posting their successful reversal of their depression–and a host of other brain and psychological conditions–by simply changing their diet. Particularly, the carnivore diet–eating only animal products–seem to eliminate all depression for all who tried it and posted about it. It appears that while it can be hormone-driven on appearance, in reality it is nutritionally driven because hormones are managed by our nutrition.
So rather than a medicinal solution, I would suggest you look into a nutritional solution.
Best wishes,
Angela
After taking zoloft for 20 years, I fell into major depression. They changed me to viibryd, titrated to 40 mg. daily. I have extremely fatty stools with explosive diarrhea. I’m also experiencing a lot of anger. I feel mad and short tempered. My fear is taking nothing leads to suicidal thoughts. I am a big red meat eater( daily). Could it just be that I need a dosage decrease?
Dear Lori,
It may be. You may have passed a tolerance threshold but it may be additive over the years. It may also be the wrong medicine for you. There are many potential problems when taking a prescription medicine, no matter what type. If you are taking this medicine for depression, you may want to look on the internet where people are reversing their depression by dietary means. If it is migraine, you may want to join us in my Facebook migraine group.
Best wishes,
Angela
Hi, I don’t know if you would know but is it safe for me to take Zoloft, Vyvanse, trazodone, and propranolol together? Those are the medications that my psychiatrist prescribed me to take.
Dear Madilyn,
Glad you reached out. No, these drugs are not safe to take together. Here is the result of “drugchecker”; I only copied the major interaction and also the therapeutic duplication. Thre are more interaction but those were moderate. To find out your drug interactions, always google “drugchecker” (as one word) and the link that is the correct one will take you to the drug checker of https://www.drugs.com/. I try to link you here to my findings but I am not sure you can see them: https://www.drugs.com/interactions-check.php?drug_list=2057-1348,1475-2533,2228-0,1956-0 It may need a new search… not sure how that works. But you know how to find it and then enter each drug name, options will pop up so select the one you have and then click “check for interactions”… I use this all the time.
Interactions between your drugs
Major
traZODone sertraline
Applies to: trazodone, Zoloft (sertraline)
Using traZODone together with sertraline can increase the risk of a rare but serious condition called the serotonin syndrome, which may include symptoms such as confusion, hallucination, seizure, extreme changes in blood pressure, increased heart rate, fever, excessive sweating, shivering or shaking, blurred vision, muscle spasm or stiffness, tremor, incoordination, stomach cramp, nausea, vomiting, and diarrhea. Severe cases may result in coma and even death. You should seek immediate medical attention if you experience these symptoms while taking the medications. Talk to your doctor if you have any questions or concerns. Your doctor may already be aware of the risks, but has determined that this is the best course of treatment for you and has taken appropriate precautions and is monitoring you closely for any potential complications. It is important to tell your doctor about all other medications you use, including vitamins and herbs. Do not stop using any medications without first talking to your doctor.
Major
sertraline lisdexamfetamine
Applies to: Zoloft (sertraline), Vyvanse (lisdexamfetamine)
Talk to your doctor before using sertraline together with lisdexamfetamine. Sertraline may increase the effects of lisdexamfetamine, and side effects such as jitteriness, nervousness, anxiety, restlessness, and racing thoughts have been reported. Combining these medications can also increase the risk of a rare but serious condition called the serotonin syndrome, which may include symptoms such as confusion, hallucination, seizure, extreme changes in blood pressure, increased heart rate, fever, excessive sweating, shivering or shaking, blurred vision, muscle spasm or stiffness, tremor, incoordination, stomach cramp, nausea, vomiting, and diarrhea. Severe cases may result in coma and even death. You should contact your doctor immediately if you experience these symptoms while taking the medications. It is important to tell your doctor about all other medications you use, including vitamins and herbs. Do not stop using any medications without first talking to your doctor.
Therapeutic duplication warnings
Therapeutic duplication is the use of more than one medicine from the same drug category or therapeutic class to treat the same condition. This can be intentional in cases where drugs with similar actions are used together for demonstrated therapeutic benefit. It can also be unintentional in cases where a patient has been treated by more than one doctor, or had prescriptions filled at more than one pharmacy, and can have potentially adverse consequences.
Duplication
Antidepressants
Therapeutic duplication
The recommended maximum number of medicines in the ‘antidepressants’ category to be taken concurrently is usually one. Your list includes two medicines belonging to the ‘antidepressants’ category:
Zoloft (sertraline)
trazodone
You may want to show this to your doctor and ask him to use this very tool in the future. This may avoid serious complications!
Best,
Angela
Thank you so much for responding! I’m 17 years old and have very little control over what my doctor prescribes me. I informed my mother of the risks and she said, “he knows what he’s doing”. I don’t know how to get her to listen to me about this, she sits with me during my sessions with the psychiatrist. Do you have any advice for possible medicine swaps that I could suggest to both my doctor and my mother? I’ll give you a little background info in case you need it. I’ve been taking the Zoloft (for panic disorder/general anxiety/depression) and Vyvanse (for ADHD) for a while, I just recently started the trazodone (for depression/insomnia) and the propranolol (for panic attacks) is only taken as needed. Thank you again, I understand if you can’t help me 🙂
Dear Madilyn,
I am very sorry that you are a minor and cannot yet decide what you do and seem powerless in helping your mom see that doctors make mistakes. Have you shown her the website itself? It is via drugs.com, which is a better source than any doctor. Perhaps that will help her see. She may also want to read my article about my mother–this article we are commenting on–so she can see that doctors are no gods at all. I cannot recommend any alternatives since they all do the same and in a similar way. The best is no drugs at all, but that requires a lifestyle change, something you may or may not be able to do while you are dependent on your parents.
There are very many research papers, those are out of your and your mom’s reach, but there are also many people who have been discussing their successes with depression, anxiety, and a host of other health conditions, by simply changing their diet, and all of these you can find on the internet. I am not sure how free you are to choose what you eat, but a diet that is exclusively animal-based (all kinds of meat, fish, poultry, eggs, dairy, seafood, organs, animal fats) void of all sweeteners, grains and plants, seems to solve depression and anxiety for many people. In addition, there are many vitamins and minerals you likely lack–perhaps you have B12 methylation problems as well, and that causes severe anxiety!
When I was 19, I had a nervous breakdown with extreme panic and anxiety to the point that I could not do anything. I had no depression, just incredible anxiety coming out of the blue–I remember taking hot and cold showers trying to get rid of it. I didn’t understand it. I also lost a lot of weight. They checked and I almost had no B12 in my blood at all. The doctors placed me on intravenous B12 several times a week for, I think, 3 months. This helped me to recover to some degree, but it wasn’t until I changed my lifestyle by excluding all sweeteners, all grains, all vegetables, all starches, and most fruits and nuts/seeds and started to supplement the fat-soluble thiamine (B1 as Allithiamine) that my anxiety completely vanished! It took me a long time to get to this point (I am almost 67 years old now) but there was no one to guide me. You do and you may be able to convince your mother to give this a try.
Best wishes,
Angela
I am currently taking 2.5 mg Lexapro. I am on a slow taper. Can i take allithiamine with it? if no, why?
Dear Amit,
I checked the drug interaction at Drugs.com and it found no interaction between thiamine and Lexapro. You may get a paradoxical response to Lipothiamine–as most of us do from all types of the TTFD version of thiamine–but that means you need to continue, only reduce the dose. There are lots of articles on HormonesMatter on thiamine, so please spend some time reading them.
Best wishes,
Angela
Hi Angela,
I came across this article while researching Serotonin Syndrome and have requested to join your Facebook page. I’ve been taking 150mg of Effexor XR for 10+ years. In the Fall of 2019, I started having high blood pressure. I went to a cardiologist who told me to stop taking the Effexor. My psychiatrist agreed and we planned to change antidepressants in the Summer of 2020 (I teach and figured it would be the best not to do this during the school year). Here we are in the Summer of 2020 and dealing with Covid-19. My psychiatrist decreased the Effexor XR to 75mg for two weeks and added 10mg of Prozac. After two weeks, he decreased the Effexor XR to 37.5mg and increased the Prozac to 20mg. The gastrointestinal issues came on like a vengeance. My GP did blood and stool tests. My platelets and liver enzymes came back high, but she assumed the liver enzymes were high due to the amount of diarrhea I’d been having. The stool samples were negative to every parasite. She did put me on Flagyl due to how active my intestines were. Week 2 of intestinal issues calmed down due to the antibiotic, but picked back up on week 3. My fever spiked the first week to 102.4. I was tested for Covid twice, both came back negative. The Covid-world makes it so difficult to know what’s going on, and few doctors are seeing in-person patients.
Fast forward to now. My psychiatrist told me to stop taking the Prozac and started me on 10mg of Paxil. The dose increased to 20mg two days ago, and I’m having the same intestinal issues, as well as chills, feeling so sluggish, having headaches/migraines (I was prescribed Zomig for my migraines), unable to sleep much and just feeling like junk. My blood pressure has been all over the place throughout this process (low and high). I’m beyond frustrated, at this point, and unsure of what to do next. This has not been a fun process at all, as I don’t want to leave the house for long periods of time due to the stomach issues.
Where should I turn? I’m in Houston, Texas and the Covid cases are spiking rapidly, but I’ve got to figure out how to get healthy and happy again.
Dear Courtney,
What was the reason for your taking Effexor? Was it for migraine or depression? I can see that Prozac was for migraines, so I am assuming all these drugs were prescribed for migraine? Since you have joined our migraine group, you will see that the trick to prevention is a dietary change and that will also calm your GI issues. However, things take time and these drugs cause severe dependence, so you need to tolerate the withdrawal it seems, since you are having SS–at least so it appears. You should talk to your doctor to review the guidelines for what to do–I believe I give the information in the article. One of the things you will need to be able to get the withdrawal over is diazepam or clonazepam (the FDA recommendation is diazepam (Valium) in a small dose) just to get you over the hump of withdrawals.
In the group you will learn the importance of avoiding some carbs, all vegetable/seed oils, all sweeteners, all processed fruits, juices, smoothies, etc., and how important it is to eat whole foods of fresh meats, animal products in general, high-fiber veggies with zero or low starch, and hydrate optimally, and increase salt. Once you are on the right diet, your brain will have the chance to relax and recover. 🙂
See you in the group,
Angela
I’ve had serotonin syndrome 7 times in my life from different meds. I’ve become more and more prone to it. Now my 16 yr daughter appears to be prone to it. I have several rare neurodegenerative conditions that require medication and after years of going to specialists, researching, and trying everything to alleviate my severe intractable pain, they are without options and hope for me mainly because of the serotonin reactions. My daughter has inherited my genetic conditions. I have also had chronic migraine for 17 yrs. Do you know any facility or doctor or researcher who would know enough about serotonin syndrome to talk with me and help me figure out options? I’m not asking for treatment, just answers. I have tried the keto diet but unfortunately because of bile duct damage I cannot do it. Please let me know if you know of anyone who would speak with me about this. Thank you.
Dear Aimes,
I am very sorry to hear about your health conditions that require drugs and your reaction to them by getting serotonin syndrome. I would like to provide you with two types of answers here and see if you find these helpful.
1) Doctors who know enough about serotonin to learn from
2) Medications you–and now your daughter–needs that cause SS
1) To be honest, I have not yet found any doctor who knew much about serotonin syndrome. I don;t take any medicines with serotonin and so I had no reason to look for a doctor past my experience with my mom. At that time I looked very VERY hard to find a doctor but found none. I found many doctors who can prescribe serotonin or SSRI and most (not all) can even explain how they work in the brain, but i found none who knew about SS other than that it exists.I am sorry that I am not very helpful with this question.
2) The need for serotonin medications: I don’t believe there are any (true) health conditions in which one needs to take serotonin medications. Serotonin is essential for mood regulation, social behavior, appetite and digestion, sleep, memory, sexual desire and function, so it is a very important product our body produces. However, 90% of the serotonin is actually made by our gut. Serotonin is what helps our gut move in a wavelike motion, which then propels the food forward in the digestive process. So we know it is important.
We can naturally increase serotonin by understanding what our body makes serotonin from. Serotonin is made from tryptophan, an amino acid, which is rich in animal products. We need 250-450 mg tryptophan a day from our diet (as per the RDA) to make enough serotonin for health. If you search online for foods riches in tryptophan, you will get a list of mixed goods, which actually aren’t even rich in tryptophan, but they list those because it is inconceivable that they suggest you eat red meat because of the belief (incorrectly) that red meat is harmful. Here is an academic article that’s free to read and lists a descent amount of foods rich in tryptophan–and you can see that red meat is left out but, in fact, red meat is higher than anything listed there.
The fact is that red meat is actually very healthy and has the most tryptophan–by weight–and it is also all bioavailable. If you consume plants for tryptophan, plant amino acids are only 65% bioavailable, so inevitably you end up cheated and get much less than you need. Here are 2 examples, both are protein powder isolates, containing the most protein in a concentrated form:
soy (plant): 1.116 gr per 100 gr soy isolate with 65% bioavailability makes this into 0.725 mg only
whey (dairy, so animal-based): 1.4 gr per 100 gr whey isolate
So just by drinking a protein drink a day, eating good quality red meat chicken, pork, fish, eggs, etc., will provide you with plenty of tryptophan to produce enough serotonin. In addition, there are now thousands upon thousands of people who have moved to a ‘carnivore diet” f animal products only, and have cured most diseases from depression to anxiety to arthritis to diabetes to GERD to allergies–the list goes on.
I understand your concern with bile duct damage, and that may present a problem but only for a moment. You can supplement bile easily, so there is no trouble then with your liver not being able to pass on enough bile. With this said and done, the ketogenic diet is not necessary. I just recommend you modify your diet such that you remove the biggest known offenders: grains, sugar, processed foods, and industrial vegetable and seed oils, and eat only whole foods that you cook from healthy foods you can buy: plenty of fresh eat, fish, eggs, veggies, some small amounts of high fiber fruits, dairy if not lactose intolerant (don’t use fake dairy, they are void of nutrients only have white color).
And a final thought: blood test for vitamins and minerals. I find that a lot of people just supplement multivitamins without ever finding out what vitamins they actually need. Taking vitamins that you don’t need may be harmful to your health, and not takign those that you need is also harmful to your health. It is vital that you have your blood tested for all vitamins. I know that most medical facilities look at my migraineurs when they request the list of tests I ask for in my migraine group like they were the little green men from plant X, but ultimately this is the only way we find out what you desperately need and what can harm you if you take it. I recommend you join my migraine group on Facebook to get a copy of the blood test I ask for, and then once you get the test back (both for you and for your daughter) we can evaluate what you need and why.
I also recommend you consider supplementing the proper B1–read the articles on HormonesMatter on Thimanine; they teach you very important facts about the role the correct thiamine format has and how it may completely turn you life around when you start supplementing it.
Long response to you here and I hope I didn’t overwhelm you. I think there is a lot that can be done for our health. <3
Best wishes to you and daughter,
Angela
This isn’t serotonin syndrome. It’s akathisia. Your poor, poor Mother was experiencing absolute torture. Please do further research via Dr David Healey’s website, RXisk, Mad In America. SSRI’s are massively overpowered drugs which lead to severe agitation (akathisia) and suicide or homicide. The facts are out there.
Marie,
Thanks for your comment. Akathisia is a very common adverse effect associated with most antipsychotic drugs and is part of serotonin syndrome. It is just one symptom of many. She didn’t have movement disorder otherwise and akathisia wore off as the serotonin wore off. It as clearly associated with the SSRI. The facts are definitely out there and I hope people read up on these drugs before they start taking them.
Best,
Angela
Angela, I wanted to Thank you for this article. i feel for you and your mom a million percent. When you say the fight of your life, you are not kidding. its the fight for their life with people who are supposed to more then you. you know how many times I have been shrugged off. my mom was put into a medicated induced psychosis by a pain management dr and a PA. all the while punishing my mom for being “addicted” to the pills he gave her otherwise would have no need or access to.
Needless to say she ended up in a mental facility for 10 days. I went everyday begging every doctor to stop the medication. They said if shes not on medication, they cant keep her there. I said ok, she doesn’t belong here. well she started to come back to herself as soon as they stopped medications. She remembered my phone number and was doing good. unfortunately she was still taking large amounts of norco and then morphine for a chronic back problem that Dr. kept giving her “muscle relaxers” for muscle spasms she complained of that later we found magnesium would help for .
But it is a warning sign to something more “opiod induced hyperalgesia” which mimic fibromyalga pains, headaches, bowel problems, agitation, anger, insulting(when you said that I know exactly what you mean how they are critical and insulting to every one) but instead of listening they wrote her,more medication. SSRI,SSNI. and today she is actually in the hospital since June 12th. for the first 6 days palliative care gave her large amounts of morphine , dilaudid, ativan. when it didn’t kill her they figured they better do more. traded 1 pill, the morphine for 6 muscle relaxers, seroquel, pain and more. her behavior changed before their eyes, they would’ve sent her home like that but i stood my ground and refused. so they are address it now that i got the patient relations involved. i have had to learn and take medical reports to prove they are not acknowledging what she has. my mom is 68. too young. and for those couple times i had my mom back i would talk to her about the whole situation to make sure i was on the right track, confirming my mom is still in there. today we are teetering on the shoulders of the doctor who got the worst of me and my demands of what and how to treat my mom. I still dont think they fully understand whats wrong with her. but I do and im demanding they listen. because sometimes the difference between life and death ====is just stopping the medication. i told them we tried your way for 2 weeks and she is worse. it will take less days to try my way.. Finding the lost mind….That’s what I am fighting for. and my hope comes from you today, again me searching for answers, proof to show dr.s, and I came across you article and i cried for you and your poor mom. i, so scared that will be my article to write. But today I refuse to accept that, and I will fight to save my mom. THANK YOU, YOUR EXPLANATION WAS RIGHT ON THE DOT.
Wow Brandi, you got my tear coming out for your mom and for you. You are fighting the battle I fought! Please be strong and firm and take your mother home. If I knew then what I know now, my mom would still be alive. It is impossible for them to not medicate as long as she is under medical care in their facility… so you must take her out of there. There is no other way! My heart goes out to you and her. I hope you are successful and can make a difference in her and your life! <3
Hugs to both of you and keep us updated!
Angela
Thank you for all the infomation you
have given me. It’s of great help.
I have not been able to tolerate
any meds since the serotonin syndrome 7 years ago. My BP
spikes when the hormones release.
I was on a very sm dose of Klonopin
0.25mg for a few years back but
I still experienced what I know now
as spillovers. I am not on any meds
now. Would it possible to join
your migraine group. My headaches
are better. I don’t believe they were
migraine. Ketosis is something
I would like to try with you and your
group.
Hugs Carmita
Hi Carmita,
Absolutely! Please join my migraine group! I have many members who have no migraines and are there in order to recover from other health conditions! 🙂 I would be very happy if you joined. I have 2 migraine groups. One is the Protocol group, which is my original group, where we help member reach “baseline”–a state from which one can move to ketogenic diet or carnivore diet. So I recommend you start there to get the basics. This group is here. The other group is newer (well… about 4 years old I think) and it has advanced members who wish to do the ketogenic diet, not all do. Here we also do what I call keto carnivore, which is slightly higher fat than protein carnivore and also practice hypercarnivore, which is very little carbs with a basic carnivore diet. You find this group here.
Please be sure to answer the 3 questions asked at the entry form and mention you come from here. Then I will know who you are. I have many admin helpers so admission will be by someone else.
I am looking forward to seeing you there!
Hugs back,
Angela
Angela,
Wonderful ! Can’t wait
Hugs to you
Carmita
My email doesnt always work, but i really need help getting off mreds that are not helping me that much, and ive been taking them on and off for almost 10 years now. I really need help.jacqueline
Please give help.jacqueline1000
Dear Jacqueline,
Have you contacted your doctor to ask guidance for reducing the medications? You didn’t say what medications you are taking and we cannot provide medical advice online. Every medication has a pharmaceutical tapering guide that even your pharmacist should be able to provide but it is your doctor’s responsibility to guide you through the process. However, tapering off the drugs, while it may solve the adverse reaction problems, it will not address the original problem because of which you started taking those drugs. You didn’t mention what those reasons were. If depression, there are thousands of anecdotal evidences on the internet about how the carnivore diet stops depression. If it is migraine, join my migraine group in Facebook. If it is something else, please search on google about what nutritional methods people used to combat their health condition.
Best wishes,
Angela
Hi Angela, I am sending this update to you here in 2020. My neuro-psyche doctor, Koller concluded that I was experiencing “spillovers”. He and I concurred that I try the alpha and beta blockers. When I took Atenolol, spillovers went into my chest with an over-abundance of restriction, while my lower body felt free and relaxed. When I was on the Prazosin, I felt that I went into a low: My symptoms were pronounced mood shifts and it was not helping the spillovers either. I therefore got off that drug after a week.
I have seen specialists such as neurologist, urologist and endocrinologist, etc. None have really been of too much help or really understood my symptoms. They don’t seem to understand the after effects of serotonin syndrome and the damage that it has left me. The neurologist would only check the labs that she wanted, but which I thought there were certain labs that could have given more indication to the symptoms that I have been experiencing.But anyway, the lab results indicated that I was high normal for norepinephrine and dopamine. She wouldn’t check the serotonin. She was concerned about the high blood pressure spikes I experience with the flow of hormones. She had me try Propanolol. I took one dose. I felt that I was in a pressure cooker. It was unbearable, so I got off it immediately.
Through the years, I have developed into a good researcher and found that the hormones spillover into my bloodstreams and cause the symptoms I experience all day long. It always feels like the sensations come up from my gut, builds up, spills over, builds up, spills over in a constant cycle. After it spills over, I have a short time period of peace. It seems that the hormones rush to every capillary of my body resulting in constriction for hours.
The research that I have done with the help of Dr Ben Lynch’s book, “Dirty Genes”, seems valid to my own experiences. Not too long ago, I had some genetics testing done. This concerned what drugs I can and cannot take. I found that the COMT gene has played a big part on why I am in this position today. I don’t metabolize hormones very fast. Hence, they build up and up. Dt Lynch is a wonderful writer and knows aspects pertaining to this subject that few others do. “Dirty Genes” is simplicity at it’s best. For me, because of damage to my receptors, caused by serotonin syndrome, I am not able to follow his instructions to the “T”. Nor am I able to follow anything to the “T”. But, I did get one thing out of the book, and that is: changing the amount and the times that I consume protein, has made some difference in my spillover times throughout the day. The spillovers have decreased somewhat.
My question to you Angela is, because serotonin, dopamine and norepinephrine work together, SSRI’s therefore damage not only the serotonin receptors, but also the norepinephrine receptors.With your expertise,have you ever known or researched a case like mine? I personally, haven’t seen any case quite like it.
I value your intellect, your knowledge and your compassion. My husband has done some research and found that there is some promise in gene therapy and gene replacement. What do you think? Is it feasible?
Sincerely,
Carmita Baker
Hi Carmita,
I am familiar with Dirty Genes and also the work of Dr. Ben Lynch. Serotonin, dopamine and norepinephrine do work together when “in nature” but not so when SSRI increases only serotonin–at least I have not read anything along these lines. I would actually suspect that an overflow if serotonin would down-regulate the other two, but I have not looked into the literature in that. I am not sure SSRIs would have an damaging affect to the receptors of dopamine or norepinephrine because the damage to the receptors is done by the specifificity of the “plug” that fills up the reuptake receptor. It often damages the receptor itself.
The receptor is protein, whose folding pattern is essential to remain unchanged but the inhibiting drug may change this, destroying the receptor itself. However, the inhibitor only inhibits the serotonin reuptake receptors and not any others.
In terms of the COMT gene, most people carry some variant. There are basically 3 possibilities: slow metabolizer, intermediate metabolizer, and fast metabolizer–in addition to normal that I exclude here. All three I listed here have some properties that change how fast your body works through certain drugs. For example, fast metabolizers get no benefit from many drugs, including time release; they tend to metabolize it all at once and thus get overdosed (I am in this category). Intermediate is also increased in speed, and the slow metabolizers keep the drug in their blood for a very long time, thereby increasing drug toxicity.
These COMT variants are very common and there is hardly a person without some variation one direction or the other.
In terms of the heart medications and the lung problem: non-selective heart medicines, such as Propranolol, affect both alpha and beta, and are therefore extremely dangerous for people with any lung concern. Even selective ones that only occupy one can cause serious lung trouble. In addition, Propranolol is very well understood to cause long-term heart damage. I try to talk every single person who was placed on Propranolol to get their doctor to switch them to a selective one or a neutral one, like Atenolol. Atenolol doesn’t use any of the receptors and so it causes no problems for the lungs.
The “spillovers” that you are referring to exist for most people who came off of SSRIs or similar–for some time–particularly if they came off very fast. It need not be permanent. The brain can recover but for that a nutritional regime change must take place. The only diet that can help heal the brain is the ketogenic. You need to be in ketosis for that to work. It really does work. If you are off of Propranolol and all other medications that are for the heart (other than Atenolol, which is OK in ketosis) or brain, then you should try ketosis.
Best wishes,
Angela
I just lost my husband from either serotonin syndrome and or neuroleptic malignant syndrome. Had never heard of either of those before. Looking back, he had been suffering for a long while and not knowing until it was too late. He was on so many mind altering meds. The end was when he hadn’t slept for 4 days, was hallucinating etc.. his dr UPPED his meds. I don’t think the hospital understood what to do either… I would like to sue, but don’t even know how to begin… checking out his Dr.. I see complaints of him over prescribing Ssri’s .. I wish I understood the risks before it was too late!
Dear Donna,
I am very sorry about the loss of your husband. <3 It is terrible how some doctors prescribe and over-prescribe medicines without any understanding of how they work and what they do. Good luck on your possible lawsuit. In my mother’s case the lawsuit was impossible because of the number of doctors and hospitals involved. My mother was deliberately bounced between 5 hospitals and had over 15 doctors involved. This was a case too large under California law to be taken on by any attorney because the maximum award is only $250k no matter how many places and people were involved. Plus the Medical Board will protect all doctors–even if they prescribe a drug when they have no license and by law are banned from prescribing drugs. Unfortunately it’s a very corrupt system.
The only way to survive our healthcare system is by keeping ourselves out of it.
Best wishes to you,
Angela
Hi, I’m 39yrs old currently on xtampza er 36mg 1 po bid and norco 5 mg 1 po E 4To 6 hr pen for chronic pain. I broke my neck in several places this wasn’t ffg ound for 10 weeks even though I was in horrific pain and saw several doctors no one would listen. Had fusion of c6 and c7 3 weeks after getting my collar off I was slammed in the back by a horse while I was feeding them. Went to ER and was told it was all muscle to walk on it 2 weeks later finding I busted my hip socket and pelvis to hell. Along with finding 4 years after my accidents just how bad my spine is. I had been fighting depression I’m not able to do anything. I can hardly take care of my house myself. I decided I needed to see someone for it. I made sure the doctor was aware of my pain meds. She put me on zoloft. I started it monday. Tuesday I felt pretty good didnt have to take as many norcos slept good that night Wednesday was even better. I hadn’t felt that good in years. Friday I was in tractor supply and it hit me. I had this weird feeling in my arms that crept up the back of my head into a full blown gosh awful headache. My heart sped up so fast I had to sit down. Saturday was even worse went to ER. Sunday I felt horrible. Monday I went to PA’s office she was gone for the week. The nurse spoke to another who said stop it. It took a week for things to ho back to normal well kinda. I’m s th ik ll having the occasional weird feeling in my arm and chest.
What a horrendous and heartbreaking story. I am so sorry you had to go through that and I am sorry for the loss of your mom. I experienced my first syncope episode in my late teens. I just passed out and had some horrible symptoms for two days after. The second time I was 23 years old and the exact same thing happened. The third time it happened we were at Universal Studios and all the same symptoms. The fourth time was at work during a training class. This time it happened at work and I was a firefighter/paramedic. So I was immediately placed on an EKG. My HR was in the upper 20’s. My husband happened to be in the same class so he was there when it occurred. It told them to give me a second and I come around. However, I was not allowed to go back to work until I was cleared by a cardiologist. I went to the doctor who did a tilt test and a 24 hour monitor. During the tilt test I went down to a HR of 15 and third degree heart block. It took a couple syncope episodes for me to realize that my body actually gives me a clue it’s coming. After the syncope I feel like I have the flu for 2-3 days after. The cardiologist informed my I had dysautonomia and placed my on 25mg of toprol to prevent tachycardia which prevents the syncope. It worked wonderfully.
I got a new PCP last year and she thinks I have silent migraines. This year I decided to go get established with a cardiologist since we moved. He did his own EKG and stress test. I went 18+ minutes at a He felt I did not have dysautonomia and changed me from torpor to zoloft 50mg. I took my first pill Wednesday night. I started getting symptoms within the hour. It started with a rush feeling over my entire body. My body felt heightened, like there was electrical current running through it. That night I couldn’t sleep. I felt like I had taken some kind of speed. My GI tract was getting started then also. It was noisy and the diarrhea started and still hasn’t stopped by has slowed down. I couldn’t eat. If I did I would vomit. I could barely keep any juice or fluid down. It took me a good day to drink a glass of water. The day around 9am all the other symptoms started to hit me.
Muscle cramps
Chills
Twitching
Goose bumps
Sweating
Couldn’t eat
Barely drink
Headache severe
Dizzy
Shakes shivering
I discontinued the medication. No way I was tolerating that for weeks in hopes the side effects go away. So that night around 10pm I finally fell asleep. Went through 4 shirts due to sweating. Woke up the next day with a cough and SOB (I am an avid runner. I have run marathons). Cooking breakfast or having a conversation made me fell like I was running a half marathon. Even when I am sick I don’t get SOB like that. What I find to be interesting is that a lot of those symptoms are the exact symptoms I get the day after a syncope episode.
I have decided on my own that I am going back on the torprol. It makes no difference to me if I have the dysautonomia or not. That SSRI is not worth the side effects.
Wow, what a story you have there Michelle! You could write a book about it. Glad you noticed that you were coming down with SS! That is so dangerous and so few doctors recognize or even accept its existence. Congrats for having made a decision that may have just saved your life! <3
Toprol is a drug I was placed on for heart arrhythmia. While it probably helped some, it was not all that great and it hugely interacted with ketosis. So if you ever change your way of eating and switch to low or very low carbs, that drug needs to be changed. With this said and done, I must add that i have had heart arrhythmia for over 20 years and it is disappearing while in ketosis. I was not born with an arrhythmia apparently–as you were also not born with whatever issues you are now having.
I would recommend you try a few new ways of eating and see but ask for a switch to Atenolol if you consider ketosis. Toprol crosses blood brain barrier and it interferes with ketosis–I think it overdoses and is unable to clear from the body. Atenolol works very similarly without crossing into the brain (I did have 10 days of headache when I switched) but it didn’t interact, and my heart is making huge recovery, so I am already down to half the dose!
Good luck to you!
Angela
Thank you Dr. Stanton for your reply. I don’t have any cardiac issues at all. The one cardiologist just felt placing me on a beta blocker would prevent my heart from going tachycardia and he felt when that occurred my Parasympathetic nervous system would flood my body with acetylcholine and norepinephrine causing me to pass out. His theory worked, in that I no longer had syncope episodes. However I still get all the after symptoms as if I had. While I was working I was a liability for the city and I had to follow the orders of the cardiologist to go back to work. Now that I am no longer working I am going to stay off all the medications and see how I do. If I feel an episode coming on I will just lie down and elevate my legs till the sensation is gone. I am going to give that I try. Thank you for the heads up on toprol crossing the blood/brain barrier. I was unaware of that. I may have my husband talk to his doctor about switching. He was placed on it a couple months ago for hypertension. He has been changing his diet in hopes of getting off it.
I am extremely interested in your diet. I ordered the book and I am really excited about reading and researching it. We already eat a low carb diet except when I am training for a race. The only issue I keep having elevated cholesterol and I have been refusing medication because my ratio is good. LDL is 134 VLDL 14 HDL 81 and triglycerides 72. Giving me a HDL/LDL ratio of 1.65 below their danger zone. My concern would be adding red meat to my diet and the cholesterol ratio changing and being forced on to a medication.
That is awesome to hear your arrhythmia disappearing in ketosis. I love hearing a good story where hard work and effort come together.
Thank you.
Michelle
Hi Michelle,
Please don’t listen to the elevated cholesterol story. So many academic articles out there show that cholesterol–taken out of context, like it is for you–has absolutely no meaning. Your cholesterol is great–better than 99% of the people out there. The actual hazard ratio is calculated by dividing triglycerides by HDL (this only works in the US measuring system). In your case that ratio is 72/81=0.89, which is the best it can be. The scores are:
0.6-1 = best possible
>1-2 = good
>2-3 = OK but raising eyebrow
>3 the risk of cardiovascular problems increase
Total cholesterol is never a metric to use because it incorporates HDL (the “good cholesterol”), which is better if greater, but when it increases, your total cholesterol increases… also it includes a number like this (triglycerides/5) and this is totally funny because triglycerides are not even cholesterol… anyhow, your cholesterol is great. No need to worry about your LDL. If there is anything too look at to worry about that would be LP(a)–a cholesterol similar to LDL but it has a protein attached to it and that’s the sign that it is harmful, or high triglycerides (meaning over 150) and low HDL (meaning less than 50 for women).
In terms of my nutrition: it is best if you join the migraine group for that here, since I don;t detail the food too much in the book. I give only basic guidelines. In the group we have recipe books for free download, nutrition trackers, and a host of other tools to help you, plus thousands of people who have the experience by now what is best for whom–it is quite individual.
I change my way of eating seasonally:
–spring ketogenic
–summer LCHF
–autumn ketogenic
–winter hypecarnivore or carnivore
This works the best for me but each person has different “best way of eating”. 🙂
Hope to see you in the group,
Angela
Thanks for your post. I think I had seratonin syndrome. For 16 years I was on 10 lexapro, and 150 Wellbutrin xl in the morning and 25 zoloft and 2.5 paxil at night. It worked for me. And then we tried a change because depression was getting bad. Lowered the Paxil to 1.25 and upped the Zoloft to 50. I immediately got high – huge pupils, felt amazing like on ecstasy, then I immediately fell asleep. That week I needed very little sleep and felt amazing but in a bad way – and had horrible diarrhea, was flying high, and shaking so we lowered it back to 25. Then went off the Paxil and into withdrawal. Then back on to just 1.25 paxil and went hypo. or syndrome again – horrible agitation and insomnia. Unsure if I switched to mania or had seratonin syndrome. Then I got an antibiotic Levaquin while in withdrawal. Could have caused more damage!
Fast forward and I felt electricity coursing through my body and I couldn’t sleep at all – some sort of “mixed state” according to the doctors when I went to the ER. Now I’m off the Paxil and zoloft and on 900 lithium along with the lexapro and Wellbutrin xl. Tried to lower the lithium from 900 to 780 and am having horrible chest pains (tightness like you couldn’t imagine), ear ringing, numb hands and feet at times, insomnia, freezing cold.
So many things are messed up in psychiatry. Generics are all different – which is most likely why I got depressed when I switched jobs and the mail order pharmacy changed.
Just though I’d share to show others I get it too. I had a good run. I’m not so hopeful as my system is ruined. Gonna try rTMS next.
Dear Polydrugged,
I am very sorry to read your words. There is no such as “mixed state” as a medical state… that is some “mixed state’ of doctors not able to figure out that you had serotonin syndrome. Glad you have survived the event. And while you are doing well on lithium, it s known to destroy the kidneys. It would be best to change your lifestyle to see if that helps. I am not an MD so cannot make any recommendations but I surely can recommend you to search the internet for success stories. Here is a web page you may want to check out. her story is amazing and quite relevant to you.
Best wishes,
Angela
I know this is an old post but I’m hoping you could help me
My 18 yo son is suffering from major depression and severe insomnia
Psych put him on Prozac and ambien
Ambien didn’t help so he tried whole slew of drugs to help him sleep and the insomnia just got worse
He developed a tremor. Psych said from sleep deprivation
He started having rage attacks, psych said from depression and sleep deprivation
His neck started twitching. Same explanation
Psych kept insisting Prozac wasn’t the cause and we should hang in until it took effect on depression
I knew something was amiss and took him to the pediatrician who noted that his eyes were dilated and said we should see neuro and ask the psych about Prozac side effects
That might my son developed muscle rigidity that lasted over an hour. I didn’t have the presence of mind to take him to ER but I did decide to stop all drugs
Thank God most symptoms have resolved all but the rage which is probably the worst. We are waiting y see a new psych, I’m boiling mad that the first one missed the signs of SS. Anyway, he’s still suffering from depression. We were hoping ssri would be the answer but now we know that it isn’t
Where do we go from here?
I’m heartbroken to see my child suffer like this, he needs serious help and I don’t know where to turn
We did do a genetic test which showed mthfr variation so maybe folate is one place to start but how do I know what he should be taking?
If anyone can offer me guidance I will be forever appreciative
Thank you
Dear Amy,
Have you looked into his nutrition? I know it may sound odd that I recommend a double-check on that but most (if not all) psychological problems are driven by insufficient nutrition. And while it may not appear to be connected, consider it seriously. Here is what I would do:
The brain is over 80% fat and cholesterol and this fat and cholesterol layer is damaged by sweeteners and insulin. The damage these cause can disrupt communication between neurons and can cause all kinds of neurological problems–including very severe ones.
So, as a first step, I would look at what he eats and drinks. The things I would consider cutting from his diet are:
–all sweetened beverages (no matter what they are sweetened with)
–all caffeinated beverages
–all juices, smoothies, shakes–except protein shakes but better eat protein from meat, fish, poultry, and eggs
–all processed foods
–all seed and vegetable oils
–all grains (including cereals, toasts, and anything grain)
Instead, I would try a wholesome diet rich in fresh proteins (meat, fish, eggs, poultry) and high-fiber vegetables,olive oil, avocado oil, coconut oil, butter, and animal fats. The nutritional change should start showing up within a few days. There are many stories by people doing this with severe neurological diseases. Medicine is seldom the best answer–particularly for a child.
For the MTHFR variation: having that variant doesn’t mean it is active, though it is highly possible given his health. Please ask his doctor to check his folate (B9), B2, B6, B12, and D3 via a blood test. B12 should be close to the top of the range, so if the lab range is 200-1000, his B12 level should be between 700-800! So if it comes out 201, it is not sufficient even though it is within the range. It is also bad if his B12 is higher than it should be–that too indicates that he is unable to metabolize (methylate) B12, so then you will need to have him supplement with “methyl cobalamin” form, the premethylated one. Folate is “methylfolate” if he needs to supplement it.
If he is on the vegan/vegetarian diet, that can cause the type of problems he seems to be having. In that case he is deficient in just about every vitamin and mineral and also essential amino acids (proteins) and essential fatty acids (omega 3 from fish and similar, and omega 6 from nuts and seeds). Be aware that the vegan diet has killed children, though younger than him.
I hope this helps. I deliberately didn’t talk about medicines, because my first approach is nutrition. Ii is now understood that nearly 100% of non-communicable diseases are caused by nutritional deficiencies. That is where you need to look first.
Best wishes,
Angela
Thank you for your response
My son’s diet is pretty clean
He eats close to zero processed foods, no take out ever, no sweetened drinks
His mainstays are salmon, eggs, unsweetened yogurt, and fruit and vegetables. He drinks water, herbal tea and kombucha (recent addition)
We use olive oil
He does also eat almonds and recently started adding grains into his diet but that’s only been in the last week. His depression/insomnia has been going on for at least 6-12 months
He used to eat chicken and beef but in the last couple of months it’s been leaving him feel ill so he stopped
We have an appt with another psych today, what is your opinion of TMS?
What type of professional should I seek out to guide us nutritionally?
Do the rage attacks from SS ever heal?
Amy, his diet seems OK. SS doesn’t last for a long time… if he has SS and it untreated, it either heals on its own or gets worse and his life can be in danger. It seems to me that this may not have anything to do with SS.
There are other conditions that may cause this–it may be as simple as B vitamins. He may not be able to methylate. There is a genetic condition that prevents B6 from metabolizing, causing anger and depression. There are many things to test with him and SS is not one of them since he has had these symptoms for some time. I would recommend you look into other things–no psychological but gut biome, vitamin, and mineral deficiencies.
Best wishes,
Angela
Hello. Please heed the excellent advice you have received about your son’s nutrition intake. I would like to offer my experience with having my own neurotransmitters tested. I was taking methylated folate, which is called methylfolate, at the advice of a very respected doctor, who had also run the MTHFR genetic testing on me as part of en executive physical. His comment was, “we don’t know if the gene is active, but taking methylfolate will cover the bases.” Sounds logical, right? In my case, consistent intake of methylfolate lead to the destruction of all my serotonin and it increases the production of adrenaline. When these 2 things happen simultaneously, you experience rage, insomnia, depression, and in some cases, suicidal thinking. I’m not trying to scare people, but rather point out that methylfolate is very powerful and should not be taken without regular review. It is also a deceptive case in which you would never suspect that an ingredient in your multivitamin is causing HUGE, negative repercussions.
I was taking 400mcg methylfolate consistently everyday, and had reached saturation state. Methylfolate has a very long half life, so discontinuance of intake does not yield results right away, the half life is 8 weeks.
So be careful with consistent intake of methylfolate, as it passes the blood brain barrier and is also stored in our red blood cells. Because the manufacturers advertise it is 7 Times more powerful than folate/folic acid, it seems to me that the dose should be divided by 7, so taking about 50mcg would make more sense. So why are they putting 400mcg in the multivitamins? Because there have not been enough tests and in some respects, the Big Pharma companies want us to experience the negative side effects so we turn to them for yet more drugs, such as antidepressants and anti anxiety medications.
Indeed Sally! And what scares me very badly is that, in some countries, B vitamin testing has no lab ranges given!! They provide the minimum required but not a healthy upper maximum, and so many people are either over-medicated with high doses of supplements, or, something even worse, cannot absorb the vitamins they take and they build up in their blood to very high levels, causing severe damage to the nervous system.
Hi Sally,
Appreciate this is a while ago now, I’m in the same boat with folate. Currently awaiting my neurotransmitter and blood/urine catecholamine/metanephrine levels but I have all the symptoms of excess adrenaline and/or it’s metabolites. It’s been 4 months since stopping folate and no improvement, it’s very severe! Just wondering how long it took you to recover, whether anything helped/hindered and whether you monitored your adrenaline pathway levels at all?
Thanks, Chloe
Dear Chloe,
Folate in the body is stored for over 4 months but if you are talking about a L-methylfolate supplement, it’s half-life in the body is about 3 hours. What folate were you taking? There are many kinds and some are dangerous whereas others are just fine.
Angela
Dear Angela,
It was methylfolate for a few days then switched to folinic acid for 3 weeks. At first I started to feel a little jittery with sleep disturbance, then symptoms exploded and but the time I stopped the folinic it was too late. Since then, a severe permanent headache, fight or flight mode, complete insomnia, tingling, along with a new food intolerance to phenols. I’ve been worked up by doctors and nothing found so far to otherwise explain these symptoms, and I arrived at the adrenaline theory after seeing that more folate can lead to more SAMe, with noradrenaline being a major methyl acceptor (to become adrenaline) and serotonin been a methyl acceptor (to become melatonin). I will update this thread with my neurotransmitter tests later in the week (as it might help others navigating adverse side-effects) but if you have anything to add or ideas that’s much appreciated. My folate level has now returned to baseline and it’s been 4 months, but the effects/metabolic impact of the folate remains.
The exact same thing happened to me due to taking folinic acid and a huge number of other supplements prescribed by an ND. I ended up in the ER with suspected serotonin syndrome and almost went into a coma after experiencing seizures. That was last spring, and I have not been the same since. What did your neurotransmitter tests say? (And what kind of Dr did you find that would test them?) Thanks in advance.
I started taking Lexapro last year after being on Zoloft/seroquel since 2015 and weaning off it. Things have gotten progressively worse. I weaned off of it myself last fall and started having panic attacks and nerve pains, pressure and popping in my head, as well as a weird head twitching jerking movement which I identify as either a neuralgia or some type of tardive akasthasia that I thought was a rupturing aneurysm. I have 4 kids 9 and under and have been barely able to care for them since. My dr put me on pristiq then back on Lexapro ..,the pooping pressure continued to get worse. and things went downhill. I have been to a neurologist who added gabapentin which was absolute hell. Suicidal thoughts constant confusion and severe mood swings. I finally stopped taking it and I’m now on 5 mg of Lexapro. Every time I take a dose I get a burning headache and the pressure popping g coming back and head jerking. If I hold off a few days it goes away until I start getting nausea and brain zaps dizziness then I’ll take a dose to prevent withdrawal and the weird symptoms coming right back. I don’t want to go through withdrawals again or I’ll be feeling sick for weeks and can’t handle that while being a mom. Drs don’t listen to me and I won’t even waste my breath trying to explain anymore.
Dear Hopeless,
I hope you will change your name to Hopeful from Hopeless. <3 There are lots of reasons to be hopeful. Why did you need to start taking Lexapro? Did you have migraines? Depression? It is important to know which so I can help you. Withdrawal symptoms can be reduced (or eliminated) by reducing the medicine properly and slowly and at the same time changing your lifestyle such that you prevent the condition you were trying to overcome with the medicine. This is why it would be good what you used the medicine for.
Angela
Hello,
I Know this is too old and I hope you’re doing great now.
I started having anxiety attacks due to stressful life pressure and I tried to avoid Medication and decided to self medicate.
I started self medicating with 5htp. I realized after taking a 100 mg dose that something was wrong, so I decided to take 50, still no changes. I started taking lower and lower in hopes I’d get some relief, but I didn’t. Instead the headaches got worst and the head started popping and hurting especially after waking up to a buzzing sensation in the top right corner of my head (inside) and really loud high pitched noise. ( I started having doubts of being a victim of the Havana syndrome).
I went to the ER and they said nothing was wrong after all they had done. I was honestly thinking that I was having a stroke or something.
I went back home but the headaches lasted a really long time, and I had to keep popping ibuprofen pills over a long period of time and I developed tinnitus. After a few months I decide to try it again and I only start with a dose of Less than 20 mg and I get the same popping sensation, the burning sensation in my brain as if it’s on fire and the Tinnitus gets worse.
I am honestly thinking about heading back to ER as I’m writing this, but I was really thankful you wrote your experience here. Because I relate to everything and It helps track possible causes.
I have only a question concerning side effects please and that is as follows:
Do you feel like you developed bruxism? Or do you grind your teeth all the time? I already used to clench my teeth due to anxiety, but after taking the 5-HTP, I started to additionaly grind them.
Thank you !
Archie
Dear Archie,
Thank you, I am doing great. Serotonin works in the serotonergic pathway rather than the dopanergic, and the two are not connected–please see at this article. Therefore, taking serotonin for anxiety won’t be helpful, since anxiety is associated with the dopanergic pathway.
Since I have never ever taken serotonin–this article is about my mother–I cannot tell you what side effects there may be other than what are listed via a google search.
I recommend you stop taking the 5htp since it is clearly the wrong medication for you–and actually it is not even a medication just a supplement. It is best if you don’t self medicate.
If you don’t want to take the medication prescribed to you, that’s totally your choice and I applaud you for your decision, but then you also shouldn’t self-medicate.
I hope my answer is helpful,
Angela
Hi Angela,
I found your blog post after having a scary experience with what I believe was SS. I had taken Lexapro for about 6 years, but decided to wean off it, and was medication free for a year. However, I relapsed and after dealing with debilitating depression and anxiety, decided to get back on the medication. I was prescribed Lexapro and Vistaril, and have been taking it for a week now. One evening before a big event I could not sleep. I took my medications, but later that night I decided to take Melatonin. The Melatonin also had 5-HTP in it. I took two capsules. For hours after I was tossing and turning because my muscles were so restless. I could not bare to stay in one position. It almost became painful and I had to “shake out” my muscles in a sense. I started to become disoriented, because this did not phase me so much for a while. Finally after so many hours I decided to get up to go to the bathroom, and I almost fell over, and I was having trouble walking straight. I then noticed my vision going blurry, and I also was losing control of my thumbs as I tried to type on my phone. My pupils also looked dilated. My heart was beating fast, and then it would slow. After doing some research, I decided to take myself to the ER, fearing the worst. (I live alone). When I got there, I found it difficult to walk and to speak. I also could not remember my social security. I was aware of everything that was happening, but felt very disoriented. I could not explain my thoughts coherently, but explained to the doctors what I thought was going on. Well nobody took me seriously. They thought I was having a panic attack, and were actually mocking me, saying I don’t know what i’m talking about. (I know what a panic attack feels like, this sure wasn’t it). I also could not express myself coherently at the time, as I was still very disoriented. They did give me a Benzo (which they said was for my panic attack, NOT SS). I didn’t care, as long as I was getting treatment, they didn’t need to believe me. I did in fact have high blood pressure, but no fever. I believe I had a mild case of SS. After taking the Benzo, I felt better a few hours later.
I know that I am very sensitive to these types of medications. years ago I had intense withdrawal symptoms that felt like my head was exploding (brain shocks). i am going to try to wean off this medication soon.
Hi Kristina,
What condition did you have for which you were/are taking these meds? May I ask? If migraine, please join my group here.
Best wishes,
Angela
I had a personal encounter with Prozac in my 30’s. I believe everything you say. I was prescribed Prozac and immediately just loved it – too much. I was in a hypomanic state that was thankfully diagnosed eventually but not before I was in a self-destructive state, not meaning suicidal but changing my life in careless and “fun” ways. I started drinking too often and could get very drunk – with blackouts-but never had a hangover while on Prozac! Red flag! Now that would be quite attractive to many people but it didn’t occur to me that was unusual. I was not ‘In touch” with my life, so to speak, yet underneath all the fun was a sneaky depression that was trying to takeover. Thank God for my understanding, forgiving husband and a friend who was once my therapist. When I got off Prozac, it was like my feet hit the ground and I could think clearly. Managing chronic pain and fatigue for the past 20 years, I am on a different SSRI at half the dose most people take. I realize I am very sensitive to medications. Even so, it is my belief that Prozac is in a class of it’s on and people react to it differently. I do not believe it should be on the market.
Dear Connie,
I totally agree with you. I don;t think that this drug (or similar) should be on the market.
Angela
A functional medicine doctor had me taking increasing doses of l-Theanine, 5HTP and Kavinase (phenibut?). A test showed high serotonin. I had been having occasional incontenence and absence seizures. A neurologist said I was depressed and needed an SSRI. I knew nothing about serotonin syndrome at the time but did mention to him that I tested high for serotonin. He convinced me to try Prozac. By the 5th pill I could not walk. My legs felt like they were filled with cement. It was very scary. What gene is related to serotonin? I’m thinking maybe genetics and the large doses of those supplements contributed to high serotonin tonstart with.
Dear Jaci,
I am very sorry to hear what happened to you. I checked at the human genome website what genes are associated with serotonin here but there are 2655 genes associated with serotonin is some way. I have no idea which ones may cause to have to much or too little or overly high sensitivity to serotonin. How fast a drug breaks down in your system also matters–that would be the CYPxxx gene where xxx stands for letters and numbers as it is a large family. Prozac is an SSRI so that can cause trouble for just about anyone.
Best wishes,
Angela
I wish doctors would use natural things like fish oil, and magnesium for depression. There would be so much less side effects and death due to ignorance in situations like this. It is really bad here in Oklahoma. I am hiv positive and all doctors care about here is whether you are taking your meds, and what other kind of medication they can get you on.
Dear Sean,
I agree with you very much. They often have a financial incentive to prescribe medicines.Unfortunately though not every supplement helps, and often there is no better option than medicines.
I wish you well,
Angela
Hello,
This is an interesting article here. I have an anxiety disorder. I hadn’t ever had anxiety so bad that it ever disrupted my life until last June. I had a series of panic attacks (I was facing a large promotion at work). Usually when I have a panic attack, I might be stricken with fear for a week or two but then go back to normal life. Usually my stints with anxiety had been years apart…until last June. I decided to go to my medical doctor to see about medication as I needed to be able to blaze through my promotion without all the panic. She put me on a low dose of Zoloft. I took one pill before bed as directed and did not sleep the entire night. I had diahrrea, vomiting, scary hallucination type thoughts and dreams that would either impede falling asleep or wake me up as soon as I did fall asleep. I had thoughts of death and a whole lot of panic attacks. The next day, I was lethargic, and paralyzed with fear and anxiety. I could not stop my mind from thinking a thousand miles a minute about every bad thing possible. I couldn’t handle in laws stopping by unannounced. I just sat there silent staring at the floor paralyzed with fear and sadness. My husband came home for lunch and I forced myself to take him outside to tell him that I shouldn’t be alone and that his brothers should go home. My husband called off of work and stayed with me in the bedroom while I cried for hours. I called the doctor who urged me to give the Zoloft more time. I refused. They told me to just stop taking them then.
I have NEVER been the same. My anxiety has never gone back to what it once was, which was a mild case that did not stop me from living my life and having fun.
What brought me here was a psychologist that told me that my symptoms sounded like “Serotonin Syndrome”. My question is: Are there any cases where this syndrome has permanently altered someone’s brain chemistry? Or is it possible that that one 24 hour period seriously traumatized me? I cannot find any information online. All I get for results is “How PTSD is treated with SSRIs. I want to know if this experience actually caused some sort of PTSD, and if that is why I have had such a difficult time getting back to my old self as I was a year ago.
Thank you
Dear Angela,
I am very sorry to hear what happened to you. Unfortunately there is no clear answer to your case. I have not heard of any long-term effects from serotonin syndrome–like potentially in your case. It is unclear to me what actually caused your severe reaction.
It is not unheard of to get serotonin syndrome from a single pill but it seems to be unheard of that it continues once the SSRI is out of your system. With this said, SSRI’s have an inhibitory function and they can cause permanent damage. The inhibit the serotonin reuptake mechanism of the neurons. The reuptake is a sensory mechanism that tells the cells to stop making serotonin when there is plenty in the synapse (between the neurons). This mechanism is what SSRIs block, so that the neuron doesn’t know that there is enough serotonin in the synapse and it keeps on manufacturing more and more.
Permanent damage to the inhibitors can occur though it is hard to envision that this occurs to so many neurons at once that it causes such long-term concern. I don’t know if there are any cases recorded anywhere and I am also unaware of any way this can be tested or looked for. I am sorry but I have no solution and probably no one will since if it can happen, it must be extremely rare.
Very sorry that I cannot be of help. I wish you good luck in recovery,
Angela
Angela…..can you please let me know how you are doing? I have been struggling with the same issue. I have been put on numerous SSRIS in the past year….even at miniscual doses and have suffered from severe panic and anxiety everytime and ever since EVEN AFTER STOPPING THEM. I am at my wits end. I have not been able to sleep without using ativan and that only gives me 2 hours or so at a time. I have compulsively been researching and your experience sounds just like mine.
Dear Lauri,
I am very sorry to hear about your experience. What I wrote was my mother’s story and not mine. Luckily I have never been on any SSRIs so I don’t have any first-hand experience. Also Ativan, it was my mother who was placed on that and not me. I have been on Valium (diazepam) instead. My story here is my scientific explanation of what happened to my mom,
It is important to understand why you are taking those medications: SSRIs are not for panic attacks. Panic attacks are the result of over-reactive alert system, which is usually triggered by some vitamin/mineral deficiency. B1 and B12 deficiencies are extremely likely. SSRIs are workign the serotonergic pathways, whereas panic attacks are on the dopanergic pathways and the two don’t directly meet. So taking SSRIs for anxiety and panic are useless.
While Valium (diazepam), a long-acting benzodiazepines, is very good for anxiety and panic attacks, Ativan is a short-acting one, like you write: 2 hours and you are up. Ativan is one f the worst possible benzodiazepines class medication ever created (right after Lunesta and Ambien, which are even worse). The half-life of Ativan is so short that is causes very strong dependence and then addiction. It is best to not take Ativan at all. If you can, ask your provider to prescribe Diazepam, which has a half-life of 26-50 hours (half-life is liver dependent in how fast your body works through it). Even at 26 hours of half-life, it is satisfactory to take it every 2nd day, or at max once a day, in minimum dose.
I recommend you start taking thiamin (B1) is a fat-soluble formula, such as Allithiamine (50 mg capsule) or Lipotiamine (50 mg pill), and check your other B vitamin levels. It is likely that you will either be very low or very high in B12. Both of those indicate trouble. Very high means you cannot methylate it and it builds up and very low means you are not eating the right foods to get enough and/or you are unable to absorb it from food. B12 should be within 80-90% of the upper range given by your lab.
I recommend you read this articles on thiamine deficiency, which cannot really be tested accurately via blood test. It will always show normal even when it is way below normal: here, here, and here. I can honestly say that I, who also has had panic attacks and anxiety my whole life, have completely recovered after supplementing 50 mg Allitiamine for 1-2 months. I have been taking B12 either as shots or sublingual for years but my anxiety and very easily triggered panic attacks only disappeared after taking this form of B1.
These supplements don’t interact with your medicines but definitely test B12 before you start takign any. Too much can be just as harmful as too little–both can cause permanent nerve damage. Once you started taking these, your problems will disappear, and then, provided you also make lifestyle changes in the way you eat, you will be able to completely quit all of you medicines after a slow taper. If your insurance doesn’t pay for B12 blood test, you can get it done via online labs like RequestATest, or others that work similarly, and are available in every state.
Best wishes and keep me posted,
Angela
Hello! I wanted to say, wow, I am new to your site but a permanent visitor now! I appreciate the work you have put into this article specifically because I am starting to understand myself how destructive the lack of knowledge regarding these medications and their interactions can be.
I am relatively young, 19, and have been on and off medication a couple times now. I currently take Adderall XR and Paxil. My question is, how long can Serotonin Syndrome go without being noticed? I started the Adderall about nine months ago and have been on Paxil for probably a year if not a little longer. I have definitely noticed some changes in myself since starting this combination and even more so since the Paxil dose has increased.
– I sweat excessively. Almost constantly. It is a little embarrassing but more concerning to me is the fact that I never had an issue like this before. I can literally drink 64 oz of water a day and go to the restroom once (meaning I sweat that much out that it doesn’t even make it to my bladder). What’s odd to me is that it doesn’t even need to be a warm day- I sweat just as much in cooler temps as I do warm. I’m trying to embrace the natural mechanism my body has for cooling, but this seems a little abnormal.
– I get very jittery around an hour to an hour and a half after taking my medication. I take both in the AM as when I started Paxil, I started taking it at night and it would increase my pulse so much I could not fall asleep. My doctor just said to take it in the morning so I did. Since combining with Adderall I have noticed a severe “rush” effect. It’s like downing a giant energy drink- lasts for about three to four hours then I’m back to normal. What I can’t figure out is if this is indeed an off reaction or just the Adderall entering my system.
– I’m very heat intolerant. Especially since starting the Adderall. I have noticed I cannot spend more than fifteen minutes in 70+ degree weather without sweating like crazy and feeling like I’m sitting by a fire! I’m not a big fan of summer heat but I have never noticed this to such an extent. I’ve been trying to take frequent breaks, drink plenty of fluids, and wear comfortable clothes to help mitigate this but it definitely seems to have worsened.
– Since starting Adderall it has become more frequent that I get severe leg cramps at night. Every week and a half or so I get excruciating ones where I cannot even bend my legs. It feels like someone is twisting my calves in knots!
I don’t know if you can give me any advice but I would really appreciate insight from someone who understands this, because my doctor has only been interested in upping my medication doses or adding more medication which I feel like is a bad idea. I’m no stranger to the lack of knowledge doctors can have on dealing with things which they are unfamiliar with, and I’m trying to heal myself through diet and lifestyle changes as much as I can (minimizing refined foods, sugar, increasing healthy fats and lots of fruits and vegetables, increasing my magnesium and vitamins B and D). From minimal research I found that combining Paxil and Adderall is almost always an “advised against” thing. My doctor doesn’t seem very thorough in educating me in what these meds can cause. I didn’t even know about serotonin syndrome until I googled some things I was experiencing! (I know, Google diagnosing is bad, but it at least brought me some information my doctor didn’t give me.)
Dear Allison,
I am very glad that you have contacted me. I placed the two drugs into a drug interaction checker here, and found the following major interaction (I bolded the ones you are having):
The sweating is probably a side effect as well–you are correct, sweating that much is not necessarily normal, though the not urinating much may be. If someone is drinking the right amount of water such that it actually absorbs the way it is supposed to absorb, urination is reduced. Your body gets rid of water in other ways, such as moistness of your breathing, your mucus membranes, your feces, and the moistness of your skin–without sweating part… just not dry skin. I well-hydrated body with proper mineral-enriched (electrolyte) concentration of water need not urinate that often. I am not discounting you sweating–that may be off as a result of these two drugs. The heat tolerance also hints at the interactions of the two drugs.
These drugs are somewhat opposing each other’s function as well. Adderall is an “upper” that makes you more alert and excited, whereas Paxil is an SSRI that is also used for anxiety and depression (albeit not very successfully for either) reduction–so they are “downers”. I suppose your body doesn’t know if it should be excited or calm. Adderall also initiates more serotonin release, plus a host of other neurotransmitter releases. Indeed, you may have too much serotonin, which woudl then lead to serotonin syndrome–in time.
And I think the cramps at night are from Adderall. It connects to the exaggerated increase in neurotransmitters in you brain.
While some people will suggest that muscle cramps at night hint at need for potassium–potassium causes “resting potential” and those who believe in potassium suggest so to “release’ the grip. Unfortunately often that makes things worse.
Some people will suggest to take more magnesium. Magnesium’s job is to open the voltage-gates channels, such as the sodium-potassium channel that operates the action and resting potentials. The problem with this suggestion is that magnesium is an excitatory mineral, and taking more of it may open the gates more but what is there is nothing there to enter? Or what if it increases activity in the middle of the night and keeps you awake?
I say it is lack of enough sodium, since sodium is necessary for action potential and you are using more of it on Adderall. Prior to action potential the cells are in refractory mode, meaning they cannot open or close or do anything. It is this that causes the cramp. Given that your brain is more active as a result of Adderall, you are likely using more brain energy and that uses more salt. I work with migraineurs and we all respond extremely well to taking salt for cramps! In fact, I did that this morning. It takes the cramps away within a minute.
I have a more private question to you: you are only 19 years old and your brain is not yet fully developed. In some literature female brain development completes at about age 34. Psychotropics such as the two you are taking modify the brain–often permanently–and may lead to brain degeneration, something that should not occur in the brain except for old age. While I am not advising you in any shape or form, ADHD and ADD both are no longer considered to be “diseases.” Both are possible to initiate by the wrong kind of nutrition. Many of the diseases that are not bacterial or viral origin have nutrition miss-match as their origin. Nutrition miss-match is eating a nutrition you are not able to utilize properly–such as many people cannot utilize the Standard American Diet (SAD) or a plant-based diet (such as vegan or vegetarian).
Have you considered to reevaluate your nutritional choice and change to one that is nutritionally more complete?
I hope you find this helpful,
Angela
The more I read about this the more concerned I become. I almost lost my wife to serotonin syndrome about 3 weeks ago. The doctor in charge at the hospital she was taken to had absolutely no idea whatsoever about this condition. Furthermore, the EMTs who transported my wife treated her as a run-of-the-mill opiate overdose and their behaviour was reprehensible, not to mention dangerous considering the drugs they gave her.
I’ll wager serotonin syndrome kills more people than anyone suspects, and I agree with the sentiments expressed above in that it’s all too easy for MDs to prescribe SSRIs without spending the time and energy to truly assess a patient’s condition and/or risks.
My wife still suffers from stuttering and profuse sweating when she becomes exhausted – which happens easily and frequently – but it seems her seizing and muscle spasms have abated. I will say this: she’s a different person as a result of her near-death experience; filled with joy at having survived and deeply suspicious of any kind of mind-altering medications.
Folks, spread the word: SSRIs are killers in disguise.
Dear Simon,
I am very sorry to hear about your wife and your experience! Indeed, SSRIs are killers in disguise! I would say that probably a good 90%+ cases of serotonin syndrome are missed and placed under some other condition and mistreated until the inevitable fatal outcome. I am glad your wife has survived the ordeal. There should be a school teaching doctors about serotonin syndrome. I wish we could reach high enough to get that goal reached.
Many hugs to your wife and to you for helping her,
Angela
Angela, thank you for your article on serotonin syndrome. I’m so sorry about your mom. I’ve just heard about SS the last few days, my husband may be having this problem. He is taking suboxone (he was on opiates for pain for years before a back surgery) he is tapering down and doing well with that. He also has went from Xanax to Klonopin. So he takes the klonopin for anxiety and his dr has recently prescribed Prozac. He has been feeling sick for quite some time but I believe it has gotten a lot worse since the Prozac. He sometimes sleeps for 36 hours strait. He is almost always nauseous and dizzy. When he first wakes up he is confused and stumbles. He’s had diarrhea, dry heaves, sweating, shakes, and does have the muscles spasms and shakiness. He feels sick all the time and some days he can’t function, so he sleeps. I let him know what I found about online about SS and he said he would talk to the people that prescribe the suboxone on Monday. I don’t think any hospital around here would know what to do. Can he try to taper off the Prozac? I would love to hear your thoughts on this. Thank you so much for you time!!
Dear Kellie,
Thank you for your note about your husband. His experience sounds terrible. May I ask why he was placed on Prozac??? That is an SSRI. It seems he was doing fine with his reduction of opioids, so not sure why he was prescribed that. Klonopin is way better than Xanax, that’s a good choice. But why Prozac?
I think that his nervous system just feels completely attacked. He has enough trouble with withdrawals from pain killers and it seems the Prozac is interacting with Suboxone. Suboxone is a very powerful CNS drug on its own as is Klonopin; I would most certainly not have added Prozac into the mix. Please ask his doctor why and if he can taper off of that.
Best wishes,
Angela
Angela,
I just wanted to let you know my husband has stopped taking the Prozac, it’s been 6 days and he is feeling so much better! His appetite is coming back as well! Thank you again for this article! I believe you helped save his life!
Dear Kelly,
I am soooooo happy to hear this! Best wishes and a big hug to both of you,
Angela
Hi Angela. Thank you for this interesting article. Unfortunately, I just found out about your blog. Now I will definitely subscribe and follow the updates. Recently I read an interesting fact: “in the examined patients for a long time there was a “constant fatigue syndrome”, manifested by a decrease in efficiency and the need for frequent rest. Fatigue was not adequate to physical activity, violated the usual daily activity and made it difficult to do homework. There was a decrease in interests, a decrease in the ability to perform mental tasks. Almost all MS patients reported increased fatigue in the heat and after taking a hot bath or shower. However, fatigue complaints were often only detected in an active survey.” What do you think about it?
Dear FairPriceRx,
Would you share the link to the article? It seems to miss some connecting point–like I had no idea it was about MS patients till the end, and there is no such as “constant fatigue syndrome” so not sure if what you are reading is meaningful without reading it myself.
Thanks,
Angela
About 8 weeks ago I started having ear pressure, dizziness, fogginess & headaches. Dr 1 said it was a viral ear infection and put me on an antiviral. When it didn’t get better and it was clear that I was having anxiety, he put me on Prozac and put tube in ear. When still not better 3 mote weeks, got new ENT. He said get mri & see neurologist. Neuro said it’s likely migraines and gave me nortryptilene. The pharmacist gave me a handout warning me of SS so I called Dr and he said I should be fine and to take together. I m too scared but I need to get well from whatever is happening so now I’m just sad. I was healthy on 0 meds before all of this and have been given over 8 diff things now but these are most recent.
Dear K,
Very sorry to hear what happened to you. Unfortunately your situation is extremely common, particularly with migraines. Migraines are hard to diagnose because there are so many symptoms and one can have migraines without any pain in the head as well. Migraine always comes with prodromes. Prodromes happen prior to the migraine. They can start from 1 day to just minutes before, depending on the prodrome. Dizziness, fogginess, and ear pressure are all prodromes. None of the medicines you got works for migraineurs.
Unfortunately Facebook is down the whole day today in the US–I am told that not all over the world–so you cannot check us out today, but please join us in our migraine group here. We help you understand the cause of migraine and also teach you how to prevent them. I wrote a book about it as well, so if you don;t want to join, just read the book.
Looking forward to seeing you in the Facebook group,
Angela
Is it possible to get serontin syndrom on 10 mg cipralex combinet with affron extract 30 mg each day?
Hi Ashley,
I suppose you meant Saffron extract? Since it is an herb, what it does and how, is not studied. However, people with certain conditions have symptom that may indeed mimic serotonin syndrome. It can initiate anxiety and other mood disorders. I found the following side effects:
The above is from this link and click on “side effects”.
I would never ever mix Western and Easter medicines.
Best wishes,
Angela
Hi Angela,
What an amazing story. Thank you for sharing. Reading another story like this, helps me see that I am not going crazy! I just don’t get why serotonin syndrome can’t be more easily diagnosed, I’m not medically trained at all, but it is so obvious to me!
My husband has taken Citalopram for 5 years for depression. We got married 2 and a half years ago. 3 weeks into our marriage, he had missed 5 days of pills, he remembered and took one just before bed. 15 minutes later, his legs started to spasm, I asked what he was doing and he said he couldn’t control it. I turned the light on and his pupils were dilated. I instantly was concerned it was a stroke as he was talking silly too. But he passed the stroke signs. I began to cry because I was really concerned, and he just laughed uncontrollably, which was not like him at all. I checked the side effected of the citalopram and became convinced it was that. He had a really bad headache the next day. He went to the doctor but he did not think it was related to the medication and shrugged it off. (It has bothered me since).
A year later he started to get twitchy legs at night. His legs would spasm, and it would wake him up. He could not get back in bed without stretching. He was and is convinced this is due to lack of exercise, as he was not doing as much exercise as before we were married, yet he was/is still active (not in an office job or sitting down all day). At this point we had moved to Austria for 6 months, and he was unable to get citalopram quite so regularly, so he was ‘eeking’ it out. His legs would spasm most nights, but not every night, there seemed no pattern. This was from end of 2017, and still continues now. However it’s getting worse. I get awoken with a kick more than once in the night, and it still happens even if he has done plenty of exercise. His mood has also changed, and this is different to the depression. He moans about everything, and has an excuse for everything. 2 days ago, I suggested we went to a shop in town, I suggested we walked. It is 5-10 mins walk, a journey he has done many times without complaint. He moaned so much that we walked, that I regretted asking his company. I can’t ask him to do ANYTHING anymore without feeling bad for asking because he makes such a big deal out of it. (Just to add that I don’t suffer from depression myself, and while I am unable to understand, I have a lot of empathy and patience with my husband)
Yesterday, I researched Serotonin Syndrome and his Citalopram, this totally convinced me it is the problem and what is going on. He can’t accept it, because he says he is afraid that the answer will be to come off his medication. He went to the doctor this morning, who said he doesn’t think it is the citalopram, ‘because there has been no history at the surgery of anyone developing SS from taking that drug’ !!! He didn’t give a reason for why he is getting leg spasms night after night, just said that my husband could try take 10mg rather than 20mg and see if it makes any difference. And said, ‘drugs have some bad side effects, but you have to way up which is worse.’
After reading your story, I am even more convinced this is the problem, as he has been getting worse. As awful as it sounds, I am hoping that he continues to worsen, so that perhaps then I will be believed!
Please, if you have any advice or knowledge that can help with this battle, please do share. Thank you so much, J
Dear Jess,
Wow, what a story! Very sorry to hear what you and your hubby are going through. I have a question: he can skip Citalopram and have no adverse reactions when he misses a day? The reason why I am asking that is because Citalopram has such an incredible withdrawal (discontinuation syndrome) symptoms that I found it very odd that he cold skip even one day, let alone more! This can have several explanations, and the very first–and perhaps the most relevant here–is that it is possible that his genetics is set to slow drug metabolizing via CYP2C19, CYP3A4 and CYP2D6 and he is retaining too much of the drug in his blood, so he may be overdosed. This would explain (to me at least) how he can go for a few days without taking it and not suffer. The half-life of Citalopram is 35 hours!! That means that the dose sot of “piles up” because the first day’s dose has not yet even reached half-life when the next pill is taken.
This drug for those with the very slow and the very fast metabolizing persons can cause a very serious serotonin syndrome on its own, without any other contributing medicine. Dilated pupils is one of the signs of an overdose. I completely disagree with his doctor… there are many clueless doctors unfortunately. He may not be having Serotonin Syndrome (yet) but he is clearly showing signs of having been overdosed.
Please take this note to a different doctor–not the one who told him that this drug cannot cause serotonin syndrome–and have them reduce his medicine or discontinue it completely. Not everyone can take an SSRI!
Good catch on your part! Thanks for letting me know. <3
Good luck with the doctor and also with your husband. One of the signs of an overdose is that they become unreasonable and impossible to convince in anything. So please take charge.
Best wishes,
Angela
Hello Angela, what are your thoughts on the use of light therapy in combination with antidepressants (specifically Wellbutrin 300 XL)? Can this cause Serotonin Syndrone? I have felt a bit off since I started using the lamp a couple of weeks ago. The light has definitely helped my sleep; I no longer feel the need to take naps during the day but I’ve been feeling anxious. Note, I know Wellbutrin can be ennervating but I have been on it for many years and never felt this way.
Hi Marie,
I looked up Wellbutrin to see if it is a serotonin increasing drug but it isn’t so. It is an atypical antidepressant that in a norepinephrine-dopamine reuptake inhibitor–blocks dopamine and norepinephrine and indirectly has an extremely small activity on the 5-HT3A serotonin receptor by negatively affecting it–meaning it actually reduces its activity. Light therapy, by contrast, can increase serotonin activity, see here, which would work against, meaning not increase but potentially decrease, what Wellbutrin does, though only “potentially” since the effects for both the drug and the light are minimal.
Maybe what you now feel is an overdose of Wellbutrin as a result of the light, which naturally heals your brain; perhaps a dose adjustment is in order.
Best wishes,
Angela
Hi Angela.
I found this site, while reading about Tryptophan.
You seem to have so much of experiences over the last year on this topic, that i maybe may ask you a question.
I have the problem, especially in winter, that i can´t fall asleep at night. The only thing, which really works is Tryptophan. I need about 3 – 4 g per night. I don´t take any other presc. drugs etc., no antidepressants.
Do you thnink, that such doeses, for 3 to 4 g can casue a bad SS also? I´m just thingking about it, because i read, TP does work differnet that SSRI, and only very short halftime.
Is this still possible, to get a complete SS, or even a very light version of a SS?
Thank you very much.
Gregor
Dear Gregor,
Tryptophan is an essential amino acid, which is a precursor to serotonin–it is not serotonin itself. In the brain it does convert into 5-HTTP but to what degree and efficiency I cannot guess. Since it is a supplement rather than a prescription medicine, there is not official guideline that I can consult. I recommend you ask a friendly pharmacist for guidance. The most I can offer is a copy paste of the possible overdose dangers:
“Overdose
Too much tryptophan can cause additional problems. A tryptophan overdose can cause a condition known as eosiniophilia-myalgia syndrome, which can cause severe muscle pain, nerve pain, hair loss, fatigue, a rash, dry skin and high levels of a type of immune cell known as eosinophils. A tryptophan overdose can also cause serotonin syndrome, which can result in confusion, hallucinations, muscle spasms, trouble walking, increased sweating, fever, rapid heartbeat, faintness and diarrhea. There is no consensus maximum safe dose for tryptophan, so there is no set “unsafe” amount. However, MayoClinic.com recommends a dose of 8 g to 12 g per day divided into three to four doses.”
This I found here.
Based on the Mayo Clinic recommendation, your dose should be safe, provided you have no health concerns and are not taking other medicines and supplements that may interact. So please ask your pharmacist.
Best wishes,
Angela
After reading your articles and related comments, I found that the website of Dr. Peter Breggin (https://breggin.com/) can provide some insights to most of the problems. He explained how harmful the psychosis drugs including anti-depressants to human being, how psychiatrists/doctors prescribe those drugs out of greed and fear to the pharmaceutical companies, how other treatments like emphatic therapy, cognitive, behavior treatment can help anxiety and depression effectively and also how to wean off those drugs safely.
My mom is also being put on those drugs due to insomnia after her L3 spine collapsed . Since she is living in a nursing home in Hong Kong, it is quite impossible to have help her wean them off. I blogged with many translated articles in Chinese and hope to open the Chinese’s horizon about the problem of the whole biopsychiatry.
Dear Katy,
Thank you for your comment and the link to Dr. Breggin! Lots to read there! Indeed, big pharma power seems endless. Very sorry to hear about your mom. I totally understand your struggles long distance! I heard others have similar problems even if they are located in countries around that part of the world. It is not just the distance but also the lack of understanding and knowledge there.
Best wishes to you and your mom!
Angela
Oh my goodness Angela, what a terrible ordeal you and your mother endured. That’s inhumane. I can’t believe such things are permitted. I’m so sorry you both had to go through that. I’m shocked – my jaw is still dropped! – at everything that transpired. I just can’t believe it. What kind of system is in place that allows this? Your poor Mum… and you too…
My heart goes out to you.
Thank you for the genetics info. I am familiar with the adjunct sites for getting info. I will check out your templates for sure.
We sound to be alike in how we react to medications. I have never tried morphine (scary what you went through!) but I have asked my doctor if I should wear a bracelet as I react to so much. It will be good to learn what and why.
I am starting to have my eyes opened as to how these institutional systems work. I am going to do my best to stay positive while being the best advocate for my mother that I can be. I think arming myself with info is a good place to start. Thank you again for the great information you provided.
Take good care!
Lana
Thanks Lana! <3 It was indeed terrifying and shocking. Never go through what I did. Prepare better.
Hugs,
Angela
Thank you for this article Angela.
I can’t believe how close it is to what I am living right now.
My mother was diagnosed with Alzheimer’s Disease several years ago.
It has progressed to the point that she in now in a care home.
I am very involved in her care and am reluctant to have her on any medications but her insomnia got to the point where she needed something.
Not only was she not sleeping, but she was waking up in the night drenched in sweat and then she would become freezing cold. This caused her to panic.
I was told that it’s the Alzheimer’s brain having difficulty with temperature.
I’m now wondering if it could have been the natural supplements that she was taking – melatonin, turmeric, ashwagandha…
She was put on a small dose (15mg) of Mirtazapine. The first few days were great and then the confusion set in. And then the deliriums began. Without alerting me, they increased her dose to 21.5 mg.
She became angry and the deliriums were now commonplace. Thankfully, the head nurse was witness to one of the deliriums so she advised the doctor to take her off of it.
Fast forward a few months and her night time anxiety and insomnia is getting worse.
We decide to try her on 25mg. of Trazodone. I am assured that it is an extremely small dose.
At the same time, the doctor prescribed a PRN (as needed dose for anxiety) of 12.5mg up to 3 times a day. I didn’t realize what this was all about at the time otherwise I would not have agreed to it.
Once a patient in a nursing home is on a medication, it is very difficult to get them off of it. My advice – don’t agree to anything unless absolutely needed. I should have agreed just to try the Trazodone for her insomnia and then assess from there.
Again, the first few days were great and then the same pattern started again – the confusion, the anger and even some hallucinations. However, she didn’t have the deliriums that she had on the Mirtazapine. The problem was that the Trazodone worked. It made her sleep and it calmed her when they gave her a PRN.
When I phoned the doctor after a week of enduring these horrible side effects, he agreed she should come off of it and said he would phone the nursing home and speak with them.
A week later she is still having the side effects. I couldn’t believe that they would last so long.
I asked the nurses if they had her on anything else and was told – “No , just the Trazodone.”
The head nurse told the doctor that the Trazodone was working well and they didn’t notice any side effects – so he didn’t take her off of it. (!!)
It has been 2 months of doctors appointments and meetings and many hard feelings between the head nurse and myself – and my mother is still on the Trazodone. The head nurse keeps hinting that she will be kicked out if they can’t deal with her anxiety.
I keep telling them that the Trazodone is CAUSING her anxiety – they are giving her medication (PRN’s) based on side effects of that very medication. So frustrating!
Unfortunately, they don’t see it that way as the Trazodone calms her at the time.
I have an appointment with the Doctor tomorrow and I will ask him to reduce her bedtime dosage to 12.5mg. Dare I mention Serotonin Syndrome to him?
Is it really possible that someone could get Serotonin Syndrome from such a small amount?
What makes me think that this is a possibility is my own experience with anti-depressants for anxiety and Tryptophan for insomnia. They were some of the worst drugs I have ever taken.
I was diagnosed with Social Phobia which has now been proven to be a ‘high serotonin’ syndrome. I’m so thankful that I had a good psychiatrist who agreed with me about the anti-depressants (not that I would have stayed on them!). But he went so far as to say that I should never take ANY type of anti-depressant based on my side effects. At the time (many years ago), I didn’t ask why – I wonder if it was because of Serotonin Syndrome?
So perhaps we have a genetic configuration in our family that predisposes us to high serotonin. Then when even a small dose is given, these side effects show up??
My mother also suffered hospital delirium when she had surgery prior to being diagnosed with Alzheimer’s. She was in that delirium for 3 days. When she got home, she didn’t even know where to find cutlery in her own kitchen when we had lunch. She didn’t recover fully from that.
I feel torn as I don’t want her placed in a hospital type setting where she will most likely be drugged even more. I want her to stay at the home that she knows. So something needs to be done that will address her night time anxiety without compromising her sanity. Poor Mom.
Are there any medications that can be used in the elderly for sleep and anxiety without these side effects? The doctor won’t prescribe Benzo’s as they cause confusion in the Alzheimer’s brain.
He mentioned we could be her on a daytime SSRI… (GASP!)
So glad I read this article… I may have agreed to it out of desperation.
Really hoping we can find a solution that works…
Dear Lana,
Wow, what an amazing story. Indeed, once in nursing care, changing medications is almost impossible. Very sorry to hear about your and your mom’s struggles.
I completely disagree with to doctor who said that benzodiazepines will cause confusion in the Alzheimer’s brain. First of all, there is already a major confusion in the Alzheimer’s brain–which appears to be nutrition related (perhaps nutrition-caused). Benzos are the only true anti-anxiety medicines because they operate on the dopanergic-pathway of the brain. Serotonin, on the other hand, works the serotonergic pathways, which are not connected to the anxiety region at all. Furthermore, serotonin is a mood (and digestion speed) booster and there is nothing “mood” or “constipation” about insomnia. Serotonin and SSRI drugs have nothing sleeping-pill about them.
In addition, there is indeed a genetic condition associated with serotonin sensitivity–I happen to sport that gene as well and probably my mom did too, hence the saga she had to endure. I now have placed serotonin medicines on my list of allergies so that no one can give them to me. I registered with Medicalert and wear an allergy bracelet with that information. If you are also sensitive to serotonin–likely based on how your mom responds to it–you may also react badly to other nervous system stimulants or modifiers as well–such as perhaps you may stop breathing from morphine, which is what is my case. These are important to check before the need arises! So please do!
Not sure how much freedom you have in the nursing care but perhaps you can request certain blood tests from them for your mom–you may have to pay for them out of pocket if they even entertain such ideas. Some of the immediate things to check would be if she is deficient in B vitamins, such as B2, B6, B9, and B12. Particularly B12, a deficiency in that can cause agitation and insomnia–taking too much can also cause agitation, so having the right amount and the right type (methylcobalmin) is vital but a deficiency needs to first be confirmed. Also vitamin D3 has a lot to do with natural body functions associated with rest, repair, and healing. In old age, melatonin may also be lacking. And a final point, Alzheimer’s is beginning to be labeled as type 3 diabetes now everywhere.
As a form of diabetes, it hints at the causal mechanism of the brain’s inability to manage glucose properly because of glucose transporter issues and insulin resistance in the brain. Glucose has a free-flow in our body in blood but without insulin and proper transporters it cannot get into the cells. It then just fills up the interstitial space around the cells and causes damage–too much glucose is toxic. There is much research now on the connection of glucose/insulin to Alzheimer’s and some experiments are ongoing with placing Alzheimer’s patients on the ketogenic diet–void of any direct glucose and very low on carbohydrates with only highly fibrous ones offered. It appears to work extremely well. In extreme cases–late stages–offering MCTs or supplemental ketones are under investigation.
MCTs are available in all supplemental stores; they are very popular these days. You may find it useful to look into the matter.
Best wishes and lots of luck!!
Angela
Thank you for your reply Angela.
I’m interested in finding out about the genetics around serotonin sensitivity… would the 23andme testing give those results?
I will definitely do it for both Mom and I.
And a great idea to place Serotonin medications on your allergies list!
I’m fortunate that Mom’s doctor is open to discussing such things although he keeps saying – ‘she’s on such a small dose’.
Perhaps the genetic testing results will persuade him.
In the meantime, I am going to go through all of Mom’s natural supplements to see if there are any others (other than Curcumin) that increase serotonin. If it helps to remove those then I will know we are on the right track.
You have a good idea to test her B vits. I have a nutrition background so when Mom was on her own and I was playing a bigger part in her care, I would make her muffins and cookies with MCT oil and Erythritol instead of sugar.
I’m sure the low sugar diet with added ketones helped to slow the progression of her dementia, but it progressed nonetheless.
Now that she’s in a nursing home, I don’t have control over what she eats. And the snacks provided each day are always sugar snacks – even for the diabetics!
You say in your article: “She (your mother) was misdiagnosed and mistreated with the wrong medicines until she died. There was nothing I could do.”
Was there nothing you could do because you weren’t her legal representative?
I asked the doc yesterday how much say I have regarding Mom’s medications now that she is in Institutional care. He said I have a lot of say.
This is new to me as Mom was never on medication prior to this so I will find out just how much power I have as her legal representative. Of course, the nursing home could choose to kick her out so I guess Mom will ultimately pay a price regardless of how much say we have.
I really appreciate your information Angela. It’s been very helpful to me.
Kind Regards,
Lana
Hi Lana,
Yes, 23andMe is a good source to start with. If you get the more expensive package (I think $199 or something like that) you get the health list as well. It is standardized though so to know more, you also need another account, such as LiveWello, and there you can see genetic variances. I have created a lot of templates–they are under my name so you can find it. Most are migraine specific but there are some others. They have some general health checks noted there as well such as are you sensitive to narcotics? Would you get a negative effect from NSAIDs and stuff like that.
Note: genetic variances you may find don;t mean you have that condition. They just are possible to be expressed. You need to have it tested to be sure. With this said and done, I will not be testing narcotics to see if I am as sensitive as it is stated–I had taken morphine for a back injury–smartly cutting the one little pill into 10 pieces and I had to force-breath for 6 hours after that little piece… so I proved to myself coincidentally that I will die from a standard morphine dose, no matter how small. So I managed to prove one. Another one that is easy to prove–and you may have mentioned already–is getting pain meds, such as codeine, and that it has no effect. That would fall under fast metabolizer of medicines and it also affects time release meds–even OTCs like expectorant that has a time released formula. Don;t get that if you are a fast metabolizer because it overdoses you. So you can learn very important and fascinating things.
Your question about legal representation of my mom: I had full legal rights via attorney and fully signed and notarized but it was completely ignored everywhere. I handed it to the hospitals and nursing homes the moment she was admitted, everywhere, AND carried a copy in my hand all the time but everywhere it was overruled and they acted regardless of my rights–in one of the hospitals I actually decided to sleep on 2 chairs for 2 nights because I wanted to see what they actually want to do with her and so I could stop them! I ended up having to put a sign on the door “Patient trying to sleep here, don’t enter” because they were using her room as some diaper storage facility and someone was coming in every hour and slammed the door both coming and going. Incredible experiences!
I tried to sue after but was unable to even start a lawsuit because I am in California, where there is a maximum $250k per malpractice lawsuit (regardless how many people are involved), and since the medical institutions know this, she was like a soccer ball, taken to a new institution every 2 weeks or less! So there were 6 institutions in 7 weeks and in each institution over 5 people so the lawsuit would have become impossibly expensive–way over the $250k limit possible to gain so no attorney would take the case.
I wish you best of luck!
Angela
I tried to post earlier but it looks like it didn’t take. :/
My story:
I have had anxiety and depression much of my life. I am currently 32. Been on various meds for it over time, but currently take Fluoxetine and Buspirone. This past year I have also been suffering from migraines (didn’t realize that’s what they were, migraine newbie) and finally sought treatment.
Lets go back to two weeks ago. I normally take 40mg of Fluoxetine and when I filled my prescription I didn’t realize the pills were now 40 instead of 20 like I’m used to, so I usually take 2. I ended up taking 80mg for a week before realizing something was off when I went in for my migraine appointment.
The doctor made an offhand comment about how I take that changing. I was like, “Crap crap crap”. Anyway, I went back to my correct dose that night. I also started migraine meds that night. Trazadone and Imitrex. I had been feeling off, headaches besides migraine, nausea, diarrhea, off balance, drowsy, shaking. Just miserable. Which progressively got worse through this last week until today.
Went to the walk in clinic and talked to someone there who agreed I had too much Serotonin in my system, but now Serotonin syndrome. Slightly elevated temp and blood pressure and heart rate. Just a miserable, miserable couple weeks.
My question is what options are there for a migraine sufferer who also has anxiety and depression? Current med list:
Omeprazole 40mg
Buspirone 40mg
Fluoxetine 40mg (accidentally 80mg)
Clonozopam .5mg as needed
Trazadone 50mg (stopping immediately)
Imitrex 25mg as needed
Daily vitamin
Have had Tylenol and Benadryl here and there the past few weeks, not much on the benadryl, but Tylenol frequently.
I saw you have a facebook group for migraines, would love to join. Let me know what you think are my next steps besides stopping my one med, drinking lots of water, sleeping, exercising, and current meds. Miserable and frustrated. Thanks so much.
Hi Christina,
I will leave both messages since both have some different additional information as well, and that is useful.
So first of all, it does sound like you have serotonin syndrome. The fever is a major tip-off and I ma shocked that your doctor didn’t consider that! The first thing that I did is visited the official drug interaction checker–something your doctor should also have done: https://www.drugs.com/drug_interactions.html you need to hit agree and then start typing in your medicines, one at the time. You have several major interactions (I leave the copy-pasted stuff unchanged–they have weird capitalization here and there):
Interactions between your drugs
Major
busPIRone FLUoxetine
Applies to: buspirone, fluoxetine
Using busPIRone together with FLUoxetine can increase the risk of a rare but serious condition called the serotonin syndrome, which may include symptoms such as confusion, hallucination, seizure, extreme changes in blood pressure, increased heart rate, fever, excessive sweating, shivering or shaking, blurred vision, muscle spasm or stiffness, tremor, incoordination, stomach cramp, nausea, vomiting, and diarrhea. Severe cases may result in coma and even death. You should seek immediate medical attention if you experience these symptoms while taking the medications. Talk to your doctor if you have any questions or concerns. Your doctor may already be aware of the risks, but has determined that this is the best course of treatment for you and has taken appropriate precautions and is monitoring you closely for any potential complications. It is important to tell your doctor about all other medications you use, including vitamins and herbs. Do not stop using any medications without first talking to your doctor.
Major
busPIRone traZODone
Applies to: buspirone, trazodone
Using busPIRone together with traZODone can increase the risk of a rare but serious condition called the serotonin syndrome, which may include symptoms such as confusion, hallucination, seizure, extreme changes in blood pressure, increased heart rate, fever, excessive sweating, shivering or shaking, blurred vision, muscle spasm or stiffness, tremor, incoordination, stomach cramp, nausea, vomiting, and diarrhea. Severe cases may result in coma and even death. You should seek immediate medical attention if you experience these symptoms while taking the medications. Talk to your doctor if you have any questions or concerns. Your doctor may already be aware of the risks, but has determined that this is the best course of treatment for you and has taken appropriate precautions and is monitoring you closely for any potential complications. It is important to tell your doctor about all other medications you use, including vitamins and herbs. Do not stop using any medications without first talking to your doctor.
Major
FLUoxetine traZODone
Applies to: fluoxetine, trazodone
Using FLUoxetine together with traZODone can increase the risk of a rare but serious condition called the serotonin syndrome, which may include symptoms such as confusion, hallucination, seizure, extreme changes in blood pressure, increased heart rate, fever, excessive sweating, shivering or shaking, blurred vision, muscle spasm or stiffness, tremor, incoordination, stomach cramp, nausea, vomiting, and diarrhea. Severe cases may result in coma and even death. You should seek immediate medical attention if you experience these symptoms while taking the medications. Talk to your doctor if you have any questions or concerns. Your doctor may already be aware of the risks, but has determined that this is the best course of treatment for you and has taken appropriate precautions and is monitoring you closely for any potential complications. It is important to tell your doctor about all other medications you use, including vitamins and herbs. Do not stop using any medications without first talking to your doctor.
Major
FLUoxetine SUMAtriptan
Applies to: fluoxetine, Imitrex (sumatriptan)
Using FLUoxetine together with SUMAtriptan can increase the risk of a rare but serious condition called the serotonin syndrome, which may include symptoms such as confusion, hallucination, seizure, extreme changes in blood pressure, increased heart rate, fever, excessive sweating, shivering or shaking, blurred vision, muscle spasm or stiffness, tremor, incoordination, stomach cramp, nausea, vomiting, and diarrhea. Severe cases may result in coma and even death. You should seek immediate medical attention if you experience these symptoms while taking the medications. Talk to your doctor if you have any questions or concerns. Your doctor may already be aware of the risks, but has determined that this is the best course of treatment for you and has taken appropriate precautions and is monitoring you closely for any potential complications. It is important to tell your doctor about all other medications you use, including vitamins and herbs. Do not stop using any medications without first talking to your doctor.
Major
traZODone SUMAtriptan
Applies to: trazodone, Imitrex (sumatriptan)
Using traZODone together with SUMAtriptan can increase the risk of a rare but serious condition called the serotonin syndrome, which may include symptoms such as confusion, hallucination, seizure, extreme changes in blood pressure, increased heart rate, fever, excessive sweating, shivering or shaking, blurred vision, muscle spasm or stiffness, tremor, incoordination, stomach cramp, nausea, vomiting, and diarrhea. Severe cases may result in coma and even death. You should seek immediate medical attention if you experience these symptoms while taking the medications. Talk to your doctor if you have any questions or concerns. Your doctor may already be aware of the risks, but has determined that this is the best course of treatment for you and has taken appropriate precautions and is monitoring you closely for any potential complications. It is important to tell your doctor about all other medications you use, including vitamins and herbs. Do not stop using any medications without first talking to your doctor.
And you also have therapeutic duplication:
Therapeutic duplication warnings
Therapeutic duplication is the use of more than one medicine from the same drug category or therapeutic class to treat the same condition. This can be intentional in cases where drugs with similar actions are used together for demonstrated therapeutic benefit. It can also be unintentional in cases where a patient has been treated by more than one doctor, or had prescriptions filled at more than one pharmacy, and can have potentially adverse consequences.
Duplication
Central Nervous System (CNS) Drugs
The recommended maximum number of medicines in the ‘Central Nervous System (CNS) Drugs’ category to be taken concurrently is usually three. Your list includes four medicines belonging to the ‘Central Nervous System (CNS) Drugs’ category:
buspirone
fluoxetine
clonazepam
trazodone
Duplication
Psychotropic agents
Therapeutic duplication
The recommended maximum number of medicines in the ‘psychotropic agents’ category to be taken concurrently is usually three. Your list includes four medicines belonging to the ‘psychotropic agents’ category:
buspirone
fluoxetine
clonazepam
trazodone
Duplication
Antidepressants
Therapeutic duplication
The recommended maximum number of medicines in the ‘antidepressants’ category to be taken concurrently is usually one. Your list includes two medicines belonging to the ‘antidepressants’ category:
fluoxetine
trazodone
Duplication
Tranquilizers
Therapeutic duplication
The recommended maximum number of medicines in the ‘tranquilizers’ category to be taken concurrently is usually one. Your list includes two medicines belonging to the ‘tranquilizers’ category:
buspirone
clonazepam
You are clearly showing signs of serotonin syndrome and I believe you have serotonin syndrome. Please print out all drug interactions and duplication that I included here, head back to the ER on the spot to have them treat you for serotonin syndrome. Once you are out of danger, please join my migraine group here. We work with you to end up medicine free and migraine free completely! Several thousands of migraine sufferers are already completely migraine and medicine free–including me. So join us and we will help you but first you need to take care of your serotonin syndrome.
Hugs,
Angela
Thank you so much. I hope to update later. Needed to feel not so alone in this and this page helped. Thank you so much
Awesome Christina and I saw you also joined our group. 🙂 That a girl. Please be sure to take care of the serotonin syndrome before anything else.
Angela
So I was just at the doctor’s who said I didn’t have Serotonin Syndrome but definitely had too much Serotonin in my system and to stop taking Trazadone. My story:
I’ve been having migraines over the past year (wasn’t sure if that’s what they were, migraine newbie here) and finally decided I needed help. That was last Wednesday. The week before I had accidentally taken too much of my Fluoxetine because they changed it from two 20mg tablets to I’ve 40mg. Guess who took two pills because no one said anything. This girl. A week later I go in for my migraine visit. She made an off hand comment about my Fluoxetine change. I was like, holy crap, I’ve been taking a double dose!
So that night I went back to my normal dose but started Trazadone nightly and Imitrex as needed. Let me tell you, the past couple weeks have just gotten progressively worse. Still getting migraines, nausea and diarrhea, shaking, and loss of balance were a part of life. Finally today I go in because I had to leave work and couldn’t function.
What options are out there for me? My current med list per day is:
Omeprazole 40mg
Buspirone 40mg
Fluoxetine 40mg (accidental 80mg for a week)
Daily vitamin
Trazadone 50mg (stopping immediately)
Imitrex 25mg as needed.
Clonazepam .5mg as needed
Have taken some Tylenol and a little Benadryl.
I’ll talk to my primary care as soon as I can about options. So far this has sucked. Having anxiety, depression, and migraines is such a bad combo.
What I meant to add was that Dr. Koller thought cyproheptadine would be good to try in a small dose to see if I would get some relieve from serotonin. Thank you .
What I am looking at now is the noreprinephrine hormone that maybe contributing
to my bp spikes and other symptoms. Just to note, during the six years on the small dose of paxil I experienced bp spikes at the clinic I worked at and one doc
said that he just did not think that such a low dose of paxil could be causing this problem and maybe I should get pheochromocytoma evaluation and at that time
I also had bouts of kidney stones. Then l had serotonin syndrome which now was over 6 years ago. I’ve always had rt side kidney pain with release. I can not thank you enough for your caring and expertise.
I sure wish that I could meet you and also give you a big hug.!!!!!!
I hope this helps others. Carmita Hugs!!!!!!
Don’t you just love Carmita when doctors say “…just did not think that such a low dose of paxil could be causing this problem…” 🙁 That’s the problem. It was probably caused by Paxil. Kidney stones are no fun and I am not sure how much medicine side effects contributed to that. Drinking more water and eating more salt can do away kidney stones in the future so be sure to stay hydrated with salt and water (not just water). I sure hope you can get some help in figuring out what caused what and how to repair the damage.
Hugs to you for your posts–I am sure it helps many people when someone like you opens up like this with all the problems you experienced. 🙂 Thank you for sharing! <3
Angela
Hi Angela,
I had emailed your site in July. I followed through with by taking a very small dose of cyproheptadine.
It did not stop the release of catacholamines. I do
know now that the circadian rhythm plays a big part
In the hormone release time. The symptoms with this
timed release have not change which are, creepy
sensation,blurred vision,tension,headaches,bp spikes,
sweats,heat,cold,chills,nausea,bowel problems etc.
These symptoms seem to mimic a condition known as phreochromocytoma. I’ve had two 24hr urine test
in 6 years and results were within higher normal.
Therefore,the doctors did not pursue. I have scheduled appts. with an Autonomic Neurologist and
a Nephrologist. Angela, is there anything that you could add that l am not aware of?.
Carmita
Hi Carmita,
I am a bit confused. Cyproheptadine is an antihistamine. I don’t recall recommending that–I don’t recommend medicines. I looked through your posts from July but I don’t see any such discussion. Catecholamines are hormones, rather than histamines, and would not respond to antihistamines. The most well-known and common catecholamines are dopamine, epinephrine, and norepinephrine and these have no histamine connections. Not quite sure how antihistamines would reduce adrenaline-type hormones.
Pheochromocytoma is possibly associated with excessive release of catecholamines in the urine, though it is not an accurate measure–that’s probably while your doctors ignored the outcome. The amount of catecholamines in the urine is also greatly affected by what you eat that day–and potentially the day before the 24-hour urine collection started.
Pheochromocytoma has a host of symptoms with one as hypertension in addition to POTTS-like symptoms, which are changes in blood pressure upon positional change, like from sitting to standing. Your BP would have to drop rather than increase when standing. The symptoms are a long list that each can also represent other things.
I am unsure how serotonin syndrome–which you clearly had–connects to catecholamines, since that is connected to your adrenal gland atop your kidneys. I would recommend getting further tests to discover what you actually have, since at this point your symptoms and the findings based on tests are a bit confused and I could not say what is what. Catecholamines should be checked in the blood to confirm or disprove the earlier urine sample, since that can easily be contaminated by what you eat but the blood test cannot. I would recommend you head in that direction.
Hope this helps,
Angela
Dr. Stanton I need help! My wife is in bad shape. Massive depression, sheer unhappiness. I believe it is the medications that several doctors have prescribed her and they are finally taking their toll on her and I don’t know what to do. I can give you a list but I know she is on 4-5 antidepressants and I believe she has or is quickly developing serotonin syndrome. She started having migraines early this year and that’s where all the prescriptions started flooding in. I need your advice if you are willing to give it. I will list a the ones I know off the top of my head to give you an idea.
Trazodone
Cymbalta
Lexapro
Fluoxetine
Trokendi(Migraine)
Sumatriptan (Injection)
Gabapentin
Any help/advice you could give would be greatly appreciated.
J
Oh no Jay! The drugs you listed have more major interactions than possible. Your wife needs to be taken to a capable doctor (not the one who prescribed all these) but someone to whom you can show the drug interactions I got from drugs.com’s interaction checker–something any doctor or pharmacist can (and should) use. Here are the major interactions (I just copy-paste)–also therapeutic duplication, meaning more than one drug doing the exact same thing. So your wife is major overdosed (the letters capitalized are that way on the page–too much typing to replace):
Interactions between your drugs
Major
FLUoxetine traZODone
Applies to: fluoxetine, trazodone
Using FLUoxetine together with traZODone can increase the risk of a rare but serious condition called the serotonin syndrome, which may include symptoms such as confusion, hallucination, seizure, extreme changes in blood pressure, increased heart rate, fever, excessive sweating, shivering or shaking, blurred vision, muscle spasm or stiffness, tremor, incoordination, stomach cramp, nausea, vomiting, and diarrhea. Severe cases may result in coma and even death. You should seek immediate medical attention if you experience these symptoms while taking the medications. Talk to your doctor if you have any questions or concerns. Your doctor may already be aware of the risks, but has determined that this is the best course of treatment for you and has taken appropriate precautions and is monitoring you closely for any potential complications. It is important to tell your doctor about all other medications you use, including vitamins and herbs. Do not stop using any medications without first talking to your doctor.
Major
SUMAtriptan DULoxetine
Applies to: sumatriptan, Cymbalta (duloxetine)
Using SUMAtriptan together with DULoxetine can increase the risk of a rare but serious condition called the serotonin syndrome, which may include symptoms such as confusion, hallucination, seizure, extreme changes in blood pressure, increased heart rate, fever, excessive sweating, shivering or shaking, blurred vision, muscle spasm or stiffness, tremor, incoordination, stomach cramp, nausea, vomiting, and diarrhea. Severe cases may result in coma and even death. You should seek immediate medical attention if you experience these symptoms while taking the medications. Talk to your doctor if you have any questions or concerns. Your doctor may already be aware of the risks, but has determined that this is the best course of treatment for you and has taken appropriate precautions and is monitoring you closely for any potential complications. It is important to tell your doctor about all other medications you use, including vitamins and herbs. Do not stop using any medications without first talking to your doctor.
Major
SUMAtriptan escitalopram
Applies to: sumatriptan, Lexapro (escitalopram)
Using SUMAtriptan together with escitalopram can increase the risk of a rare but serious condition called the serotonin syndrome, which may include symptoms such as confusion, hallucination, seizure, extreme changes in blood pressure, increased heart rate, fever, excessive sweating, shivering or shaking, blurred vision, muscle spasm or stiffness, tremor, incoordination, stomach cramp, nausea, vomiting, and diarrhea. Severe cases may result in coma and even death. You should seek immediate medical attention if you experience these symptoms while taking the medications. Talk to your doctor if you have any questions or concerns. Your doctor may already be aware of the risks, but has determined that this is the best course of treatment for you and has taken appropriate precautions and is monitoring you closely for any potential complications. It is important to tell your doctor about all other medications you use, including vitamins and herbs. Do not stop using any medications without first talking to your doctor.
Major
traZODone DULoxetine
Applies to: trazodone, Cymbalta (duloxetine)
Using traZODone together with DULoxetine can increase the risk of a rare but serious condition called the serotonin syndrome, which may include symptoms such as confusion, hallucination, seizure, extreme changes in blood pressure, increased heart rate, fever, excessive sweating, shivering or shaking, blurred vision, muscle spasm or stiffness, tremor, incoordination, stomach cramp, nausea, vomiting, and diarrhea. Severe cases may result in coma and even death. You should seek immediate medical attention if you experience these symptoms while taking the medications. Talk to your doctor if you have any questions or concerns. Your doctor may already be aware of the risks, but has determined that this is the best course of treatment for you and has taken appropriate precautions and is monitoring you closely for any potential complications. It is important to tell your doctor about all other medications you use, including vitamins and herbs. Do not stop using any medications without first talking to your doctor.
Major
traZODone escitalopram
Applies to: trazodone, Lexapro (escitalopram)
Using escitalopram together with traZODone can increase the risk of a rare but serious condition called the serotonin syndrome, which may include symptoms such as confusion, hallucination, seizure, extreme changes in blood pressure, increased heart rate, fever, excessive sweating, shivering or shaking, blurred vision, muscle spasm or stiffness, tremor, incoordination, stomach cramp, nausea, vomiting, and diarrhea. Severe cases may result in coma and even death. You should contact your doctor immediately if you experience these symptoms during treatment. In addition, combining these medications can increase the risk of an irregular heart rhythm that may be serious and potentially life-threatening, although it is a relatively rare side effect. You may be more susceptible if you have a heart condition called congenital long QT syndrome, other cardiac diseases, conduction abnormalities, or electrolyte disturbances (for example, magnesium or potassium loss due to severe or prolonged diarrhea or vomiting). Talk to your doctor if you have any questions or concerns. Your doctor may already be aware of the risks, but has determined that this is the best course of treatment for you and has taken appropriate precautions and is monitoring you closely for any potential complications. You should seek immediate medical attention if you develop sudden dizziness, lightheadedness, fainting, shortness of breath, or heart palpitations during treatment with these medications, whether together or alone. It is important to tell your doctor about all other medications you use, including vitamins and herbs. Do not stop using any medications without first talking to your doctor.
Major
traZODone SUMAtriptan
Applies to: trazodone, sumatriptan
Using traZODone together with SUMAtriptan can increase the risk of a rare but serious condition called the serotonin syndrome, which may include symptoms such as confusion, hallucination, seizure, extreme changes in blood pressure, increased heart rate, fever, excessive sweating, shivering or shaking, blurred vision, muscle spasm or stiffness, tremor, incoordination, stomach cramp, nausea, vomiting, and diarrhea. Severe cases may result in coma and even death. You should seek immediate medical attention if you experience these symptoms while taking the medications. Talk to your doctor if you have any questions or concerns. Your doctor may already be aware of the risks, but has determined that this is the best course of treatment for you and has taken appropriate precautions and is monitoring you closely for any potential complications. It is important to tell your doctor about all other medications you use, including vitamins and herbs. Do not stop using any medications without first talking to your doctor.
Major
FLUoxetine DULoxetine
Applies to: fluoxetine, Cymbalta (duloxetine)
Using FLUoxetine together with DULoxetine can increase the risk of a rare but serious condition called the serotonin syndrome, which may include symptoms such as confusion, hallucination, seizure, extreme changes in blood pressure, increased heart rate, fever, excessive sweating, shivering or shaking, blurred vision, muscle spasm or stiffness, tremor, incoordination, stomach cramp, nausea, vomiting, and diarrhea. Severe cases may result in coma and even death. You should seek immediate medical attention if you experience these symptoms while taking the medications. Talk to your doctor if you have any questions or concerns. Your doctor may already be aware of the risks, but has determined that this is the best course of treatment for you and has taken appropriate precautions and is monitoring you closely for any potential complications. It is important to tell your doctor about all other medications you use, including vitamins and herbs. Do not stop using any medications without first talking to your doctor.
Major
FLUoxetine SUMAtriptan
Applies to: fluoxetine, sumatriptan
Using FLUoxetine together with SUMAtriptan can increase the risk of a rare but serious condition called the serotonin syndrome, which may include symptoms such as confusion, hallucination, seizure, extreme changes in blood pressure, increased heart rate, fever, excessive sweating, shivering or shaking, blurred vision, muscle spasm or stiffness, tremor, incoordination, stomach cramp, nausea, vomiting, and diarrhea. Severe cases may result in coma and even death. You should seek immediate medical attention if you experience these symptoms while taking the medications. Talk to your doctor if you have any questions or concerns. Your doctor may already be aware of the risks, but has determined that this is the best course of treatment for you and has taken appropriate precautions and is monitoring you closely for any potential complications. It is important to tell your doctor about all other medications you use, including vitamins and herbs. Do not stop using any medications without first talking to your doctor.
Major
FLUoxetine escitalopram
Applies to: fluoxetine, Lexapro (escitalopram)
Using escitalopram together with FLUoxetine can increase the risk of a rare but serious condition called the serotonin syndrome, which may include symptoms such as confusion, hallucination, seizure, extreme changes in blood pressure, increased heart rate, fever, excessive sweating, shivering or shaking, blurred vision, muscle spasm or stiffness, tremor, incoordination, stomach cramp, nausea, vomiting, and diarrhea. Severe cases may result in coma and even death. You should contact your doctor immediately if you experience these symptoms during treatment. In addition, combining these medications can increase the risk of an irregular heart rhythm that may be serious and potentially life-threatening, although it is a relatively rare side effect. You may be more susceptible if you have a heart condition called congenital long QT syndrome, other cardiac diseases, conduction abnormalities, or electrolyte disturbances (for example, magnesium or potassium loss due to severe or prolonged diarrhea or vomiting). Talk to your doctor if you have any questions or concerns. Your doctor may already be aware of the risks, but has determined that this is the best course of treatment for you and has taken appropriate precautions and is monitoring you closely for any potential complications. You should seek immediate medical attention if you develop sudden dizziness, lightheadedness, fainting, shortness of breath, or heart palpitations during treatment with these medications, whether together or alone. It is important to tell your doctor about all other medications you use, including vitamins and herbs. Do not stop using any medications without first talking to your doctor.
Major
escitalopram DULoxetine
Applies to: Lexapro (escitalopram), Cymbalta (duloxetine)
Using escitalopram together with DULoxetine can increase the risk of a rare but serious condition called the serotonin syndrome, which may include symptoms such as confusion, hallucination, seizure, extreme changes in blood pressure, increased heart rate, fever, excessive sweating, shivering or shaking, blurred vision, muscle spasm or stiffness, tremor, incoordination, stomach cramp, nausea, vomiting, and diarrhea. Severe cases may result in coma and even death. You should seek immediate medical attention if you experience these symptoms while taking the medications. Talk to your doctor if you have any questions or concerns. Your doctor may already be aware of the risks, but has determined that this is the best course of treatment for you and has taken appropriate precautions and is monitoring you closely for any potential complications. It is important to tell your doctor about all other medications you use, including vitamins and herbs. Do not stop using any medications without first talking to your doctor.
Therapeutic duplication warnings
Therapeutic duplication is the use of more than one medicine from the same drug category or therapeutic class to treat the same condition. This can be intentional in cases where drugs with similar actions are used together for demonstrated therapeutic benefit. It can also be unintentional in cases where a patient has been treated by more than one doctor, or had prescriptions filled at more than one pharmacy, and can have potentially adverse consequences.
Therapeutic duplication warnings
Therapeutic duplication is the use of more than one medicine from the same drug category or therapeutic class to treat the same condition. This can be intentional in cases where drugs with similar actions are used together for demonstrated therapeutic benefit. It can also be unintentional in cases where a patient has been treated by more than one doctor, or had prescriptions filled at more than one pharmacy, and can have potentially adverse consequences.
Duplication
Central Nervous System (CNS) Drugs
Therapeutic duplication
The recommended maximum number of medicines in the ‘Central Nervous System (CNS) Drugs’ category to be taken concurrently is usually three. Your list includes six medicines belonging to the ‘Central Nervous System (CNS) Drugs’ category:
trazodone
Cymbalta (duloxetine)
Lexapro (escitalopram)
fluoxetine
Trokendi XR (topiramate)
gabapentin
Note: The benefits of taking this combination of medicines may outweigh any risks associated with therapeutic duplication. This information does not take the place of talking to your doctor. Always check with your healthcare provider to determine if any adjustments to your medications are needed.
Duplication
Psychotropic agents
Therapeutic duplication
The recommended maximum number of medicines in the ‘psychotropic agents’ category to be taken concurrently is usually three. Your list includes four medicines belonging to the ‘psychotropic agents’ category:
trazodone
Cymbalta (duloxetine)
Lexapro (escitalopram)
fluoxetine
Duplication
Antidepressants
Therapeutic duplication
The recommended maximum number of medicines in the ‘antidepressants’ category to be taken concurrently is usually one. Your list includes four medicines belonging to the ‘antidepressants’ category:
trazodone
Cymbalta (duloxetine)
Lexapro (escitalopram)
fluoxetine
Central Nervous System (CNS) Drugs
The recommended maximum number of medicines in the ‘Central Nervous System (CNS) Drugs’ category to be taken concurrently is usually three. Your list includes six medicines belonging to the ‘Central Nervous System (CNS) Drugs’ category:
trazodone
Cymbalta (duloxetine)
Lexapro (escitalopram)
fluoxetine
Trokendi XR (topiramate)
gabapentin
Note: The benefits of taking this combination of medicines may outweigh any risks associated with therapeutic duplication. This information does not take the place of talking to your doctor. Always check with your healthcare provider to determine if any adjustments to your medications are needed.
Duplication
Psychotropic agents
Therapeutic duplication
The recommended maximum number of medicines in the ‘psychotropic agents’ category to be taken concurrently is usually three. Your list includes four medicines belonging to the ‘psychotropic agents’ category:
trazodone
Cymbalta (duloxetine)
Lexapro (escitalopram)
fluoxetine
Duplication
Antidepressants
Therapeutic duplication
The recommended maximum number of medicines in the ‘antidepressants’ category to be taken concurrently is usually one. Your list includes four medicines belonging to the ‘antidepressants’ category:
trazodone
Cymbalta (duloxetine)
Lexapro (escitalopram)
fluoxetine
Jay, please note that every single drug she takes in combination of just 2 can cause serotonin syndrome. Please print this out, together with the link to the website I got this information from, take her to the ER or to her doctor tomorrow the latest and have them look to see what must go immediately. I have a migraine group that she should join where thousands of migraine sufferers learn what causes migraine by reading my book and then they learn how to apply a protocol I created. They all become migraine and medicine free. It is free.
Best wishes,
Angela
Thank you for bringing this issue forward. When my husband died suddenly 16 yrs. ago, I developed a panic disorder and depression. A psychiatrist put me on 200 mg of Zoloft, which he assured me was like “taking a vitamin everyday.” He said I could stay on it forever. 200 mg. Today, I weigh 110 lbs., am 65 yrs. old and have had cancer twice. Three years ago, I had a severe seizure and developed, in only a few hours, complete muscle rigidity and horrible twitching in my legs which actually looked like a bag of worms. The paramedics took me to the hospital, even though they dismissed me as a “drug addict” having a bad reaction. I could not even tell them what was wrong I was in such horrific pain. It happened again a month later, but this time I almost died after being left in the ER for several hours with no treatment. I have told every doctor I’ve ever seen that I take 200 mg of Zoloft. After these two incidents, I began seeing neurologists to find out what was happening to me. I cannot even tell you the amount of money I have spent looking for answers. I was diagnosed with Stiff Person Syndrome and I cannot walk anymore unless I use a cane and I have horrible pain and twitching still in my legs. I was dismissed by every neurologist. For the past year I have been suffering from uncontrolled diarrhea. Last week I visited an endochronologist to get an endoscopy and colonoscopy to see what is going on. The very first thing she said when she looked at my chart is you have serotonin poisoning. Now that I have been researching it, yes, that’s what happened. I have reduced my dose now by half and will try to reduce it another half in a few months. My life is pretty much ruined but I am so glad that people like you are getting this out there.
Oh wow Luci! I cried reading your message. What a horrific story. I am glad you are alive and admire your strength! I would like to boost you onward to recovery! Your life may not be ruined at all. I am the same age as you are and started weight lifting and kickboxing this year to improve my body and strength and the changes are amazing. I also changed my nutrition from the carbohydrate-based nutrition to the ketogenic–this happened 4 years ago–and for the past 6 months to keto carnivore (don’t eat any veggies and fruits either). These steps I took have reversed my aging process completely and I made a full recovery in many health conditions I had.
One of the best things about the ketogenic diet is that it heals the brain and it also health the body.
Back to Zoloft: I blame the first doctor who prescribed Zoloft to you for the acute depression you suffered from the death of your husband. Antidepressants are only supposed to be prescribed for chronic depression of no known cause. This is the important part: depression with no know cause. Under any other circumstances working with a therapist to help you over your sock would have been the way to go. I hope that you can completely come off of Zoloft in time–it takes time and know-how in titrating off without discomfort. Sounds like you now have a good endocrinologist to guide you so please seek out her help.
Best wishes,
Angela
Six years ago I had severe serotonin syndrome caused by my being on 5mg dose of Paxil for 5+ years prior. Since then to this day I am daily fighting the after-effects. My sensations are a continual flow of catacholomines that rush through my body that cause heat or cold, spikes in blood pressure , tension, and fight or flight symptoms. I was originally put on Paxil for early menopause which was giving me some anxiety, not depression, never depression. I am 60 years old now. I struggled on Paxil from day 1 but I stayed on it because the doctors insisted that 5mg would not have that effect on me.After I finally got my genetics tested, I found that I was an intermediate metabolizer with the cyp2d6 enzyme. I have had all types of medical testing done and still don’t know what could be the cause of the constant releasing of these hormones. I don’t tolerate any medicines. Could I be sensitive to my own serotonin? I am a retired nurse now. I haven’t been able to work for the last 6 years. Does anyone understand where I can go from here?
Dear Carmita,
You are very correct. Paxil, as an SSRI, has absolutely nothing to do with anxiety. What you should have received is benzodiazepines (preferably a very low dose Diazepam as needed max once daily). Unfortunately SSRIs can do a lot of permanent damage, particularly for those whose drug metabolism is faster or slower than what the drug expects, because you get overdosed. I am a fast metabolizer and metabolize all medicines really fast such that they have no effect on the problem they should help but I get very sick from them. I got to the point of not even takign simple OTC medicines for anything, knowing how bad they are for those of us with the CYP2D6 enzyme variant.
I don’t think you are sensitive to your own serotonin but I think that Paxil’s reuptake inhibitors damaged some of your neurons (maybe all) that are now in perpetual serotonin production. Ask your doctor to test a very low dose serotonin blocker medicine–this blocks the production, as opposed to SSRIs that block the production-inhibition. So SSRIs force the neurons to produce serotonin all the time nonstop and my suspicion is that by the very nature of these inhibitors modifying the protein of the reuptake inhibitors, they can damage it, often for life.
You may find a very low dose serotonin blocker may work. It is important to note that only 10% of serotonin is used by the brain and 90% by your intestines, so if you were allergic to your own serotonin, you would have diarrhea all the time. This is an important distinguishing factor.
I wish you well,
Angela
Angela, I am so glad that you brought up the diarhea. I had chronic diarhea during the 6 years I was on Paxil.I had 2 colonoscopies during that time; they found nothing.I am now seeing a gasterenterologist for gut and bowel problems. I am on 15mg Lopressor for help with blood pressure spikes. Could norepinephrine also be involved? Are there any natural serotonin blockers that I could explore? As you know, most everything goes through the cyp2d6.
I work very hard everyday on this and at this point, any small improvement in my suffering is welcome. I still have a calmness in me and I smile whenever I can.
I have no depression and no panic attacks, just this continual drip. Could ptsd be a contributing factor? Thank you. I appreciate your kindness and support.
Carmita
Oh wow Carmita! And no doctor ever even questioned the role of Paxil in all of your troubles and here you are in one chat you have an answer. 🙁 So shameful for our medical system! So very sorry for what you are going through. There are medication that block serotonin production; one is cyproheptadine. Since I am not an MD and don;t prescribe anything, I am not familiar with what is most commonly used–I am only familiar with this one medicine for that. Not sure about natural serotonin blockers–just quickly googled that and it brought up a few things I would not recommend you take.
Norinephrine is for blood pressure control. Your blood pressure spikes are likely the result of the serotonin syndrome as well–that is one of the most typical symptoms of serotonin syndrome.
It seems to me that your troubles are connected to the long ago taken Paxil. 🙁
PTSD is a very serious condition that can easily convert into brain damage. It is definitely something to be looked at and taken care of. I am not sure how it may contribute to your current status. It is good that you feel an inner calm but I am suggesting that inner calm can also mask things, such as damage from PTSD. Please take care of your well-being in mind as well as brain and body.
I hope things can be sorted out for you soon!
Hugs,
Angela
Angela, I want to keep things brief yet still get my points across.I have been with my neuro psych doctor for 6 years now. He diagnosed me with serotonin syndrome at that time.3 years ago he also diagnosed me with ptsd. My case was addressed in a national psychiactric conference.I have always known that my special case has been medical, just like you knew that your mother had serotonin syndrome. All professional medical doctors that I have seen, could not put 2 and 2 together. They want to make you comfortable but not get into finding the actual cause of my symptoms. They say that they truly do not know.I agree with you that my ptsd is not associated with the aftermath of the serotonin syndrome.The calm and smiles that I have expressed,to answer you, is the hope that I have always had within me as part of my personality.It has helped me immensely during this harsh trial. I feel so blessed to have talked with you because truth has always been the most important factor in my life. I will continue on my journey and I have the most love for you and your mother. I hope this helps others in memory of your mom.
Hugs,
Carmita
Thanks Carmita,
Your comments brought tears to my eyes. Best wishes for your recovery and much love,
Angela
I also have PTSD, check all your related medications for that as well! My issues started out as GI issues which then lead to more medications that contributed to the issue to be prescribed, which then lead to my gallbladder requiring emergency surgery. In one year I had small issues creep up in addition to the GI issues, migraines, TMJ, increased anxiety and insomnia, etc. Each new drug prescribed to address these symptoms is now known to contribute to toxicity! I had 16 active medications by the time I was admitted for the emergency surgery and the hospital observed me having major symptoms, muscles jerking, blood pressure, temp variations, confusion, and still it was never assessed. They did check to see if I possibly had a stroke, I hadn’t, then wrote it off as an anxiety attack!
Best of luck to you!
Hello, I am a new poster on this site. I am so relieved to have found it (while searching everywhere on line that I could find on possible serotonin effects from a dietary supplement). I will provide a better introduction and history of my Serotonin Syndrome experience. But for now PLEASE TELL ME WHERE TO get the detailed genetic testing done that you recommend. Where do start?? THANK YOU!
Dee
Dear Dee,
I am glad you found this site. 🙂
In terms of genetic testing, there are many companies that specialize in genetic testing, such as 23andMe or Ancestry–of course, to understand the information, you are better off hiring a company like Futura or visit a Functional Medicine doctor and ask for their services. I am a bit versed in genetics and started off with LiveWello for generating my initial analysis and then I discovered Promethease. I recommend Promethease the most. It is inexpensive–you do need either 23andMe or Ancestry genetics raw data (or both–fun!! It shows you conflicting findings if any!), which it then analyses.
Genetic testing tells you your predispositions only. It will not “diagnose” or suggests that you actually have some health condition or disease. It cannot, since many forces need to act upon a genetic variant to have the “switch” turn it on and make it functionally different from what it would have been otherwise. For example, I know many people who have the MTHFR variant, suggesting that they may have a problem with B9 methylation, but then checking a blood test (homocysteine) we find out that they have no problems at all. In other words, just because your genes have a variant, it doesn’t mean you have the associated condition. Other genes, not considered, are also affecting the variant and so you may or may not have any issues.
Hope this helps!
Best wishes,
Angela
I know absolutely that I bounced around the serotonin toxicity spectrum for YEARS! That it was missed 4 times when I was at the high end of moderate/borderline severe evem, and each of these times I was in the hospital with the exception of one, which I did seek care for at my doctor’s office and was told it was an allergic reaction! I was prescribed 16 medications last year alone that now are known to contribute to serotonin toxicity, most to band aid the symptoms I now know to have been caused by the serotonin toxicity. The last few were used to treat me during emergency gallbladder removal, which I also believe to be caused by the toxicity because my gallbladder failed due to dysfunction of my sphincter of oddi, a smooth muscle in the GI track, the first muscles to generally express physical symptoms due to toxicity. This issue was confirmed back in 2011/12! I vomited daily for two years, resulting in the need for total dental restoration at the cost of over $15,000! I’m a shell of the woman I once was. I lost so much weight, my health, and my sanity almost in the end. I’m only in my 30s so was often told it was “anxiety” or “in my head”. Is there a way I can contact you to provide all the details to see what you think?
It scares and sickens me that this can happen to anyone! I’m extremely careful with medications, only taking when absolutely necessary and it still happened to me, for years!!
I’m so sorry to hear of your mother’s story, and the fact that nobody listened to you when clearly you do understand clinically!
Thanks Ammalyn. Indeed, doctors are either not taught the symptoms or are just purely ignorant. I cannot tell what is making doctors so blind to this. Clearly a change is needed. The best thing we can do is to not accept any medicines but seek out the cause of the condition. I find that a very large percentage of our ailments today are caused by our foods and their lack of nutrients. Unfortunately it takes the body years to recover!!! I have changed my entire lifestyle over 6 years ago and while over 90% of my problems already vanished, this week I started noticing new hair growth!! It is now about an inch long and it started to show up–it is also different color from my natural hair!! Go figure. It can take over 6 years for your body to totally revamp itself and change everything.
So the proper nutrition (no grains, no sugar, no simple carbs of any kind, no processed foods, no juices, no shakes or smoothies, no vegetable oils–and in my case also no fruits or vegetables at all) can make the body completely recover.
I wish you good luck!
Angela
I suggest a better and less costly service to analyze your SNPs:
https://www.dnatoz.com
I have been on 60mg Fluoxetine an 120 oxcycontin er for years, I tried to lower dose of fluoxetine and have been going thru hell since, My primary care doctor who gives me these meds thinks there is no connection with my symptoms which are severe anxiety, panic attacks with uncontol crying also aches and headaches. I have been to emergency room. they say see my primary. i now am waiting to see a phyciatrist but not till Oct 1.I feel like i cannot wait till then. every day i take the fluoxetine i feel like im taking poison. I do take low dose of valium that helps but very little.
Teresa,
What you eat matters a ton in how you feel. I work with a lot of migraineurs and they all are taking a ton of meds, some including Fluoxetine (Prozac). It is much easier to come off of it slowly if you change your diet such that your body becomes healthy. Eating a lot of processed foods, simple carbs, lots of grains, and even sugar substitutes, cause a lot of health problems for your body and then you cannot expect your body to “help” you in what you want to achieve. Medicines don;t make anyone healthy–they just cover up symptoms. Food is medicine so use it as such.
Best wishes,
Angela
I would like to get off some meds, I have Lupus. I was interested in genetic testing.Im sorry my first text wasnt clear. Its hard for me to explain my symptoms. I would like to hear what you think of the combination and amount of meds im taking re the serotonin syndrome. Thank you.
Hi Teresa,
I am not able to advise you but here is what I would do if I were you. There is a drug interaction checker here that you should put all your medicines in–as you start typing the name, choices appear and hit “add” and then the next and once all added, hit “check interactions”. It places the warnings into several groups for you:
Major interaction: immediately head to your doctor and have her/him to “remove or modify” such that you have no interactions
Moderate: on your next doctor’s visit show the interactions to your doctor and ask for “remove or modify”
Minor: no action needed
Therapeutic Duplication: when you are taking more than 1 medicine to reach the same outcome, like taking more than one antidepressants.
It usually also brings up interactions with foods–like grapefruit can cause trouble for the clearance of medications and thus can overdose your meds, so for most medicines, eating or drinking grapefruit is a no no.
Be sure to print out your interactions as you are heading to your doctor so she/he can read an official interaction that can be checked by the doctor and pharmacist as well.
In terms of lupus: it is an autoimmune disease made of inflammation as a result of eating foods your body finds inflammatory. Such foods are: grains, sweeteners, starches, fruits and vegetable juices, smoothies, and shakes. In some cases once you quit all of the above, you may find that you completely recover from all your ailments. If not, also remove eggs and dairy and add one at the time back a week apart after 2 weeks of absence. Grains need to be quit for a minimum 3 months to see any change–they cause so much damage that healing to the point of your discovery is that slow.
Best wishes,
Angela
Isn’t 5mg of Paxil a very low dose? I think the smallest pill you can get is 10mg, so she had to be cutting that in half. I take 10mg Paxil everyday, along with Xanax, for anxiety. I don’t have signs of serotonin disorder but noticed that I got awfully grumpy when I started taking Turmeric for pain issues. Turmeric can also raise your serotonin levels so I had to quit. Too bad as it did seem to work.
Hi Peggy,
Yes, 10 mg is the smallest dose. Some people use compound pharmacies to get smaller doses of medicines, so perhaps that’s the case here.
Turmeric interacts with many medicines. In general, if one takes Western Medicine, I recommend to not mix that with Eastern Medicine. Interactions are highly likely. While turmeric is a spice, it is also an herb used in Eastern Medicine.
Paxil is an extremely powerful SSRI with half-life of 21 hours (that means half of the drug is eliminated from the body in 21 hours) but there are some genetic variants that can accelerate the drug or slow it down so it can create trouble based on the body’s ability to metabolize it. Some genotypes, for example migraineurs, seems to have a hard time with many of these drugs in that they absorb very quickly, causing a fast overdose and then they leave the body very fast as well, causing withdrawal. For people like that, many medications should not be used because the initial fast absorption (for super metabolizers) can seriously overdose.
Doctors really should check genetic variants of the CYPxxx genes where xxx has many different variations, like CYP1A2 or CYP2C19, etc., to see if the patient about to be prescribed a drug will become sick from it or the drug will not work at all.
Best wishes,
Angela
Thank you for this informative article. I am sorry for the loss of your mother. I recently had Serotonin Syndrome that fortunately my PCP mentioned. I missed it even though I am a psychiatric nurse. Mine started with a combination of Fentanyl, Zofran, and Prozac. I have severe nerve damage in my spine, so when I became hyper reflexive with clonus, they thought it was my spine. Then I lost my balance and fell frequently so they thought it was MS. Diaphoresis was ticked off as menopause, and increased anxiety, confusion and sleep disturbances was thought to be part of a grief reaction after losing both my parents. My hypertension was out of control and I had episodes of auditory hallucinations. Also scatoma from my ocular migraines. You can hear the zebra hooves running to each specialist I saw.
I stopped all the meds except my Fentanyl and it took me over a year before I could ambulated without a cane at 57 y/o. Recently I was put on a low dose of Prozac and the symptoms started returning. So off the Prozac I go and have been educating all my doctors from my hematologist to my neurologist regarding this insidious syndrome.
Dear Lea,
Thank you so much for your highly informative and educational comment! I think everyone should read what you wrote. I am glad you are with us and recovery is not out of the question. I am very sorry about the death of your parents and your feelings are totally within expected.
I had a major back injury in 2011 or 2012 with 3 vertebrae blown out by an exploding cysts. My left side was paralyzed for two months (in wheelchair) and slept set in a chair because I could not get flat no matter how hard I tried. Even the physical therapist sent me away when my doctor signed me up saying “it is too soon”… My surgeon was sharpening her knife but I took over and with the same endurance as I got my doctorate, I educated myself about the spine. Today, at age 65, I lift weights for fun (at 110 lbs now) and do kickboxing for a bit of heart movement… My surgeon doesn’t believe how my back recovered. So don;t give up!! Read up on back issues, do exercises, such as tilt table, 90-90 and similar (I used to put a triangle pillow under my butt to give a slight incline and also support for my neck. Lying down on a 36-inch foam roll lengthwise helped straighten my back as well by relaxing all the muscles around it. I used to do these several times per week and the end-result was a completely healed back.
Try these if your PT or doctor supports them–my PT was the one who recommended them and wow!
In terms of any SSRI, SNRI, or any serotonin medicine: you will not be able to ever take them again. I would recommend you place serotonin on your allergy list and leave it there for life–I did!
I wish you the best of luck and hopefully you can help on your nerve damage to make life more tolerable. <3
Best wishes,
Angela
Is it likely that a case of “mild” serotonin syndrome could persist weeks (or indefinitely) untreated? A young PCP was seeking to avoid increasing my mother’s chronic pain meds. Instead, he increased Cymbalta from 30 mg 1 day, to 2x per day and concurrently added Trazodone 50 mg at night. Within 48 hrs she became manic and agitated which she’s never been before. The Cymbalta and trazodone were stopped (she’s D/c’d Cymbalta cold before without any detectable issues) but nearly 3 weeks later she’s still manic. MD refuses to add any antagonist drugs or sedatives. Tough to get another MD in a semi-acute situation for a nursing home resident.
Dear J,
I suppose it is more likely that some damage occurred from the serotonin in your mom’s brain such that the reuptake inhibition became permanent and your mom’s brain (perhaps) is “stuck” in much more serotonin-release mode than it should be. I would think that it would be good to test an antagonist. What kind of MD is in the nursing home who refuses to even try? I would recommend that you contact your state’s Board of Medicine and seek advice on how to force the MD to evaluate.
My gut feeling is that he may not want to test the antagonist because testing would be an admission of his earlier mistake. If he did make a mistake earlier (it seems he did), and the antagonist would work, that would be more than admission. That woudl be proof. I think (again, just a gut feel) that you are up against an ego.
I wish you best of luck in your search on how to get him to test an antagonist!! <3
Hugs,
Angela
Thank you, Angela. Yes, he said he won’t write any sedating medication until he knows the etiology, and was waving primarily psych diagnosis around. Obviously, it’s more than a coincidence she becomes manic 48 hours after Cymbalta doubled, and trazodone was added. The infuriating thing is that this is an outside private Cedars Sinai Md that found because I thought we’d get better outcomes. He’s very young only in practice less than 5 years and I agree it’s pure ego at my mother’s expense. I have to get him to bow out of his own volition otherwise I’ll have a tantrum from mom. I can’t do that for 2 weeks because he’s on vacation. What a mess.
What a terrible situation J. I am not even sure that this MD knows what he is doing since a serotonin blocker is anything but a sedating medicine. What is he thinking of? It was a doctor like this doctor who doomed my mother too–2 of them actually in two different locations. I would go ahead and report the incidence to the Board of Medicine and ask for advice and perhaps you can replace him with a different doctor in the meantime.
Best of luck!
Angela
I no longer trust doctors. As far as I’m concerned, MD stands for Massive Dickhead. I’m not here to talk about my experiences, but I am here to talk about the ease with which doctors prescribe medication. When I asked to be put on zoloft, the doctor blithely prescribed alprazolam without asking me a single question about addiction, was I currently taking any meds for anxiety, etc. Not to mention that I’d have to go through withdrawal…
This relates to trying to tell the doctors about your mom’s serotonin levels and being ignored. Because if the doctors didn’t think about it, it can’t be true. I could go on. But not here. Thank you for posting this. It made a difference to me to hear from somebody who once again knows what they’re talking about and faces a sea of opposition whilst a loved one fades in front of you.
Thank you Johannes for your comment. Indeed, I support your distrust of doctors. There are good doctors too, honest ones who really try to help you, only even they have their hands tied by the medical institution they work for and what they have learned in their medical school! And what they learn in medical schools today is already outdated by about 30 years so I am not surprised at all.
We the patients must learn enough medicine to understand what’s going on and what to do about it.
Best wishes to your recovery,
Angela
Thank you for highlighting the dangers of serotonin syndrome. I, too, suffered through acute SS several years ago as a result of a protocol that used Frova as a mini-prophylaxis for menstrual migraine. This was the only serotonin-altering drug I was taking at the time, and I dosed it exactly as recommended by my neurologist. I was desperate for migraine relief.
A couple of days into the protocol, I began experiencing severe stomach pain, blue nail beds, and severe shivering. At first I thought I had a GI virus. I spent hours covered in blankets, and then the elevated body temperature began along with the myoclonic movements in my legs. Somewhere in the fog, I suspected I may have SS and asked my husband to get my laptop (I’m a nurse practitioner). I confirmed it- it was the Frova. Eventually the slamming headache kicked in, and I had to seek help.
Every doctor tried to tell me I had the flu and that I couldn’t possibly have SS as a result of only taking Frova. Not one doctor would hear it. There are now cases like mine out there in the literature, but I’m not sure they are given much thought. To write so many scripts and then want to hear nothing of the ramifications of those scripts is simply negligent. Thank you for sharing your story.
Dear Erica,
Very sorry to hear how you had to fight. Indeed, it is negligence–or worse! On one of my private blogs I have just received a comment from a nurse practitioner (they are equivalent to MDs only no residency) on an article I wrote there on SSRIs and their difference from benzodiazepines. She has a similar experience to you in terms of ignorance and is also explaining the influence of big pharma on why these drugs are prescribed.
Unfortunately the doctors will not do any better until big pharma power is strong and the patients don;t self-educate, like you do now.
Hope for your quick recovery!
Best wishes,
Angela
I am on my 6th anxiety medication. I was on Lexapro, buspar, paxil, celaxa and trinquilfity and now back on Lexapro. I did not ween off of the meds, I just went from one to another per my psychiatrist. I was on Paxil for only 3 months and then switched to something else as I did not like it. My head now feels heavy and it cracks all the time, I have a tingling sensation through out my body and my bones hurt, I sweat at night but not real heavy. I never had these feelings from the other medicationd until I used Paxil as my therapist recommended it. I’m trying to figure out what is wrong with me and if these feelings will ever go away. All I really want is my life back. I am wondering if I should go see a Neurologist to see if they can figure out what is wrong with me. My GP told me to deal with the tingling if the medication is working.
Dear Carol,
Thanks for your comment. What you are experiencing are brain zaps I believe. I have heard of others having the same if they come off these medicines very fast–it is also listed as an adverse reaction when the medicines are not tapered off properly. It is particularly common with Lexapro. If I were you, I would also ask to have me checked for serotonin syndrome because some of your symptoms are borderline hinting at that to me.
I must add that not one of the medicines in your list is for anxiety. These are all serotonergic pathway medication, and don’t touch the dopanergic pathway, which is what you need in order to control your anxiety. Most doctors, for some odd reason, prescribe antidepressants for anxiety–although I am 100% sure they know the difference (at least I would hope they know the difference). Here is an article I wrote on the difference of these two drug classes. The only true anxiety medicines are the family of benzodiazepines. However, because of the many doctors who prescribed (and still do) these meds wrong, they caused extreme addiction and there is a general fear-cloud encircling them. As a result, it is hard to get a therapist/neurologist to agree to prescribing a long-acting benzodiazepine for your anxiety, such as Valium (diazepam) or Klonopin (clonazepam). I also wrote an article on short-acting versus long-acting benzodiazepines that you find here, which explains why the short-acting ones (such as Ativan (lorazepam) should never ever be prescribed to anyone, though that is usually what ends up being prescribed.
If your doctor is willing to entertain a change, please have her/him consider prescribing Valium in a very low dose–therapeutic dose is 5 mg and smallest dose is 2 mg. The half-life (the time which it takes to clear 50% of the medicine out of your system) is 26-50 hours!! That is HOURS so more than one day!! So please don’t take it more than once a day maximum!! If I were prescribing this, I would prescribe the lowest dose once every 2 days.
And don’t just quit Lexapro please!!! It takes quite a bit of slow taper. The tapering schedule prescribed by the pharmaceutical company is way too fast and guarantees that your will go back on Lexapro. So talk to your doctor and ask for a slower titration schedule.
Best wishes,
Angela
I am the un-named person that Angela notes in her much earlier comment had an MI with a resultant stent seven years ago but tested with clear arteries recently. Angela has extraordinary understanding of the neurobiology involved. None of my many medical personnel including at the teaching hospital had any real understanding why a very healthy, physically fit adult with NO family cardiac history and low BP and low cholesterol would have an MI or clogged arteries. Second opinions from everyone and the response was: “keep doing what you are doing”. That might have killed me without the homocysteine understanding……Thanks once again Angela for your bravery.
Thanks Bart for your comment! I truly appreciate your speaking up! And I am very happy that fate brought you into my life and we could figure things out to try to “right a wrong” as much as possible. 🙂
Angela
My name is Katherine,
I managed to survive serotonin syndrome while borderline going into cardiac arrest and seizure because I self-diagnosed and stuttered it to the paramedics and newly resident doctor.
I am a 28 year old female who had the misfortune to have a severe head trauma while working as a Community Support Worker. The head injury led to my loss of being able to work and I developed from post-Concussion syndrome to Fibromyalgia.
My GP did all she could to try and treat my pain while I was waiting a year to be accepted into a pain clinic. She ended up prescribing 120mg Cymbalta (SSRI) and 400mg Lyrica (Pre-Gabalin) based on academic evidence to try an combat the opioid pain medication (Hydromorphone by this point) and anti-inflammatories (Naproxen) I needed just to function and move.
Once in the Pain Clinic, I let them know ALL the medications I was on AND the dosages. The Anesthesiologist ended prescribing 2mg Amitriptyline and 2mg Ambilify on top of what I was already taking. I could tell something was off after a couple of days but I was waved off as it was within normal side effects.
I ended up being out of province, visiting family, when I really started to get the symptoms after 2 weeks of this new medication added on. It happened really fast from when I first thought what it might be to a full on attack. I have a degree in Psychology and Biology, and I just barely remembered a single class that mentioned the signs, symptoms, and resulting aftermath of Serotonin Toxicity (Syndrome).
I called my doctor to try and get advice but could only leave a message. A couple hours later I got a message from her telling me to go to the hospital immediately if I had any of the symptoms. Two hours later I was in tachycardia with 150 beats per min, really high blood pressure for me at 160/100, was severely stuttering and slurring my words, I had multiple hallucinations, and had little motor control. I barely managed to get my mom to call an ambulance. I barely told the paramedics what it was. I barely stuttered to a newly resident doctor, ” Serotonin Syndrome, benzodiazepine please?” I knew I would die otherwise if she said no.
I was very lucky that the young doctor believed and weighed my answer to be right enough to give me clonazepam. Within the hour I could talk more normally and my heart rate/blood pressure were more normal.
I then was taken off all Serotonin and those last two new drugs. I proceeded to go through terrible withdrawals for 3 weeks. Even now I am trying to get off of Lyrica, as I feel it too is not helping me.
I’m still waiting to talk to my Anesthesiologist about what happened with what she prescribed. I most likely will give her another chance to help me.
My message is this: Always look up your symptoms when your gut tells you something is wrong. Never trust your doctors to always make the right decisions when prescribing medication. They may fuck up and it is YOU they fuck over with their mistakes.
Stay Alive.
Sincerely,
Katherine S
Wow Katherine! I shared a few tears with you. What amazing story and courage you ave! Indeed, we all must self educate before we visit our doctor! It is a sad state of affairs to have to do that and not trust our own doctors, our hospital doctors, and not even the emergency room doctors–also nurses. Unfortunately they are also learning the same bad information that our doctors learn and are not trained to recognize symptoms.
I never forget what one doctor told to one of my clients, and I think this is representative of our healthcare. It was about a test the doctor refused to order, but which can be ordered by the patient in the US via online services, such as Request-A-Test and others. The test results came back completely normal and so my client didn’t need the medicine the doctor wanted to prescribe. This was his response upon seeing the test–this is paraphrased and not a direct quote:
“I don’t know what that means and I don’t need to know what that means for prescribing medicines!”
And the doctor went ahead and prescribed the medicine to my clients, who promptly trashes it (I wish that happened in front of the doctor but it didn’t). I personally have trashed medicine in front of the doctor in ER when I was given a drug I didn’t need. Shamefully, some doctors request a signature from the patent that they have refused the recommended medicine to cover their backs. This shows that we live in a pharmaceutical-state where medicines rule over healthcare, even at the price of the health–or life–of the patient.
Glad you are alive and with us! <3
I run a fibromyalgia group. It appears that fibro is hyperactivity of the “touch” sensory nerves, which is initiated in the CNS. While not close to what migraine is by its symptoms, it seems to be similar in cause–in terms of hyperactivation of sensory nerves–only in migraine different sensory nerves. Given that your fibro started after injury, it is likely the result of a damaged brain area responsible for touch sensory neurons activity and they are in hyper drive. Migraine-brain is in hypersensory mode and responds very well to a treatment I have been specializing in for the past almost ten years,and on Facebook almost 5 years. It is a very successful and completely free program; also free from medicines. You may find it benefits you. If you woudl like to try it, please join the small fibro group here or the large migraine group here. We may be able to help you heal your brain.
Many hugs to you!
Angela
Can you please email me? No one will listen to me and this is very important. I am scared and a mother of a young child. I know for a fact I suffered seratonin syndrome and have been put back on seratonin drugs. Everyone around me is convinced my symptoms were just that of anxiety and I swear they are not. Would love to email you my story and get some much needed advice.
Dear BB,
Thanks for your comment. I am a scientist blogger on this website and don’t take private emails–I have several thousand people I work with in several FB groups. It would be impossible for me to get emails from thousands of people who read my posts and would like to share their stories with me. There is only one me and so that is impossible. However, HormonesMatter is always looking for stories told my those who are suffering. I would recommend you write it up as a story and send it to the site owner under info@hormonesmatter.com and the site owner will publish that. Or, alternatively, you could just post it as a comment–like the comment you just made–and it will publish that way and I can respond to that. The best way to recover from serotonin syndrome is by stopping the serotonin medicine(s). If you feel it is causing you serotonin syndrome–which is entirely possible–you need to reduce and then quit that medicine. I don’t know why you are taking serotonin medicine, so the reason would also be helpful. Many people who receive serotonin medicines gain no benefit from them. Also, there is no such law or regulation that you must follow your doctor’s orders of a prescription. So you have choices.
Looking forward to reading your story either as a comment or as a story on this blog.
Best wishes,
Angela
I had this happen to me I was prescribed Zoloft and trazadone and had every symptom and my pcp made me feel stupid and told me I didn’t have it and said it was anxiety I had every symptom of seratonin syndrome and was laughingly dismissed and now a year later I have hand and voice tremors, insomnia ,depression and much declined cognitive and moter skills with no resolve
Very sorry to hear Cathy. I hope you are not on any serotonin medication now. Are you?
Angela
Thank you Angela, no I am not, I am on clonmazapan .25 was .50 but I take less due to poor cognitive and motor skills, I am very depresed I have a Bachelors degree and had a great job and fell on ice and had hip.arthoscopy and still have intermittent groin pain, a torn meniscus and extreme deep buttock pain fron si joint dysfunction, my pcp has been great for 15 years but obviously injury and knowledge of medicine interactions are not her forte, she told me I could keep taking imitrix with 325 norco 500 robaxin and the Zoloft and trazadone, I have IBS so rarely took norco, I took Motrin a lot with robaxin and then when cognitive issues began stopped robaxin and took meloxican, just had a neuropsych exam and scored very low, the medicines have ruined my mind and I have unresolved tinnitus, my life went from great to miserable can I get my brain to work again? Had to beg for cortisol adrenalin advanced tosh as my hair and eyelashes are falling out, I have insomnia and what she calls anxiety hand , right arm and speech tremors any advice I just want my life back please
Oh dear Cathy, you sure had your share of terrible experiences! 🙁 I think that you are on the right track. Meloxicam is an excellent NSAID–I had a major back injury about 7-8 years ago and lost sensation on my left side for 2 months completely, so I was in a wheelchair. I used Meloxicam then and found it better than anything with narcotics in it. I quit it as soon as I could. My back is completely recovered now and I lift weights (power lift) and kickbox for fun and to keep my back in good shape. It is possible to recover from anything–at least that is my attitude! Clonazepam is a good benzodiazepines class medicine–just be sure to take it max once a day because it has a very long half-life (the time it takes for half of the medicine to leave your body). Its half-life is 26-50 hours depending on certain genetic metabolic factors.
Depending on your age, you can make a complete recovery or partial if you set your mind to it. You would have to find a doctor who is familiar with the modern nutritional approaches and fasting for health. As difficult as it is to believe, fasting two or more days can completely revamp your immune system and can start also a process in which your body gets rid of cells that are not functioning right and either replaces them with new ones or repairs them. It is a great way of being in general but it requires a lifestyle change and a good healthcare provider who knows what you need and can help you get that service.
I hope you can find a doctor who can help you with that! <3
Best wishes,
Angela
hi, i hope you can help, im 46 years old and iv recently been discharged from hospital after a heart attack, i was given an angiogram which was clear, i then had a echocardiogram which showed lv systolic impairment, post/lateral hypokinesis, they have said they arnt sure why i have these results so i need to have an mri scan. during my initial examination i was asked about my medication, i told them that for approximately 6 years iv been taking tramadol, fluoxetine and lansoprazole. i was then immediately taken off the tramadol and told it can cause serotonin syndrome which id never heard of, i then began to read online articles regarding serotonin syndrome and side affects to which iv had a number of over the years (Irregular heartbeat,Heavy cold sweating, Diarrhea, dizzy spells and blurred vison. i have visited my local doctor several times over the years regarding these symptoms and given ECG tests but nothing showed up so no diagnosis was ever made so i have just lived with it since. i am now curious to know if prolonged serotonin syndrome could be a cause of my heart disease, any information would be very helpfull,
many thanks
david hirst
Hi David,
Thanks for your note. Very sorry to hear about your heart attack but glad that you are doing fine now. I looked up the medicines you are/were taking and none is connected to any heart problems alone, however, the combination of Tramadol and Fluoxetine can cause serotonin syndrome–well each alone can cause serotonin syndrome actually. Fluoxetine is an SSRI (selective serotonin reuptake inhibitor) and Tramadol is an opioid that acts like an SNRI (serotonin–norepinephrine reuptake inhibitor), so you definitely were serotonin overdosed. I would suspect that the heart attack was unrelated though the effect of serotonin cannot be ruled out. Serotonin does affect the heart by causing vasoconstriction (constricting the blood vessels thereby increasing blood pressure) and in some people vasodilation (dilating the blood vessels and reducing blood pressure). This combination can compromise a heart that is otherwise weak, unhealthy, or has some congenital issues.
The systolic impairment that your echocardiogram showed may indeed be the outcome of such mixed messages, particularly since your heart is otherwise normal.
I have a patient I am working with who had a heart attack and now sports a stent. Yet, when I asked this person to get a CAC scan, a Coronary Artery Calcium scan, which shows calcium deposits in the arteries in the heart, I found something interesting. People with heart attack usually have very high scores on the CAC scan but this person had almost nothing! This is important, because one can get a heart attack from having too much homocysteine buildup in the blood. Homocysteine is an amino acid, which needs to be removed, else it sort of “gums up” the blood, and can cause major atherosclerosis-like residues on the artery wall, but which have nothing to do with atherosclerosis. The cause of this homocysteine buildup is the person’s inability to methylate folic acid into folate… yep, vitamin B9. It is that simple in many cases, only doctors never ever look past their noses. Just about every processed food you eat is fortified with folic acid, and a large percent of the population cannot methylate that and get sick as a result.
I recommend you do two things to get to the bottom of this and find out if your heart attack was really caused by your heart–meaning high atherosclerosis level, so need to see the CAC score, or high homocysteine levels in the blood, which then leads us to homocysteine causing your heart attack. If neither is the case, we can entertain the serotonin medications and the possibility that they somehow caused a heart attack. It is not possible to directly check serotonin because your brain serotonin can only be measured by a spinal tap (and good luck getting that), and in the blood they can only measure the serotonin that is circulating to help you eliminate your food by bowel movement by creating the wave-like motion of your intestines. So direct measurement is impossible but we can look at indirect measures of the cause of your heart attack by other means.
The homocysteine test is simple, ask your doctor for a blood test for it. The healthy range is 2-14 though there is a narrower range that I consider healthy and which doesn;t need special B vitamins, which is 2-8. If you are over 14, your heart attack was likely caused by your inability to metylate B9, in which case this will repeat in the future unless you start B9 methylation precursors supplementation: B2, B6, and B12–all of these need to be in active sublingual form. B12 needs to be sublingual methylcobalamin. I also would take a small dose of B9 in methylfolate form, which is pre-methylated. These will remove homocysteine from your blood.
In terms of getting the CAC score scan: it is not covered by insurance (though not expensive) and most doctors have no idea what it is, yet a prescription is required to get it. Only university medical centers or research hospitals provide CAC scan, which is simply a CT scan but with heart electrodes on you. It is a 5-minute procedure. The radiologist then provides a number (please pay extra to get your own report–they will send you a DVD of the actual scan plus the score), which is the score, Anything under 100 is healthy and shows no atherosclerosis of concern. So if your score is less than 100, your heart attack was likely initiated by something other than your personal health–meaning maybe the medicines or serotonin syndrome. If your score is greater than 100, your metabolic health is questionable and potentially your heart attack would have happened with or without the medicines. If your score is over 100, you need to look into improving your nutrition.
Please follow up and let us know how your tests are coming along! I wish you well and good health after your recovery.
Angela
I suffered from serotonin syndrome multiple times but just recently put it together. I got it from l-tryptophan, Lexapro, herbal supplements and 5-htp. Terrifying symptoms. Well, I found out that I am probably susceptible to serotonin and I have taken a large daily dose of dessicated thyroid since I was 19. The t3 in the thyroid raises serotonin levels. Any addition serotonin is unsafe for someone like me taking dessicated thyroid. I never knew that. We need to get the word out!
Dear Wendy,
Thanks for your comment! Indeed, there are gene markers for that susceptibility–I am also sensitive and would react “manic” actually according to my genetics. Unfortunately no doctor ever checks–it is not part of “routine care” to check any genetics. In fact, even when specifically asked for, it is still usually refused. So we are all guinea pigs for medicines without knowing how we react to them in advance–often finding out too late the cause of our response to a drug.
Thank you for the information about desiccated thyroid replacement medicine and serotonin. It will help everyone.
An additional quick note: hypothyroidism is often the result of not consuming enough iodine. Have you tried to increase your dietary iodine? Hypothyroidism can also be autoimmune problem caused by consuming foods you are sensitive to. The most usual suspects are grain (not gluten but all grains), eggs, dairy, and nuts. To test, quit all these and then slowly add them back one by one. The biggest difficulty is that improvements from quitting grains may not show up for 3+ months because they block off your entire metabolic system and the cells need to be replaced across the board. That takes time.
I did the above autoimmune food elimination and in my case I had such incredible response to removing grains that not only did my thyroid go back to normal (I also consume extra iodine) but a host of other autoimmune conditions disappeared, including my asthma, which is driven by grains! I had no clue about that. My arthritis and all allergies also went away. So try it.
Best of luck,
Angela
Dr Stanton. Amazing story. And I’m sorry to hear about your mom. I also wrote my SS story in this amazing blog. We are thinking of starting a SSRI awareness foundation. We are trying to locate doctors and experts to be part of it. If you might be interested please let me know. I’m on Facebook or my Neurotoxicity Support Group. It’s filled with the SSRI injured.
Dear Christian,
Thanks for starting an SSRI awareness foundation. I would be honored to be a part of it. I will join your FB group as well. Thanks for the information and the invitation.
Best wishes,
Angela
Dear Matthew,
I don’t think I have ever read a sadder and more serious story ever anywhere! You are a true warrior and a survivor whose life should be made into a film. I read it now 3 times and still cannot envision the pain and struggle you went through.
I agree with everything you say even in terms of others who may often commit crimes as a result of serotonin syndrome. Unfortunately the world is blind to this for a reason: there are no conclusive tests for serotonin because it is found in 2 places in the body as you know: brain and intestines. 90% of the serotonin in our body is in the intestines and so measuring serotonin levels in the blood will inevitably give results for what is in the intestines since the brain is a “closed room” with no access. Spinal tap (lumbar puncture) is an option that is never used–I suppose because it too comes with risks, it is expensive, and because one of the criteria is fever and most in serotonin toxicity don’t get fever. There are tests that can be performed that can approximate trouble, see here for all available tests as of today. If you page back to the very beginning of the article, you can read the kind of damage serotonin syndrome can cause in addition to death.
Unfortunately the medical system we have is not tolerant toward doctors who ask questions or listen to the family. We have a “silent” system of just prescribing medicines and nothing else. This is also referred to as the McDonaldization of Medicine, a term used even in scientific literature, so it is well-known by all involved but they don’t change the system because of the financial incentives and the ensuing conflict of interest.
I can tell from the “voice” you are writing with that you are no longer at risk–you write amazingly well. I wish we could change the system but we cannot. The only impact we can make is to change the people whom we can reach. Your comment here reaches many readers but I think it would reach even more if you wrote this story for HormonesMatter as a publishable article about your experience and also your suggestions with respect to criminal activity and its connection to serotonin syndrome–or mania, in general, caused by any other medicine that acts on the brain–and there are many of those.
I would be looking forward to reading your article starting a debate–many medical professionals read this blog. It would be helpful!
As for recovery, I find that damage caused by drugs, nutrition, and even genetics to some degree, can be helped by a diet that contains minimal carbohydrates and high fat. That is because glucose (and the associated insulin) causes damage to the brain. The brain is mostly fat and cholesterol so feeding it the right way helps a ton. There are several nutritional plans like this. I favor the ketogenic approach since I feel very comfortable with it. If that is feasible for you, look into it and see if it is something you could try. 🙂
All the best wishes for you and do consider to write this up–please send a note to the owner of this site–found under “contact us.”
Angela
Putting my thoughts in order to make a publishable article would be quite hard for me. In the SSRI toxicity workup linked, many tests are mentioned, but not what results would constitute SSRI toxicity. My earliest results of those tests are from a few months after discontinuing SSRI’s, and not out of range, though I could check with the hospital I was taken to after suicide attempt to see if they maintained those records. An awful reflection of the state of mental health: as I was released from the first hospital and sent to a mental hospital for the remainder of a 72 hour hold, the doctor at the mental hospital screamed at me that I ruined my liver and was a druggy because of the high level of opiates in my system… all of which the first hospital administered. My liver may have been inflamed temporarily, but it was fine quite soon after. Absolutely nothing was done to counteract the actual brain or systemic bodily injury of the gassing, and certainly nothing was done to test for prescription drugs as a cause. They simply switched me to another brand of each, and when let out another doctor gave me a different brand of both. Hard to believe, but it seems I lost 20-30lbs of muscle in just a couple weeks and could hardly walk; even though I was a powerful partner in Pas-de-deux, among many other powerful activities. (Men in ballet such as myself mostly throw and catch advanced level ballerinas) I didn’t like to go out in pubic because people would look at me and be horrified by my skeletal appearance, then gay men were constantly hitting on me after I gained a few pounds with the assumption that my apparent anorexia was intentional. No care was given for my physical problems from that incident, nor the physical problems that led up to their assumption that my problem was depression.
Good point about the diet, though my case goes much further than that. I cannot tolerate any carbohydrates, few proteins, and only the highest quality fats. I’ve been on a liquid diet for 18 months as I can digest nothing else. Would SSRI toxicity still be causing such issues after so many years?
You mentioned the pain and suffering I “went” through. It never ended, and apparently won’t.
Mathew, we can help pull the story together. You wouldn’t need every detail, just broad strokes to give others a sense of what happens. We can take what you have written as comments, format and prepare something for you to review and edit, if you are willing.
Dear Matthew,
I think you put your thoughts “on paper” extremely well on the two comments you made. I suppose it just woudl be best to show it as a paper you wrote rather than a comment since (I guess, I don’t know) if as a comment it gets enough attention. Sounds like you went through the same path my mother did–she started with a 3-day hold and then a 7 or 10-day hold by now I don; recall. They used experimental drugs on here there since they removed my power of attorney rights while there. I got her back in near coma and had her taken off all meds for over 2 weeks to allow her to recover to whatever level she could. She passed a week after that. Unfortunately our medical system is totally ruined by doctors who get paid for writing prescriptions. At least we can now see each doctor if they accept any payments from big pharma for anything here. (Use only last name and state since they often enter in their first name differently or a different address so just last name and state.)
Unfortunately they can only test with lumbar puncture but most places will not do it–no idea why. I believe it is a blatant refusal to accept that the most frequently prescribed medicines cause serious danger to people–also, few report in the adverse reporting system and without that the FDA has no records to remove a product from the market or to change the directions of the medicines. In fact, the situation is so bad that I received a threat for my article you commented on. Here is the threat I received:
In terms of long-term effects of SSRIs–yes, it is possible becuase of the way they function. An article I wrote on another blog (my blog) some time ago on how SSRIs work explains how SSRIs work. The reason why their effects can be so damaging is because the inhibitor for the reuptake is a plug (think of it as a cork in a wine bottle) that doesn’t belong there-wrong shape, size and polarity–and the damage it can cause to the delicate proteins that make up the reuptake (sensor) to the neuron can be permanent. Just like wine bottle corks can get stuck, break, end up in the bottle, so can these inhibitor plugs end up in the wrong place. They also press heavy on the channels they block and that alone can change the shape of the protein, making it non-functional. So yes, permanent damage is possible.
However, neurons regenerate and with the proper food you can force regeneration really well. Very sorry that you can eat only liquid foods now but it seems you are eating the best foods you can. Make sure the highest quality fast include heavy duty animal fast since vegetable oils are not very healthy. It sounds like you are on the ketogenic diet if you eat little carbs like fruits and vegetables and no grains at all. Protein is important so if you cannot eat meat, have at least lots of eggs that you can liquefy and also perhaps whey.
I would be glad to help you co-write an article with you!! Let me know if you are interested. 🙂
Hugs,
Angela
I’m completely shutting down due to a three-fold attack by my property management company, and cannot divert my mental/emotional resources to writing a document at this time. I may have to move, with nowhere left to go. [as I composed this, the local temporary manager just wrote to tell me that the tripling of my rent was completely wrong and will handle it for me tomorrow – it seems orchestrated, but I’m glad I have local management on my side]
Can you see my email address, and can you write to me directly so I don’t have to keep this page open and refresh it?
I have no diet name that I know of, but turns out I only eat a small subset of the Low FODMAP diet. I cannot tolerate egg yolks, and to eat beef (when I tolerate it) I have to cook it to mush and only eat the pure protein after pouring off fat, and same goes for chicken. I guess I’m starving my brain. I could eat butter, though have not been. Fish oil doesn’t do well for me lately. Even olive oil tolerance has gone down, and that was my major fat. I’m not tolerating anything that feeds my brain! (and this is new, I was eating a more varied diet until a collapse in November 2015.) I’m mostly eating pure protein. I’m going to Costco right now to buy several gallons of milk and pounds of potatoes for this week (already having egg whites and protein drinks in large quantities) and whatever else I think I can consume. Wish I knew what fats you mean. I’ll try to see what they have.
I battled a host of symptoms for years and was then told by a mature-aged doctor last year that I had serotonin syndrome. The MyDNA tests showed amitriptyline in the red traffic light section of the report and reported that I would get myopathy from Amitriptyline but I was on other serotonergic medications, e.g. curcumin. My problem is to prove it to the insurance company in Australia as they will not take the MyDNA report as clinical proof. What specialist do I have to see? How do I know that I do not have mitochondrial damage? I was sent to a geriatrician because of my cognitive decline (confusion, memory loss, etc) and the GP wanted to rule out dementia. Can anyone answer my question
Hi Lyn,
Thanks for your note. A few things are important to discuss. Curcumin is held in great tradition in Indian medicine but it seems that most research is coming from there and several had to be retracted for falsifying data. It is really hard to get a good understanding on what curcumin does–we know that food is medicine and I am sure that curcumin also has some properties that help certain health conditions–it seems to be used for depression in many articles, mostly experimented on mice. I cannot make heads or tails out of curcumin and its serotonin connection by reliable research.
In terms of Amitriptyline, yes, there is a definite possibility of trouble. It is an SNRI with serotonin reuptake inhibition being the strongest. The trick with genetics is to understand why a particular condition may exists in connection with genetic predisposition. In your case, the thing to look at are two genes: CYP2D6 and CYP2C19 (not sure your genetics company looked at that). These genes are responsible for how you metabolize drugs–meaning the speed with which they break down. There are several categories, of which 2 can get one into trouble: the extremely slow metabolizers–the drug takes very long to exit the body and it can then cause more effects, including inhibiting the neurons’ reuptake longer, forcing serotonin release longer. If this is very long, and you are due to take another pill before the first one cleared from your body, in time this can pile up to serotonin toxicity, e.g serotonin syndrome.
The other case is if you are an ultra fast metabolizer. In this case your body gets an overdose immediately and then quickly all effects stop. For example, ultra metabolizers of medicines don’t get any benefit from most pain killers because they metabolize them very fast but they get overdosed first. Many migraineurs are ultra fast metabolizers–I am one of them–and so time release medicines don’t work as time release as they get to be metabolized very fast. Of course, you can see from this that an overdose is eminent immediately after the drug is taken but it clears from the body very fast.
So if you were to use any genetic evidence, it would have to be these two genes.
I am not sure if there is a way to connect Amitriptyline to mitochondrial damage–basically no drug can be connected to mitochondrial damage since there is no mitochondrial “memory” to look at what caused what. There are hundreds of thousands of mitochondria in every cell and in neurons they number in the millions. If they were all damaged, we would not have this conversation, since without some properly functioning mitochondria, you would not be alive. So that also makes it more difficult to find which mitochondria is damaged, where they are, and from what they are damaged. See the difficulty?
However, you seem quite well now in terms of your brain functioning so likely your serotonin syndrome passed–meaning serotonin syndrome doesn’t last for a very long time. It is fast–within days–and if the serotonin medicine continues, the person is dead. So the fact that you are here and writing, means that you no longer have serotonin syndrome. So there is not much you can do about past events that were not caught in time.
In terms of your cognitive decline: all reuptake inhibitors cause a cognitive decline independent of serotonin. As you read the article I need not repeat how reuptake inhibitors work, but some reuptake inhibitors change the shape of the reuptake and even after you quit the drug, the reuptake is not able to work. So these drugs are neuro-degenerative. They all are; every single one of them. The best thing you can do is to slowly reduce that drug and after you are not takign any medicine, increase your serotonin the right way. By far the biggest serotonin booster is the sun, so spend some time on the sun every single day. Heavy resistance training exercise or intense running/hiking also boost serotonin. Turkey, the food after which everyone tends to fall asleep, is serotonin rich. Since you had/have depression, one of the most important things you can do is to remove those foods from your diet that enhance depression: refined carbohydrates–all processed foods, juices, smoothies, shakes, anything with any flour, anything sweetened in any way–even with substitutes, naturals, or honey–all canned prepared foods, etc., should be stopped by you. Focus on eating whole fresh foods that you make from scratch. It needs not be fancy or expensive but it needs to be fresh and prepared by you. Like, in the US, in all grocery stores, those who eat healthy whole fresh foods never visit the middle isles of the store but shop “on the periphery”.
Research shows that for many people, the LCHF (low carbs high fat) diet is the best–particularly if you have a very sensitive brain, like you do with depression. To boost the health, recovery, or replacement of damaged mitochondria by healthy ones, intermittent fasting appears to initiate the best job–minimum 16 hours of only water and salt, and with some regularity; I practice this almost every day. It helps your cognition to recover, it rebuilds the brain and all mitochondria that are damaged get replaced. So there are options for you but you need to stop that medicine first. It interacts with the ketogenic metabolic process (it blocks H1 and H2 receptors that cause major problems for the drug to find its way in the fat burning metabolic process and it ends up as an agonist instead) and 16+ hours of intermittent fasting will bring you into the ketogenic metabolic process. So please reduce this drug and stop it before you start anything I mentioned.
Good luck to you!
Angela
Hey guys.
I am 5 months postpardum and shortly after I gave birth I started low dose Zoloft which has been raised each month to a HIGH dose to no avail. It helped a lot actually but now things are starting to feel worse since starting other meds. I end up having three discs to rupture from a fall/DDD/OA and was in severe pain. I was given Gabapentin, Cymbalta and Flexeril on Top.. Then they just added Meloxicam and a,10,day course of steroids. I also took pain meds but only for 2,weeks. My pain is worse, I have migraines, sweating, anxiety and hot flashes, chills and mild disorientation which is probably contributed to all the crap they have me on. I also have bowel incontinence and bowel changes on and off.
I suppose if it was severe I would be so confused and in the hospital. But I may have some serotonin syndrome. I am also nauseated. I think the Cymbalta I started a few days ago is the contributing factor. I’m worried. Why would doctors do this?!?
Hi Brandy,
Zoloft (sertraline–see the comment I just posted on that for Mina) is an SSRI (selective serotonin reuptake inhibitor) that alone can cause serotonin syndrome but Cymbalta and Zoloft are both doing exactly the same thing!! You have been overdosed and are indeed having a serotonin syndrome. I just ran a drug interaction check at drugs.com’s website for you because I suspected that you have many interactions. I found that you have MAJOR and MODERATE interaction between several of your medicines and you also have what is called “therapeutic duplication” which means you are taking more than one medicine for the exact same purpose and thus you are overdosed.
Here are your interactions:
MAJOR:
sertraline cyclobenzaprine
Applies to: Zoloft (sertraline), Flexeril (cyclobenzaprine)
Using sertraline together with cyclobenzaprine can increase the risk of a rare but serious condition called the serotonin syndrome, which may include symptoms such as confusion, hallucination, seizure, extreme changes in blood pressure, increased heart rate, fever, excessive sweating, shivering or shaking, blurred vision, muscle spasm or stiffness, tremor, incoordination, stomach cramp, nausea, vomiting, and diarrhea. Severe cases may result in coma and even death. You should seek immediate medical attention if you experience these symptoms while taking the medications. Talk to your doctor if you have any questions or concerns. Your doctor may already be aware of the risks, but has determined that this is the best course of treatment for you and has taken appropriate precautions and is monitoring you closely for any potential complications. It is important to tell your doctor about all other medications you use, including vitamins and herbs. Do not stop using any medications without first talking to your doctor.
MAJOR
sertraline duloxetine
Applies to: Zoloft (sertraline), Cymbalta (duloxetine)
Using sertraline together with Duloxetine can increase the risk of a rare but serious condition called the serotonin syndrome, which may include symptoms such as confusion, hallucination, seizure, extreme changes in blood pressure, increased heart rate, fever, excessive sweating, shivering or shaking, blurred vision, muscle spasm or stiffness, tremor, incoordination, stomach cramp, nausea, vomiting, and diarrhea. Severe cases may result in coma and even death. You should seek immediate medical attention if you experience these symptoms while taking the medications. Talk to your doctor if you have any questions or concerns. Your doctor may already be aware of the risks, but has determined that this is the best course of treatment for you and has taken appropriate precautions and is monitoring you closely for any potential complications. It is important to tell your doctor about all other medications you use, including vitamins and herbs. Do not stop using any medications without first talking to your doctor.
MAJOR
cyclobenzaprine duloxetine
Applies to: Flexeril (cyclobenzaprine), Cymbalta (duloxetine)
Using cyclobenzaprine together with Duloxetine can increase the risk of a rare but serious condition called the serotonin syndrome, which may include symptoms such as confusion, hallucination, seizure, extreme changes in blood pressure, increased heart rate, fever, excessive sweating, shivering or shaking, blurred vision, muscle spasm or stiffness, tremor, incoordination, stomach cramp, nausea, vomiting, and diarrhea. Severe cases may result in coma and even death. You should seek immediate medical attention if you experience these symptoms while taking the medications. Talk to your doctor if you have any questions or concerns. Your doctor may already be aware of the risks, but has determined that this is the best course of treatment for you and has taken appropriate precautions and is monitoring you closely for any potential complications. It is important to tell your doctor about all other medications you use, including vitamins and herbs. Do not stop using any medications without first talking to your doctor.
MODERATE
sertraline gabapentin
Applies to: Zoloft (sertraline), gabapentin
Using sertraline together with gabapentin may increase side effects such as dizziness, drowsiness, confusion, and difficulty concentrating. Some people, especially the elderly, may also experience impairment in thinking, judgment, and motor coordination. You should avoid or limit the use of alcohol while being treated with these medications. Also avoid activities requiring mental alertness such as driving or operating hazardous machinery until you know how the medications affect you. Talk to your doctor if you have any questions or concerns. It is important to tell your doctor about all other medications you use, including vitamins and herbs. Do not stop using any medications without first talking to your doctor.
MODERATE
sertraline meloxicam
Applies to: Zoloft (sertraline), meloxicam
Using sertraline together with meloxicam may increase the risk of bleeding. The interaction may be more likely if you are elderly or have kidney or liver disease. Talk to your doctor if you have any questions or concerns. Your doctor may already be aware of the risks, but has determined that this is the best course of treatment for you and has taken appropriate precautions and is monitoring you closely for any potential complications. You should seek immediate medical attention if you experience any unusual bleeding or bruising, or have other signs and symptoms of bleeding such as dizziness; lightheadedness; red or black, tarry stools; coughing up or vomiting fresh or dried blood that looks like coffee grounds; severe headache; and weakness. It is important to tell your doctor about all other medications you use, including vitamins and herbs. Do not stop using any medications without first talking to your doctor.
MODERATE
cyclobenzaprine gabapentin
Applies to: Flexeril (cyclobenzaprine), gabapentin
Using cyclobenzaprine together with gabapentin may increase side effects such as dizziness, drowsiness, confusion, and difficulty concentrating. Some people, especially the elderly, may also experience impairment in thinking, judgment, and motor coordination. You should avoid or limit the use of alcohol while being treated with these medications. Also avoid activities requiring mental alertness such as driving or operating hazardous machinery until you know how the medications affect you. Talk to your doctor if you have any questions or concerns. It is important to tell your doctor about all other medications you use, including vitamins and herbs. Do not stop using any medications without first talking to your doctor.
MODERATE
gabapentin duloxetine
Applies to: gabapentin, Cymbalta (duloxetine)
Using gabapentin together with Duloxetine may increase side effects such as dizziness, drowsiness, confusion, and difficulty concentrating. Some people, especially the elderly, may also experience impairment in thinking, judgment, and motor coordination. You should avoid or limit the use of alcohol while being treated with these medications. Also avoid activities requiring mental alertness such as driving or operating hazardous machinery until you know how the medications affect you. Talk to your doctor if you have any questions or concerns. It is important to tell your doctor about all other medications you use, including vitamins and herbs. Do not stop using any medications without first talking to your doctor.
MODERATE
meloxicam duloxetine
Applies to: meloxicam, Cymbalta (duloxetine)
Using Duloxetine together with meloxicam may increase the risk of bleeding. The interaction may be more likely if you are elderly or have kidney or liver disease. Talk to your doctor if you have any questions or concerns. Your doctor may already be aware of the risks, but has determined that this is the best course of treatment for you and has taken appropriate precautions and is monitoring you closely for any potential complications. You should seek immediate medical attention if you experience any unusual bleeding or bruising, or have other signs and symptoms of bleeding such as dizziness; lightheadedness; red or black, tarry stools; coughing up or vomiting fresh or dried blood that looks like coffee grounds; severe headache; and weakness. It is important to tell your doctor about all other medications you use, including vitamins and herbs. Do not stop using any medications without first talking to your doctor.
THERAPEUTIC DUPLICATIONS
Therapeutic duplication is the use of more than one medicine from the same drug category or therapeutic class to treat the same condition. This can be intentional in cases where drugs with similar actions are used together for demonstrated therapeutic benefit. It can also be unintentional in cases where a patient has been treated by more than one doctor, or had prescriptions filled at more than one pharmacy, and can have potentially adverse consequences.
Duplication
Antidepressants
The recommended maximum number of medicines in the ‘antidepressants’ category to be taken concurrently is usually one. Your list includes two medicines belonging to the ‘antidepressants’ category:
duloxetine (active ingredient in Cymbalta (duloxetine))
sertraline (active ingredient in Zoloft (sertraline))
In terms of your symptoms that you are listing you are definitely starting serotonin syndrome. Please visit your nearest ER (don’t make a doctor’s appointment but head to ER), take your list of medicines, take this note I wrote here–specifically because I want them to see the interactions and the therapeutic duplications) and you tell them what you have!! Don’t let them stop you from what you have to say. If you feel you need a more powerful voice, take a friend who has no fear of what we call “white coat effect” to be sure you are not discounted.
Unfortunately many doctors have no idea what they are doing (I call them clueless doctors) because they were never told about the interactions and also never were taught to recognize a serotonin syndrome.
Please head to the ER a.s.a.p.
Best wishes,
Angela
Please help me. I am bedridden with multiple symptoms. Went to my local ED after husband called poison control (who said I had SS and to head to the ED) Despite having a complete history of meds and symptoms gradually onsetting in the past year, including psychotic and mania, i was denied SS by simple blood and urine tests which I know doesn’t diagnose SS. I was given 1mg ativan shot and sent home which stopped the tremors for now and a histamine for sedation. I work in the medical field and cannot get my PCP or Hospital to write me even an excuse to take 1 week off of work. I’m still being directed to take all the meds I’ve been on and increase the Benzos. I know you are a busy lady, but I would love to send you my history and know what you think about it. We;ve looked up everything possible on the web and everything points to SS but no one will listen. I’m probably going to lose my job because i can’t function. If you can, please email me. -Amanda
Dear Amanda,
I am very sorry for what you are going through. Since I am a PhD and not an MD, I cannot guide you in any way in place of an MD. However, since I just had anotehr person contact me with a similar problem who was on over 20 medications, 5 of which were therapeutic duplication, I asked her to go back to her family doctor to have that cleared up. Her doctor refused saying she was not the one who prescribed all those and didn’t help her. Then I asked the patient to head to the doctor(s) who prescribed those to her–she was no longer in touch with them. I next recommended she visit the ER to have the doctors there help her. They refused.
After that she managed to get a hold of one of her doctors–I think her neurologist–who said that while she can help her clean up her medicines, a patient doesn’t need any permission from any doctor to stop or reduce a medicine!
Therefore, if you believe you have serotonin syndrome, please ask your pharmacist which medicine (assuming you take more than one) is causing the problem. Then you can slowly reduce little by little or if your symptoms are very bad, take a bigger cut but don’t quit any medicines cold turkey because that can really hurt you!
I wish you the best of luck and please keep me updated!
Angela
Dr. Angela,
I am in same situation as Amanda, except for the fact that I have been stuck inside my home now for almost 3 years! After going to EVERY TYPE of specialist (and all of them receiving a full list of my VERY DANGEROUS “Therapeutic Duplications” – 14 Interactions), I have all but given up hope. I have begged my doctor to help…and she is one of the MANY CLUELESS DOCTORS.
You could get a Grant, and start a Clinic just for the Tens of Thousands of us that, right now, are Silently Dying because of Medications our doctors have failed to research. But, hey! At least THEY got some good gifts from the Drug Reps, right?
I know that I am in the Severe to Critical stage of my Serotonin Syndrome. I have taken 300mg. of TOPAMAX since 2002, along with 400mg of Celebrex. Within a year of those drugs, I was MOVED BETWEEN 3-4 Anti-depressants AND varying dosages of each, before settling on CELEXA which I’ve now been on for 14 years. AT THE SAME TIME, my “Psy-quack-atrist” and my doctor were trying to work through 3 DIFFERENT ADHD Medications / Doses to find the right fit. From 2003-2012, I think, I was on varying doses of ADDERALL (2008-2012, with the last two years at 30mg).
**BETWEEN 2008-2011, I began showing MAJOR behavioral changes, and LOST EVERYTHING – including my ability to Reason, Remember, Focus, and Control my Emotions… I lost 4 Jobs; 1 home; a 10 year relationship; the REALLY CLOSE RELATIONSHIP I had with my now grown children; the use of my left hand, possibly (some of the accident) due to my inability to focus on the job I was doing; the respect of my peers, in the Counseling Profession…so much more….After this period, I ended up spending a little bit of time in one of our “special hospitals”, because of Suicidal and Homicidal Threats!
In the last year, my ADHD MEDICATION was changed to VYVANSE, and was worked up to Max dose of 70mg.
After all that, ONLY MORE DRUGS WERE ADDED. Lamictal, Gabapentin, Ativan…
EVERY SYMPTOM LISTED UNDER THE SEVERE CATEGORY ON THE MAYO CLINIC SITE DESCRIBES ME – but I cannot find an Inpatient Center that will HEAR ME SAY “It’s SS. I need to be MEDICALLY DETOXED FOR SS, and Monitored Carefully. I need to have My Serotonin Levels Monitored – whatever that entails (checking other body systems)? I need Mental Health intervention, to assess what Medications I ACTUALLY NEED, and what diagnoses may have been artificially created by Therapeutic Duplication. And, I need to be set up with Regular Visits with a local “SMART, ON-POINT PSYCHIATRIST / Physician” who will stay on the treatment plan that I truly need to follow.
Oh my, dear Tracey. I am so sorry to hear what you are doing through. Unfortunately I must agree: there are many clueless doctors out there though I am shocked to hear that you cannot find a single good doctor who can help you. I was contacted by another person in a similar situation like yours and an MD responded to her plea suggesting that a patient never needs an approval for not taking a medicine. Since I am not an MD, I cannot advise you in any which way. But I can tell you what I would do (and what I did).
I use this drug interaction site to check for interactions “drug interaction checker” and used to print out all MAJOR interactions. I then would scroll to the bottom to find THERAPEUTIC DUPLICATION and print all that out as well. I would head to a pharmacy and ask for consultation with a pharmacist to see what he/she says. Not all pharmacies are willing to discuss interactions and therapeutic duplication but worthy a try.
If that doesn’t work, and no one is helping me, I would help myself. That is basically what I did with migraines… No one could help so I just took matters into my own hand. I studied up on each medication–they are pretty well described on wikipedia (usually under generic name) and find those with the worst reputation and most side effects. I would start tapering very slowly one medication at the time, starting with the therapeutic duplication types. That is because since they are duplicates, they do the same thing, and it is least likely that removing a duplicate will cause any trouble–it will likely improve things.
However, some of these medicines take a very long time to reduce and quit. When I was in the process of reduction I removed a tiny bit from one day but kept the rest until my body got used to the change then would remove a little bit from another day 3 days away as well and stay that way for some time and so forth until every day of the week was at the reduced dose and then repeat chopping off a little more. This also allowed me to see if I had any bad reactions for the reduction so I could stop the reduction if I had to–I never had to.
This worked very well for me. It does take a very long time to come off on SSRIs–some can take over a year to taper off from it but at the end there is nothing more important than safety. Having SS looming in the background is not safe, so you should look into what I did. Some SSRIs and voltage gated calcium channel blockers may leave permanent damage or just a longer lasting damage that heals over a long time.
Do the best you can. Your writing is very clear and coherent, you sound really good and quite capable to do as you wish. I am sure you can achieve miracles. <3
Best wishes,
Angela
Hi Angela,
I had my first experience dealing with ssris a little less than three months ago. I was prescribed 25mg a day. I was not consistent with it like I should have been and took them on a off for about two weeks. During the time I was on them I felt like I had the flew and would get sharp pain at my temples that would come and go. I wasn’t on anything else and have never had issues with headaches before so I immediately contributed my symptoms to the Zoloft (sertraline). I stopped te medication completely and the headaches got worse. Now I get them almost daily. I’ve been back to my doctor and no one can tell me what’s happened. They brush off any mention of it being the ssri. I am getting scared now to a point where I don’t even think it is the medication anymore. I’ve had a normal Ct, and requesting an MRI (but deep down I still feel like the Zoloft messed me up).
Hi Leah,
How scary! May I ask what kind of a headache do you have? Where exactly is the pain located? Does it respond to any OTC? I am not trying to diagnose only trying to exclude some possibilities that would not show up in the scanners. Headache is one of the top most common side effects of Zoloft–while takign it. There is no mention of it (or of anything else) after you stop taking it.
I copy-pasted here all the adverse reactions from wikipedia:
Very common (>10%)
Fatigue
Insomnia
Nausea
Dry mouth
Diarrhea
Headache
Ejaculation disorder
Dizziness
Sweating
Common (1-10%)[edit]
Agitation
Anorexia
Constipation
Dyspepsia (indigestion)
Decreased libido
Sweating
Tremor
Vomiting
Impaired concentration
Nervousness
Paroniria (i.e., depraved or morbid dreaming/nightmares)
Yawning
Palpitations
Increased sweating
Hot flushes
Weight decrease
Weight increase
Myoclonus
Hypertonia
Bruxism (teeth grinding)
Hypoaesthesia
Menstrual irregularities
Sexual dysfunction
Rash
Vision abnormal
Asthenia
Chest pain
Paraesthesia
Tinnitus (hearing ringing in the ears)
Uncommon (0.1-1%)
Hypertension (high blood pressure)
Hyperkinesia
Bronchospasm
Oesophagitis (swollen oesophagus)
Dysphagia
Haemorrhoids
Periorbital Oedema
Purpura
Cold Sweat
Dry skin
Nocturia
Urinary Retention
Polyuria (excessive urination)
Vaginal Haemorrhage
Malaise
Chills
Pyrexia (fever)
Thirst
Pollakiuria
Micturition disorder
Salivary Hypersecretion
Tongue Disorder
Osteoarthritis
Muscular Weakness
Back Pain
Muscle Twitching
Eructation (belching)
Dyspnoea (air hunger)
Epistaxis (nose bleed)
Oedema peripheral
Periorbital edema
Syncope
Postural dizziness
Tachycardia (high heart rate)
Urticaria (hives)
Migraine
Abnormal bleeding (esp. in the GI tract)
Muscle cramps
Arthralgia
Depressive symptoms
Euphoria
Hallucination
Alopecia (hair loss)
Urinary Retention (being unable to pass urine)
Pruritus
Amnesia memory loss.
Urinary incontinence
Eye pain
Asymptomatic elevations in serum transaminases
Abnormal semen
Melaena (black faeces due to a bleed in the stomach)
Coffee ground vomiting
Haematochezia
Stomatitis (swollen mouth)
Tongue ulceration
Tooth Disorder
Glossitis (soreness/swelling of the tongue)
Mouth Ulceration
Laryngospasm
Hyperventilation (breathing more often than required to keep one’s blood sufficiently oxygenated)
Hypoventilation (breathing less often than required to keep one’s blood sufficiently oxygenated)
Stridor
Dysphonia (voice disorder)
Upper Respiratory Tract Infection
Rhinitis (irritation/inflammation inside the nose)
Hiccups
Apathy
Thinking Abnormal
Rare (<0.1%)
Allergic reaction
Allergy
Anaphylactoid reaction
Face oedema
Priapism
Atrial arrhythmia
AV block
Coma
Peripheral Ischaemia
Injury
Vasodilation Procedure
Lymphadenopathy
Involuntary muscle contractions
Galactorrhoea (lactation that is unrelated to pregnancy or breastfeeding)
Gynaecomastia (swelling of breast tissue in men)
Hyperprolactinaemia (high blood prolactin levels)
Hypothyroidism (underactive thyroid gland)
Syndrome of inappropriate secretion of antidiuretic hormone (SIADH)
Pancreatitis (swollen pancreas)
Altered platelet function
Haematuria (blood in the urine)
Leukopenia (low white blood cell count)
Thrombocytopenia (low blood platelet count)
Increased coagulation times
Abnormal clinical laboratory results
Hyponatraemia (low blood sodium)
Conversion Disorder
Drug Dependence
Paranoia
Myocardial Infarction (heart attack)
Bradycardia
Cardiac Disorder
Suicidal Ideation/behaviour
Sleep Walking
Premature Ejaculation
Hyperglycemia (high blood sugar)
Hypoglycemia (low blood sugar)
Hypercholesterolaemia (high blood cholesterol)
Vasculitis
Aggressive reaction
Psychosis (hallucinations and delusions)
Mania (a dangerously elated mood)
Menorrhagia (an abnormally excessive amount of menstrual bleeding)
Atrophic Vulvovaginitis
Balanoposthitis
Genital Discharge
Angioedema
Photosensitivity skin reaction
Enuresis
Visual field defect
Abnormal liver function
Dermatitis
Dermatitis Bullous
Rash Follicular
Glaucoma
Lacrimal Disorder
Scotoma
Diplopia
Photophobia
Hyphaema
Mydriasis
Hair Texture Abnormal
Neoplasm
Diverticulitis
Choreoathetosis
Dyskinesia
Hyperaesthesia
Sensory Disturbance
Gastroenteritis
Otitis Media
Skin Odour Abnormal
Unknown frequency
QTc prolongation
Anaphylactoid Reaction
Allergic Reaction
Allergy
Neuroleptic malignant syndrome. A potentially fatal reaction that most often occurs as a result of the use of antipsychotic drugs. It is characterised by fever, muscle rigidity, rhabdomyolysis (muscle breakdown), profuse sweating, tachycardia, tachypnoea (rapid breathing), agitation.
Stevens-Johnson syndrome a potentially fatal skin reaction.
Toxic epidermal necrolysis another potentially fatal skin reaction.
Torsades de pointes a potentially fatal change in the heart’s rhythm.
Cerebrovascular spasm
Serotonin syndrome similar to neuroleptic malignant syndrome but develops more rapidly (over a period of hours instead of days/weeks for neuroleptic malignant syndrome)
Bone fracture
Movement disorders
Diabetes mellitus
Dyspnoea
Jaundice yellowing of the skin, mucous membranes and eyes due to an impaired ability of the liver to clear the haem breakdown by product, bilirubin.
Hepatitis
Liver failure
Persistent Sexual Dysfunction
So yes, it is likely caused by the medicine. The reason why you still have the headache maybe from the inhibitor not letting go of the neuron’s reuptake (sensor that the neuron made enough) and so you may also not be making and releasing enough neurotransmitters. Hopefully this is temporary only taking longer than you expected to release. Let me know how it goes! There may be a few things to try if it is not improving soon.
Hugs,
Angela
Hi Angela,
Thank you so much for the brief reply! It’s hard to describe them. I want to say headaches but I’ve had headaches before from normal stressors that go away when I sleep them off or take a few Advil. These are sharp pains almost spasm like. They last for a few seconds, occur on different parts of my temples, forehead, top scalp area if that makes any sense. I don’t want to say zaps, because I don’t know what that feels like but it could be. I notice that occur when I get excited, become agitated or simply have sudden eye movement. This is also so strange,new, and scary to me to say the least. What you are saying makes a lot of sense. Through research on these drugs I’ve learned that even with a small dose of any type of antidepressant it can’t take a while for the brain to return to homeostasis granted no permanent damage has been done.
Hi Leah,
It seems you may be getting cluster headaches… just an estimation. If it is cluster headaches, what you may want to ask your doctor to prescribe is oxygen (in those tanks or oxygen concentrator machine you can plug into the wall or on battery but they are pricey). I think trying an oxygen tank and using oxygen at the first sensation of a stab may help. Cluster headaches respond to oxygen if started early.
Unfortunately, ibuprofen can also cause rebound headaches; one needs to be careful of all medicines! 🙁
Indeed, the brain takes some time to return to homeostasis. To help it to do so, if you stop all added sugars, it will provide a huge help! The brain doesn’t do very well with sugar. Plus, it will benefit you entire mood and how you feel. So there is hope! 🙂
Best of luck!
Hugs,
Angela
My daughter started Zoloft recently and now she’s getting those sharp pains in the temple area. This is weird and scary. I think she needs to get off the Zoloft
Hi Angela,
To answer your other questions it will occasionally respond to ibuprofen, anything else will cause rebound type headaches. I was prescribed butalbutal which helped a bit but then got headaches from that and it ended up irritating my stomach, causing upset stomach. I’m now trying sumatriptan. I was offered a slew of other ssris to help with the original zoloft withdrawel but turned those all down. I don’t ever want to touch another antidepressant again! The everyday anxiety I was originally prescribed the zoloft for was nothing compared to what I’m going through now.
I get Cluster headaches. I found out they were Cluster, and not Migraine, when I was put on Prozac. But only because I questioned my doctor about a possible drug interaction between Prozac and Imitrex! When I asked her about taking them together she had to look it up online. She came back and said that Serotonin Syndrome was a possibility, but it was very rare and I shouldn’t worry about it! Well, I don’t trust doctors so I did my own research. That’s when I figured out that my “migraines” were really Cluster headaches! I should NEVER have been taking oral Imitrex. I got a prescription for Oxygen and it worked really well until I went off Prozac. That year, 2016, my Cluster headaches were horrific! Oxygen did nothing! Even when I went up to a very high flo rate. The only thing that made the oxygen work again was Benedryl. (I discovered that year, that Cluster headaches are also known as Serotonin headaches and Histamine headaches!) I was on Prozac for over a decade.
Hi Susan,
I am glad you did your research and found out you had cluster headaches and not migraines. Most doctors cannot tell the difference between any headaches let alone define what a migraine is or what a cluster headache is. Even academic literature is confused, and depending upon what academic journal you read, you will find different definitions. This can make everyone’s life miserable, as it made yours. Very sorry about that. Interestingly, after you mentioned Benadryl, and antihistamine, I looked up research on that. I am a migraine specialist and not cluster headaches–though I do have plenty of cluster headache sufferers in my group, so it was worthy of my time. Indeed, you do release high histamines during an attack, so an antihistamine is a great choice. In terms of Prozac (or any SSRI or SNRI or triptans), indeed, the problem is that depending on where they take the serotonin level measurement during the attack, it is low serotonin in some places (such as blood) and high in some other places (such as the spinal fluid–which is what is in your brain as well). And so the message is mixed and confuses doctors. If serotonin is low in the blood but high in the brain, I am sure they don’t know how to relate to that. It does take some figuring out but here it goes.
Over 90% of all serotonin is made and used by our intestines and thus it is not in our brain. Only 10% max is made and used by our brain. I am quite positive that many doctors don’t know this and that your doctor, who had to get on the internet to check interaction probably would not have known that. I don;t actually blame your doctor–at least she admitted she needed to look up the interaction and at least SHE LOOKED!!! Most doctors would not even take the time to find out. So actually she seems to have been a pretty good doctor in some ways! Better than most, though I understand you ended up getting hurt. And that needs an explanation, given that we know that for cluster headache, serotonin levels differ depending on where it is measured.
It is assumed that giving triptant (serotonin) or SSRIs or SNRIs are good for everything froma tooth ache to the death of your child. It is a crazy world out there when it comes to these dangerous drugs. Prozac is an SSRI, and so it is supposed to increase brain serotonin such that it blocks the natural “how much do I already have” sensor (reuptake), so the brain cell thinks it has not yet made enough. This an SSRI forces the brain into a serotonin machine at all cost. While takign any serotonin medicine only transfers little serotonin or SSRI into the brain because of the blood brain barrier, enough gets through to mess with this reuptake mechanism. And in the brain, when something is blocked from being used, communication is broken and degeneration starts.
In your case, you had more than enough serotonin in your brain during a cluster headache attack but not enough in your peripheral blood supply and so it probably increased serotonin in your blood to higher levels, which was good, but it also forced the brain to make more, which was bad. When you stopped Prozac–and I don’t know how you stopped, since these drugs have warning on them to not just quit because of discontinuation syndrome–your brain had to re-establish its lost reuptake functions and connections. This takes time–hence the warning about discontinuation syndrome. This could have been the cause of your current struggle, not sure. The standard of care, believe it or not, is triptans or a preventive, such as an SSRI, for cluster headaches. Most doctors have no idea about oxygen either. So you are ahead of the game.
So hold tight and allow serotonin to be rebuilt naturally: go on the sun as much as you can; it has a normalizing function.
Best wishes for you!
Hugs,
Angela
Can someone tell me how long serotonin syndrome lasts once you stop taking the medication that caused it?
My niece is 24 years old, has been on sertraline for a short while 6 months maybe. She was also taking the highest amount of tramodol.
She was admitted to hospital following stomach pains, had raised white cells but they didn’t no what was wrong with her.
Few days later she was released, and she continued her medication at home. Sertraline and tramodol.
Then suddenly like a switch had gone off, she became confused, manic episodes, rambling, talking nonsense and over evaluating everything. She didn’t make sense. Had high fever, chills, shakes loads of symptoms.
she was put In a mental health facility query seretonin syndrome.
They gave IV fluids and 1 paracetamol a day.
A week later she was released to be monitored at home each week.
It’s been 2 weeks now and she has slightly improved but is still confused and rambling. She’s unable to care for her young kids and needs constantly watching.
They have prescribed her a sleeping tablet to take once at night. But she hasn’t slept in two days.
She sits down and constantly thinks, but stares into space or she follows an adult around the flat rambling on about things That don’t make sense.
I’m so worried for her.
Will the symptoms go away? Her symptoms are that of a mentally ill patient.
Dear Mina,
I am very sorry to hear that your niece got serotonin syndrome. It seems like she has a very severe reaction. Severe serotonin syndrome damage may take a very long time to recover since in addition to the extra serototonin that must clear, your niece is also going through severe withdrawal at the same time. Tramadol is a narcotic and stopping that causes major withdrawals. Sertraline is the one that caused her serotonin syndrome (like in the article my mother’s death).
The hospital did not do its treatment properly. For serotonin syndrome she should have received: muscle relaxants, benzodiazepines like diazepam (Valium), serotonin-production blocking agents such as cyproheptadine, oxygen, drugs that control heart rate and blood pressure (it can be too high or too low). These all in addition to intravenous (IV) fluids.
It is also possible that her brain is still not free from all the extra serotonin since she didn’t receive serotonin blocking agents plus after stopping SSRI, like Sertraline, the brain often doesn’t know how to make or stop making serotonin–there is recovery time needed for the “inhibitor” to be removed from the receptor and this time is very much individual. Unfortunately, sometimes the damage is permanent.
Please take your niece back to the ER and explain to them what she is going through so they can run some tests and see if she is suffering withdrawal, still has too much serotonin, or suffered permanent damage.
I wish her well and a big hug to you for reaching out to try to help her! <3
Angela
My wife was recently diagnosed with stage IV cancer; she had breast cancer 10 years ago, and it came back with a vengeance. She has been on citalopram (SSRI) for years for depression. Her cancer is now in her bones, liver, and lungs, so she was in a lot of pain. She can’t tolerate opiods, so she was given Tramadol (a synthetic opiod). After her chemo, she was given Zofran. All three of those have “major” interactions for Seratonin Syndrome – Citalopram/Tramadol, Citalopram/Zofran, and Tramadol/Zofran. She kept getting more and more sick following the chemo, and she finally got so bad we went in and they gave her Zofran through her port. As she was getting it I could actually see her getting more and more distressed as she was getting the infusion. I looked up the interactions on my phone and all three combinations increase the risk of Seratonin Syndrome. She immediately stopped the Zofran and started feeling better within a couple of days. It might just be that she was moving farther from last chemo, but I wonder whether it was the interaction.
There are two things I don’t understand.
1. Why in the world don’t these highly trained “professionals” check for interactions before prescribing these things? If I can look it up so easily on-line, it should be child’s play to write a computer program that checks for interactions as physicians prescribe these things. The medical center is part of a massive operation owned by the University of Pennsylvania, so this SHOULDN’T BE THAT HARD. You prescribe something, and if it’s a potential problem with another med the patient is already taking you get a big red flag. All of the prescription data is entered into their information system, but I really think these electronic systems are an end in themselves rather than being used as the tool they could be. They spend all their time entering data but no time actually LOOKING at it.
2. Can SS cause hand blisters due to toxicity? My wife developed severe hand blisters, and as a result of this and her other discomforts the MD is switching chemo drugs. The current chemo drug was doing great at lowering her marker numbers, and if all of the problems are caused by drug interactions rather than the chemo it would be foolish to switch.
Dear Tom,
I removed your other post so it only appears now once in the right place. I am very sorry to hear about the cancer returning for your wife, metastasized. I am certain that you completely got it right and she was suffering more from the serotonin syndrome building up than the chemo therapy itself, which is brutal on its own.
You have a perfect question about why doctors are so good at prescribing all these medications without looking at interactions. At one level I agree that they are not reading only writing and so they are not aware of what is what but another part of me tells me something else: ignorance. It is, indeed, very easy to find out about drug interactions; here is a website I always use for convenience since it does a perfect job, fast, efficient, and is always correct–it is also free.
I am confident that every single doctor has a drug interaction checker either on their phone or on the computer when they prescribe a medicine only they don’t think it is appropriate to look. I feel (my experience with some of my doctors) is that they are time pressured and feel that they may look less knowledgeable if they need to look things up in front of a patient. Yet those doctors who actually do take the time to look, develop more trust. After all, everyone is human and doctors can forget or make mistakes; looking it up is actually reinforcing trust. I don’t think they realize this.
I also found, on my own experience, that the majority of doctors have very narrow field of specialty and don’t ever test the waters of integrative medicine or study other fields of medicine to broaden their understanding. As a result, they pretend they know enough even if they don’t. This is very sad because lives depend upon their decisions.
And finally, medicine applies a cookie-cutter approach and only symptom treats today. This can be very dangerous, as it was the case for your wife who received such interacting medicines. It remains your job and the job of the rest of us to keep an eye out for our loved ones and learn enough to stop the doctors from making mistakes. It is hard work because most people are not trained medically or scientifically. It is lucky you had the knowledge to look up the interactions and the guts to pass the information on to the doctor. Most people feel intimidated until it is too late.
I congratulate you for your strength and wisdom and wish your wife all the best in a successful chemotherapy treatment and remission.
Hugs,
Angela
Angela, My 82 year old father went to the hospital for stomach pain. He led a very active life, lived on his own and was very happy. He had COPD from working with asbestos and followed all his doctors instructions and was managing it well. While in the emergency room he was his normal self, talking and joking around with the doctors. They ran various test and determined his white cell was high and his lactic acid was elevated, as well as enlarged liver. They decided to admit him for further testing. Shortly after he was given IV fentanyl and Zofran, he then became confused and he broke out in a cold clammy sweat and was unable to respond. He remained this way for quite awhile, they then gave him another dose of fentanyl and Zofran then went into respiratory distress and was put on a breathing tube. He continued to receive IV fentanyl. He was also taking sertraline, which continued while hospitalized. His lactic acid and CO2 levels were off the charts and his protein levels increased everyday. His organs began to fail one by one and he became so septic that blisters formed on his skin. I did not know about serotonin syndrome until I looked into drug interactions, my father was taking sertraline on a regular basis, then given fentanyl and Zofran in the hospital, he went downhill in a matter of hours. The hospital came to me and asked if they could do a autopsy because they did not understand what happened to him. The results of the autopsy were high grade endocrine cancer of the liver, with bone marrow involvement. He was never diagnosed with cancer nor showed any symptoms. Liver cancer increases serotonin levels, then he was given fentanyl and Zofran while taking sertraline. If I know this, how come a team of doctors and nurses did not know what could happen when these drugs are given together. I believed his death was from serotonin syndrome.
Oh my Paula, I am so sorry about your father! Indeed! How come they did not know!? It is further confusing to me that they did not see his liver cancer at such advanced stage since that comes with symptoms that are actually visible–such as the yellowing on the skin. Also, bone cancer is extremely painful from the very beginning so I find that too highly unlikely to have contributed to his passing in the hospital. I am not sure I believe in the autopsy findings of the hospital at all.
When my mother died–in hospital like your father–I asked if they would do an autopsy (they did not want to since “she died from a stroke” but I wanted to find out if she had serotonin syndrome as I diagnosed or Alzheimer’s as they diagnosed, which I knew she did not have). The hospital told me that they will only do autopsy such that it confirms the final cause of death–meaning not the original cause but the “end” cause, which in the case of my mom was a stroke and in the case of your father was multiple organ failure.
In checking on the three medications your father received, I find that fentanyl has a protein binding capacity at a high level of over 80% with metabolic pathway that is hepatic; sertraline is also hepatic with an even higher protein binding ability than fentanyl (95%); and Zofran is also hepatic with the least protein binding but still over 70%. All 3 are liver damaging–this explains the liver damage they have found and I very seriously doubt that it was cancer. All three drugs are excreted renal–this explains the high CO2 level since his electrolyte was completely out of homeostasis and he was experiencing dehydration.
All three drugs modify serotonin in some way and Fentanyl and Sertraline alone each can cause serotonin syndrome. Combine the three and for sure he had serotonin syndrome.
Since they said that he had endocrine liver cancer, that is a metastatic state of the liver from cancer elsewhere, so the primary cancer would have had to have been the bone cancer or perhaps a third cancer they have not diagnosed. Bone cancer is extremely painful from the very early stages on so it is very hard for me to accept that he was not in pain with a bone cancer! Liver cancer, in addition to the yellowing of the skin and the whites of the eyes, also comes with extreme fatigue. Based on your description of your father joking and feeling well in the ER, I am having a very hard time seeing him with 2 types of cancers, one that changes appearance and stamina and the other that causes extreme pain. It does not add up.
It would have been very painful for you to get an independent autopsy I am sure. However, the findings the hospital presented you with do not line up well with me at all. Furthermore, knowing that it is not in the interest of the hospital to tell you that “oops we goofed up,” your chances of finding a true cause from the very hospital that caused his death is highly unlikely.
I am very sorry about the death of your father and I hope I did not ignite further pain–that was not my intention only I feel that knowing the truth may help closure. It helped me when I received the autopsy I ordered independently from the hospital and found out that my mom had no Alzheimer’s at all. It does not change the outcome but it changed me.
I wish you all the love and comfort I can over the internet! <3
Angela
In 2013, my Psychiatrist changed to a new antidepressant Fetzima. I was taking Trazadone in combination with clonozapam for RLS. My pain management doctor wanted to take me off of 5-300 hydrocodone and put me on Tramadol, and I would have taken it if I didn’t have an appointment with my Psychiatrist the next day. He said it would give me serotonin syndrome and provided me with a printout that showed this to be true. But right below Tramadol was Trazadone and I told him those symptons listed there were what I had been having for several months. Excessive sweating, extreme agitation, inability to handle the slightest stress (felt like crying), loss of balance and coordination, and high blood pressure. I told my pain doctor I could not take the Tramadol. When the medicine was stopped (Trazadone) stayed on Fetzima the symptoms subsided. However, I never felt quite the same, very easily upset and wanting to cry at the slightest thing. Then in 2016 of this year my pain management doctor prescribed me Pentazocine/Naloxone and I had switched to Viibryd for depression. The unfortunate think about Serotonin Syndrome is that when you are the person suffering from it you don’t know its happening until a few months because the symptoms creep up on you and I thought I was just not getting better from the first time I had it. Several months went by and I started having increased pain, severe tremors in my fingers and hands, insomnia, but the severe sweating didn’t start until the last week. When I recognized that I looked up the new pain medication and sure enough it was marked as a major side affect for serotonin syndrome. I stopped taking it and within 3 days it was like a dark cloud had been lifted off of my head. Initially I felt a sort of euphoria, but now I am still easily angered and upset. My pain doctor said he didn’t believe it was serotonin syndrome at all, but opioid withdrawal. I just put my head down on the doctors table because I knew opioid withdrawals happen within 24 to 72 hours, not over a seven month period. He said I was on the verge of a nervous breakdown and he was certainly correct about that but not the reasoning behind it. He now wants me to take Naltrexone 1MG low dose treatment for pain. In addition, he had previously prescribed me Nucynta 50mg, Buprenoophine 2MG, for pain, both of which are marked as major serotonin syndrome when taken with Viibryd. I have just returned from a three months leave of absence from a job I used to handle quite easily, only to struggle with every little issue that pops up. I am afraid I am going to just quit going to work and lose my job. I am going to stop taking everything, but I am afraid I have been permanently damaged and that I will never feel good again. Is this possible?
Dear William,
Thank you for your note and write up. It is truly a miracle that you are with us so time to celebrate for that a little and come out of depression since you could have died an agonizing death and here you are, looking for solutions! I applaud you for that! <3
I have a question or two: you mention pain doctor but not what kind of pain you have. Some forms of pains (like migraine) can be treated without medicines very successfully so if that is what you have, you may want to give that a try and join my group. If by pain you refer to anxiety, nervous breakdown and depression, I recommend you try to change your diet to be “depression and anxiety friendly.” It is now well understood how sugar works the brain into anxiety: it first activated the dopamine system to make you feel good, releasing dopamine and then once you run out of sugar “on the brain” your brain releases adrenaline and THAT causes anxiety.
So by stopping sugar, you can intervene in the depression/anxiety creation process and prevent it–or at least get on the right road to be able to manage it or deal with it. Whatever permanent damage you may have had from the medicines may or may not be permanent–it is dependent on your age and damage type and damage strength. There are ways to “change” the brain and repair it. First you need to stop all sugar and refined carbohydrates, which irritate and cause damage (as noted above) and then get on brain repair:
From the much literature and my personal experience (as a migraineur, I also fight anxiety though not depression all my life, since age 19 actually), I found that the simple task of reducing carbs and increasing animal fats in my diet completely changed my brain. I no longer experience any of the typical anxiety, etc., and also am migraine free (I don;t take medicines either). It seems that so far everyone making this diet change benefited greatly and studies are now under way to use a rather strict therapeutic version of this nutritional approach (ketogenic) to literally cure many CNS disorders, such as depression, Parkinson’s, MS, migraine, seizures (for that it is already used as treatment!), cancer (also used as treatment), and type 2 diabetes (also used as treatment), and some more like autism where research just started and great strides have already been made.
It is best to work this nutritional approach under the supervision of a specialist because in my opinion many people are doing it wrong–but experts are hard to find. You are welcome to join my keto mild for migraine group, which has an expert team connected to it whom you can hire (I am not affiliated and don’t even know them, only a member found them and used their services), which is a learning group and sharing of experience group on how to “fall into” the ketogenic nutritional approach without getting hurt.
I hope you find these helpful.
Best wishes,
Angela
My 20 year-old son DIED from serotonin syndrome in a rural hospital. They didn’t know what he had; didn’t know how to treat it.
20 years old — he should have had his whole life ahead of him.
Oh wow! I am so sorry to hear this! My heart goes out to you! <3
Hugs,
Angela
I am trying to find a clinical pharmacologist or neuroscientist to review my late partner’s autopsy report, medication history, and adverse reaction
history to see if the there is a cause and effect situation.
I need an expert for the Coroner to be able to get reports from.
My partner was diagnosed with dementia after being prescribed some very
strong anti depressants in 2010. The symptoms of the dementia diagnosis
were the same signs of adverse reactions to the drugs. The doctors at
the time knew that he was super sensitive to medications and testified
to his sensitivity in family court in 2012. He was diagnosed with
Prostate cancer in 2009. He chose to treat this homeopathically, very
sucessfully while he was allowed his homeopathic treatment.
MRI, SPECT and CT scans in 2008, 2009 and 2011 all showed no
deterioration in his brain, no vascular disorders anywhere. A CT scan in
2011 showed prostate cancer and bladder diverticula, among other things.
Bryan was prescribed the following medications between 2010 and his
death in June 2014:
Mirtzapine, Venlafaxine, Temazepam, Ibuprofen, Clomipramine, Lorazepam,
Clonazepam, Midazolam, Fludrocortisone, Madopar, Risperidone,
Olanzapine, Donepezil, Scopolamine, Epilim and Paracetamol and Oxybutynin.
Combinations of medications: Mirtazapine and Venlafaxine (2010 – 2011);
Lorazepam, Clonazepam and Ibuprofen (August 2011); Madopar, Risperidone,
Clonazepam, Fludrocortisone, Oxybutynin (Oct 2011 – May 2012) ;
Donepezil and Epilim (Dec 2011 – Jan 2013);
Bryan experienced several episodes of delirium, and at one point I was told he had drug induced parkinsons. Having done a spreadsheet of his medications and adverse reactions, I have often wondered if he had developed Serotonin Syndrome. I am absolutely sure that the dementias found at autopsy are drug induced.
Bryan experienced significant side effects to all these drugs. Some of
the side effects include hyper sedation, peripheral oedema, aggression,
on off effect, falls, urinary tract and bladder infections.
I need an expert to review my material and be prepared, if they agree
that there is cause and effect between the drugs and conditions found in
Bryan’s autopsy report.
I have contacted a number of specialists in New Zealand and Australia
and no -one will help me. This investigation fits beautifully into the
study that Dr Hamish Jamieson is doing and I contacted him, but never
got a reply.
Dear Sally,
I am very sorry about what happened to your partner. I hope that the report contains all information about the necessary findings to tell what happened. To tell if your partner had no Alzheimer’s type dementia is not extremely hard since that disease changes the brain’s structure to the point that is visible in the scanner–not sure if they had taken and MRI of his brain while alive, close to his death. If yes, the autopsy report and the MRI combined can help determine if he had Parkinson’s type dementia but not necessarily if it is drug induced if they find it. They can merely see if he indeed had that.
Regular dementia (not Alzheimer’s) does not necessarily show changes in the brain. Some studies show that plaque buildup (the very thing considered to be the hallmark of dementia) is either present or not; there is no association (causal or otherwise) with dementia and plaques.
I don’t know how old your partner was; age also matters because dementia shrinks the brain. Brain shrinkage is an expected feature of the aging brain but not in the young. The information I am providing to you here is not an evaluation but so you can see that even the best of experts in the field may not be able to help you if you don’t have the CNS (brain and spine) examined by an autopsy including all that is necessary and if you don’t have MRI records.
To find a good expert for the analysis, your best bet is likely in a medical teaching university, or, if you feel that a district attorney would take the case on as a criminal act, he/she will have experts on the stand looking at the records to decide if your partner had dementia of any kind or not and if the cause can be determined.
When my mother died, I donated her CNS to one of the best known teaching universities where I live to do the autopsy and I specifically asked them to check for dementia. I was told that the equipment needed for such is very specific and needs to be handled by a specialized coroner who has such–likely a criminal investigator’s chosen coroner. But even then, showing that the dementia is caused by the drugs may only be possible if an MRI shows that prior to drug treatment his brain was such and after drug treatment his brain became such and the time passed was too short to have ended up with such high level dementia. It is a battle that we have to fight against huge waves also because too many people are labeled with Alzheimer’s disease for convenience sake simply because the symptoms of many other diseases, such as serotonin syndrome, present identically.
In my mother’s case, she was labeled with Alzheimer’s disease and that could immediately be excluded since neither the MRI nor the autopsy showed any deterioration of the kind in the brain that would indicate Parkinson’s.
It is a sad state of matter that I cannot help you any better. I am not familiar with experts in the field who can or are willing to give such analysis myself.
Best wishes; my heart goes out to you.
Angela
Hi
I am very sorry to hear this but also glad i found it. I am sorry for your loss and all through the stupidity of some medical professionals. My sister is going through the same situation as your mother. I don’t recognise her anymore – she is like a whole different person. Her mental health doctor has prescribed: zoloft 200mg, serequel 100mg morning and lunch 50mg dinner and a slow release bedtime, valdoxane 1 tablet at night. Pluse valium 5mg 3 times a day and morphine for pain and NAC 3 tablets in the morning and 3 at night.. Also heart medications. In the last 2 weeks she has stopped zoloft and valdoxane and is now on something new. She has collapsed and sick since yesterday (02/04/2016) and now when she rang her mental health doctor she said she has “Serotonion Syndrome” and to stop everything except valium and go to hospital if she gets worse. How can a doctor prescribe 4 different types of mood stablizers like that? I am so angry. She is a whole different person. I don’t know what to do.
Hi Roxanne,
Sorry for the late response, I just found your comment now by accident. I am very sorry about your sister! I have an answer for your question but it is not appropriate to write it here. I think you know what my answer is based on my story about my mother and my experience with her doctors as well as the many members I help in my migraine group, many of whom come to the group with over 20 medicines all prescribed by the same doctor. The “nice” answer is that they get paid by pharmaceuticals to prescribe medicines so they prescribe, need it or not. Not all doctors are like that! Unfortunately many are!
Best luck for your sister and I hope that she is going to recover fully! She had a competent doctor who recognized it!
Hugs,
Angela
My daughter was diagnosed with serotonin syndrome her frst day of 3rd grade and taken of zoloft. She has Asperegers and an anxiety disorder. She would get excruciating abdominal pain, her face would flush and she would start sweating. As things got worse,she would develop Nero symptoms -eyes not tracking, could talk but not understand what you said,got really loud, lost muscle and urine control at times,and had an irregular heart beat. These episodes lasted about 3 minuts after which the flushing gradually receded and the abdominal pain lessened. Her pediatrician said there was no test for serotonin syndrome but if she tested negative for a bunch of stuff and the episodes stopped when SSRI’s were stopoed,then by process of elimination, she absolutely had serotonin syndrome and it was essential that she never took another SSRI.
Question 1- Are there tests for serotonin syndrome. He is very open minded and would research any information we gave him.
Her pediatrician sent her to a pediatric neurologist who diagnosed her with abdominal migraines with attendant seizures. She said stop the migraines, and the seizures would stop too and focused on migraine preventative medications to no avail. Some of these meds we stopped and refused to give her due to the side affects. Her episodes started getting predictable, about every 26 days. She started her periods at age 11 and as predicted, her abdominal migraines gradually stopped. She is 13 now and out of nowhere, she started getting abdominal migraines about day 6 of her periods every month. This week, about halfway through her cycle, she had tworked abdominal migraines with flushing on Tuesday, 3 on Wednesday, 6 yesterday, and so far, only 2 today but had a seizure with the 2nd one.
The only things we have changed are 1, Reducing her Vyvanse from 60 mg to 10, and 2, drinking alkaline water. Her only other medication is .1mg clonadine 2x perday and an antihistamine at bedtime.
Question 2 – Could the medication change or alkaline water have affected her serotonin syndrome?
Question 3 – Any ideas?
Hi Sheri,
Sorry for the delayed response but I am out of the country with limited internet access so responding from my phone; please excuse typos.
Sorry to hear about your daughter. Unfortunately there is not one test that can conclude that your daughter has serotonin syndrome. Here is a link to what can be done to at least exclude the chance that she may:http://www.mayoclinic.org/diseases-conditions/serotonin-syndrome/basics/tests-diagnosis/con-20028946
In general, some of the symptoms you describe fall into many categories so it is really only possible to tell if she slowly comes off the medication (cannot just stop else she may end up with seizures) and see if things improve.
On the other hand, there is an ancient diet used to treat seizures and now experimentally also autism: ketogenic diet. It seems to resolve seizures over 90% of the cases. My personal opinion is that the ketogenic diet helps because the brain is over 70% fat and our modern diet is low fat. So the brain cannot make the necessary repair. The ketogenic diet for children with seizures is about 80 – 90% fat and the remaining small percent is protein and carbs.
This diet also works for migraines and many other brain conditions. It is my finding that carbohydrates are very destructive to the brain and especially so for those who are glucose sensitive. People with seizures and migraines are glucose sensitive. There us a strong correlation between these conditions and metabolic disorders.
So I recommend you consult with a ketogenic expert and try that method. I personally find that members with migraine do extremely well on a less strict version of this diet that I call keto mild. It will be detailed in my next edition of my book.
In terms of alkaline water: I am personally very much against that. Each of our organs requires a specific pH level for health. Saliva, for example, needs to be slightly acidic to protect against incoming bacteria and also to help predigest our food. Making a body too alkaline makes the body vulnerable to infections. Please check with a medical professional (not a naturopath) about the acidity level needed for your child to remain healthy.
Hope I managed to answer with few typos by phone.
Hugs,
Angela
Thanks Angela. This is very helpful.
I am surprised that nobody has mentioned thiamine in this series of comments about serotonin syndrome. Serotonin turnover has been investigated in regional brain areas of rats made thiamine deficient. It induced an increase in endogenous five-HIAA and impaired five-HIAA efflux from the brain. Thiamine deficiency produces the same symptoms as mild deficiency of oxygen (pseudo-hypoxia) that include anxiety. It is therefore more likely that taking an SSRI would precipitate serotonin syndrome in somebody that was deficient in thiamine. Thiamine deficiency is easily induced from the high sugar intake that is so common in America.
Van Woert M H, et al Effect of thiamine deficiency on brain serotonin turnover Brain Res 1979; 179 (is 1): 103-110.
Thanks for your comment Derrick. You provided a very much appreciated comment. It was not added because it is complex and I tried to keep the article as simple as possible. This medicine does cause hypoxia in lab animals. It is likely to cause the same in humans. I see blood test results from many of my group members and some show enlarged red blood cells, which is an indirect measure of this hypoxia effect that was overridden (or tried to be) by the body by increasing red blood cell size to allow the cell to carry more oxygen. After these migraineurs stop they medicines (like voltage-gated calcium channel blockers, voltage gated sodium channel-blockers and serotonin medicines) they end up with enlarged red blood cells. It is yet to be seen if the red blood cells revert to regular size after some time of recovery. It is too soon to tell since most of the members in my group who stopped these medicines had done so less than 6 months ago–it takes a long time to quit these medicines by titrating down very slowly. Plus the body’s recovery is also slow and age dependent. It will be interesting to see if the body is resilient enough to change the bone marrow’s instructions in producing regular sized red blood cells.
Thank you for you constructive comment!
Angela
Wow thank you for your article. Like so many of your other readers I am currently recovering from SS WITH NO DIAGNOSIS OR TREATMENT HELP FROM MY SO CALLED DR WHO SIMPLY DISMISSED ME. THANK GOD FOR THE INTERNET AND YOUR ARTICLE FOR KNOWLEDGE. There will now be better days ahead. My experience actually was very similar to your moms except that I was able to educate myself and make changes that I believe saved my life and sanity. Thank you again for standing up for the little guy and saving lives with knowledge.
Dear Linda,
Thank you for your kind note. I wish you all the best in your full recovery! I hope many people taking serotonin medications woudl read this article–including doctors.
Best wishes,
Angela
One other thing I would like to share with you Dr. Stanton… is that neurotransmitter and hormonal imbalances are the direct result of mineral imbalances within our bodies. These imbalances are due to the hugely increased stress of modern life combined with food sources with depleted mineral content from insecticides, pesticides and agribusiness practices. The result of this combination is mineral deficiencies and imbalances that put a great deal of stress on our bodies, affecting the endocrine systems especially. Minerals are the building blocks our bodies use. For instance, magnesium alone is responsible for over 3000 enzymatic reactions in our bodies. Ceruloplasmin, a protein produced in the liver is responsible for excreting excess metals like iron and copper, but most of us are very deficient in it, and as a result metals like copper and iron become dysregulated and stored due to low cerulosplasmin status. I mention all this because it is truly the underlying cause of neurotransmitter dysregulation as well. A lot of research is available on mineral and metal dysregulation… and Morley Robbins of the facebook group called the Magnesium Advocacy Group (he has branched beyond magnesium exclusively now … his research has uncovered the profound health effects of iron overload and copper overload) where he shares his findings and has developed a protocol to raise ceruloplasmin and balance minerals … he is not the first to work with mineral balancing obviously, many others have come before him, such as Rick Malther, etc. Anyway, I just wanted to bring this information to your attention. Some books you might find interesting are the Magnesium Miracle by Dr. Carolyn Dean and The Calcium Lie II (which covers much more than just calcium) by Dr. Robert Thompson.
Thanks Carol. I am quite familiar with the names and the books. I am also very much in agreement with you on mineral deficiencies and must add that in the migraine group (that is my main focus for now) I start by removing everyone from all vitamins and metals and herbs and send each for blood tests to check what (if anything) they are deficient in BUT everyone gets instructions to take magnesium. We also found a website that explains which magnesium does and what and everyone takes magnesium according to their condition. On one of my website where I keep some of the testimonials from migraine members (you find it here: http://stantonmigraineprotocol.com/testimonials/ ) you can see that since every person takes different magnesium based on need, significant improvements are achieved in heart condition as well as brain and whole body.
In terms of general mineral imbalances: yes, my book “Fighting The Migraine Epidemic: How To Treat and Prevent Migraines Without Medicines – An Insider’s View” is specifically discussing one key types of group of minerals: those that make up our electrolytes.
I just published an academic journal article on what actually happens when migraineurs start to balance their electrolytes that is publishing in Volume 11, issue 2 of the Journal of mental Health in Family Medicine and can currently be found here (it may move):
http://www.mhfmjournal.com/abstract/migraine-cause-and-treatment-0.html
In this article I explain how migraines respond to proper electrolytes: they vanish. It is that simple. Thus to provide support to your suggestion: indeed, I would think that a very large percent of our diseases (both of the body and that of the mind) are the result of our poor diet, too much sugar, not enough proper minerals and water. I am in full support of your argument!
Hugs,
Angela
Wow… So impressive Angela! I am so happy to hear of all the knowledge you have amassed regarding magnesium, other minerals and electrolytes and that you incorporate it into your protocols for migraines. Minerals and electrolytes are so foundational to our health but it is amazing how they are so ignored in the mainstream med community for the most part. I look forward to reading your links and learning more!! I still get a little confused about which magnesium type is best for what, so I look forward to seeing that info… and will share in the files of the MAG fb group. Best to you. I will be following your work!
Thanks Carol. I actually published an academic journal article on the subject of migraines and the need for minerals just recently–it is still in press but can already be accessed. This particular article focuses only on a limited number of minerals and magnesium is not one of them becuase of limitations of space and the required explanations but it helps you see the connection of migraines and the importance of minerals. It also shows you why the medical community has been blind to this for so long. I hope you enjoy it:
http://www.mhfmjournal.com/abstract/migraine-cause-and-treatment-0.html
For some reason the supplementary material is not included in the article but is available upon request.
Angela,
I have been seeing a doctor trained in “functional medicine” and when I asked about the minerals, his reply was that they did NOT learn anything about them!! I was flabbergasted!! He seemed to only know about fatty acids and aminos, etc. He and another doc with an online newsletter did not seem to realize that SOME people cannot convert betacarotene to Vitamin A since they are missing some components for that process!! It seems like we are quite a bit on our own with dealing with our health (of course, I was sick when I was 12 — now 69 — so I am USED to finding my own answers from literature)!!
I recently made a comment to a doctor (turned out she was a naturopath in an admin position) that if the medical community would only take proper care of the older generation there who not be any need for them to seek “euthanasia”!! Older people can be functioning participants in our society. Two of my aunts are over 90 and still contributing and very lively — the older one still plays bridge and treated herself to a 90th birthday present by going to the track in Los Angeles and riding 6 laps at 175 mph with a racing driver!! Now she talks about going again!
Angela,
Thanks for the article — as I was telling Carol, I take high doses of tryptophan in the winter. I have had some of my minerals tested and generally those that are high in others are low in my body. My zinc and copper were low despite taking high doses (then I found out that I had celiac disease — NO formal diagnosis since I had stopped eating wheat before the doc did the gliadan test — SIGH!!) I cannot seem to tolerate any “grains” — even quinoa gives me diarrhea and then I absorb even fewer nutrients and minerals from my diet. I do a lot of reading and searching (really enjoy Hormones Matter) and feel it is possible that I have a pyrrole disorder since it need to take a LOT of minerals and B vitamins to feel “normal”. I am taking some magnesium (and had some gel to apply to the skin but can’t raise any response from the supplier at this time)and will pick up a more absorbable form today. I mentioned to Carol that I have Sheehan’s syndrome so many hormones need to be checked and balanced and finding the right practitioner is really difficult where we live!
Thanks again for the article!!
Gloria
Hi Gloria,
You sent chills through my veins reading about the high doses of tryptophan. While it is an essential amino acid that we must consume, serotonin, and all triptans (hence the similarity in the name) are derived from it. High doses of it CAN cause serotonin syndrome! I usually ask everyone to stop taking this supplement in my migraine group because they take many other medications and so this can cause SS plus other undesired interactions.
One of the reasons why you are likely having trouble absorbing minerals and vitamins from your food is because Celiacs have a damaged intestinal and gut lining. It is very difficult to find food that you do not make on your own that is without some gliadin protein (or some other proteins that are part of the gluten family). I am not a Celiac and also tested negative to all grains (for the same reason you did… stupidly stopped grains many weeks before the allergy test… duh) but, to give you an example for a non-allergic reaction of someone who ate bread and grains all her life with no problems, after stopping all grains I ate hash browns inn a restaurant last Sunday and boy did I pay for that! And I had no clue I was sensitive (not allergic apparently and clearly not a Celiac) but the price us sensitives pay is
1) inability to absorb nutrients even from pills;
2) lack of proper gut flora for absorption of nutrients in general.
Thus it is not enough for a Celiac to go grain free. A Celiac must also take a good 2-3 months of probiotics until the proper gut flora is established–normally probiotics is enough for a week or 2 weeks max but for Celiacs the damage is so great that the bacteria cannot even establish fast enough well enough. It is totally pointless for most people to take vitamins – I had that tested in my migraine group with B-12 as someone just had a blood test after taking B-12 pill and had been taking it forever and was still low. Monthly injections of B-12 are recommended. I am not sure about the rest of the vitamins and minerals. Magnesium comes in many shapes and forms and given your status as a Celiac, your absorption will greatly depend on what magnesium is best for you.
Some time ago I found this page that gives a very good explanation of the top 10 magnesium types (both good and bad) so you can see which may be the best for you.
http://www.naturalnews.com/046401_magnesium_dietary_supplements_nutrient_absorption.html
However, a word of caution: magnesium citrate has the highest bio-availability but it is also a laxative! Given your Celiac status I would avoid that particular kind of magnesium.
I hope this is helpful!
Angela
Carol,
I often seem to have the OPPOSITE “reaction” to meds and some supplements — I have been taking Tryptan (tryptophan) for about 20 years. The first sample that I tried, I told my son that I felt “ambitious” enough to feel like cleaning the fridge and the stove at the same time. He told me to rest till that feeling passed which did not take long at all.
I have Sheehan’s syndrome so my hypothyroidism is problematic and I also have severe seasonal Affective disorder (we are in Canada in the central prairies so not much sun for about 8 months of the year).
I have read several times about Serotonin syndrome (because it do take high doses of tryptan — the bottle says 8 to 12 grams per day and I have used that high a dose in the winter — but down to 2 grams during the summer now that I am sunbathing). So I am somewhat concerned about serotonin syndrome, but do not seem to have ANY of the symptoms (my digestion is poor — celiac– and I do not absorb well at all) that are described in the literature (except maybe for higher bp and heartrate — I will be 70 next year — which docs attribute to my thyroid meds). I am able to “regulate” my dose of Tryptan by watching how I interact with others. If I get too talkative (like someone who has had too many alcoholic drinks), I cut back on my tryptophan. I am also taking Magnesium and have looked at Carolyn Dean’s info.
May I please make a suggestion? Defining serotonin syndrome in the opening paragraph would be very helpful to those of us not familiar with the term. Also, if I understand the article correctly, everyone who is taking an SSRI, which inhibits the reuptake functioning, will by definition develop SS? Is that what you are saying? If so, very vast implications. I am really glad to have read this article because a good friend of mine is caretaker for a 100 yo woman who displays many of the behaviors your mother had when she switched to the SSRI. I will share this with her. Thank you!
Thanks Carol. I considered doing that (up front explaining what SS was) but then I changed my mind because I wanted it to be emotional and it is a very emotional story for me. I cried my way through the article because of the loss of my mother and how I lost her. So it is also filled with typos but I decided to let it go since it reflects what it is like to witness someone with SS and feel helpless more than coldly tells you facts.
Not everyone gets SS from one SSRI and I see many people in my migraine group who take more than 3 types and are still OK. One never knows when the threshold will be crossed. Because serotonin builds up in the brain with the assumption that it is needed, if it is not needed and builds up to toxic levels is when the problems show up. This threshold is different for each person of course. It is also dependent on what one does during the day.
Only a small amount of serotonin is needed in the brain and how much is used versus how much is made is individual. However, if the 100 years old person exhibits three of the above list of symptoms (the three of these symptoms is as per NIH that you find here:
https://www.nlm.nih.gov/medlineplus/ency/article/007272.htm )
I recommend that you print the instructions out on the link above and hand it to the medical staff/care taker of that old lady and that they stop serotonin immediately and follow the protocol for treatment. I see you have some other comment as well. I respond to that separately.
Hugs,
Angela
I am so sorry that your poor mom suffered in this way. To go from such a thriving life and bright mind to depression, anger and confusion that could have been alleviated must have been devastating for you and especially when you knew what was going wrong. My mom fell and broke her ankle at 81… and it was the beginning of the end for her. Her medical mismanagment was so frustrating as well… she developed IBS and her gastroenterologist did nothing to alleviate the horrible symptoms. It is what eventually killed her 6 mos later, and I now know it could have been treated. After her death I learned that her long term endocrinologist had so mismanaged her thyroid treatment following its removal that the last 25 yrs of her life were needlessly horrible for her; it actually destroyed her life. I of course had no idea at the time about the thyroid treatment being so wrong…. it must have been even more heartbreaking for you to KNOW what was happening and yet no one would listen. My personal feeling is that doctors tend to view the elderly as about to die in general and so they just want to make as much money on them as they can. Harsh view of things, but I saw so many things that convinced me of that. Thanks so much for explaining a bit more about how SS works. I will definitely forward this link to my dear friend Dee who is her caregiver…. right now. So take some comfort that your heart-breaking story will help others. Blessings. Carol
Carol,
I am so sorry to hear that your mother’s thyroid problem was not handled appropriately. My mom was in the same boat — We are in Saskatchewan in Canada and sometimes I wonder about the medical care. It seems like for the doctors — ANYWHERE in the lab range is just fine but IF one reads the literature for many lab results the best levels are in the middle or the “upper” range. That is not true of the TSH lab range — one doctor commented to his patient that if one was hooked up to an IV that gave the optimal thyroid hormone levels — the TSH SHOULD theoretically be 0.00! AND the endocrinologists here wanted mine to get to the middle of the range!!?? And I have Sheehan’s syndrome so my pituitary is just limping along and not working that well. SIGH!! We do so much need to learn and be our own advocate. Yesterday my doctor wanted me to add an antidepressant to my Tryptophan prescription because of my “anxiety” — I told her that my “anxiety” is because the doctors are not being helpful for my situation!! AND then she screwed up my prescription — ordering the “summer” dose instead of the “winter” dose!!
I have had Serotonin Syndrome 2x. The first time my primary care physician was titrating me off of one SSRI and titrating me up with another SSRI. I was rushed to the hospital from her office. I spent 3 days in the hospital. I was given epinephrine in the ambulance and benadyril. I was then sent to the ICU. I was on Paxil and serzone..not one doctor that came to check me out had a clue. I am also a chronic daily migraine suffer. The next time I had serotonin syndrome my new PCP sent me to a poor excuse of a psychotherapist. I was taking Celexa and he decided to prescribe trazadone to help me sleep. I will never forget my husband drove me to see the doctor as I had many of the symptoms mentioned in your article. I had a window to be treated and stopped. Instead the doctor asked me to leave the room for a moment he wanted to speak to my husband. The long and short of this story the doctor told me I would not be thrashing on the floor. I would be fine. Three days later, my husband drove me to the ER where my 11th neurologist met us. I don’t recall the ride to the hospital. My dear neurologist knew exactly that I had serotonin syndrome. I once again spent 3 days in the hospital. Bags of Benadryl, an MRI an extensive neuro. exam every day. Needless to say, I am still battling Chronic Daily Migraines Depression, Fibromyalgia and on my 15th neurologist. I am educated now. I hope I may send your fine article regarding Serotonin Syndrome to my 15th neurologist. Thank-you and God Bless. Jean
Oh my goodness Jean-Marie! I felt my blood pressure rise as I read your comment here! Not one of them treated your serotonin syndrome correctly! It is a miracle that you are alive! My gosh. Glad you are with us!
I hope you are not on any serotonin medicines anymore. If you are not already in my migraine group, please join! There is much we can do to help you. Please ask to be let in and remind me of your comment here so I know who I am talking to. I am just cleaning the group out of people who are there for decoration but we are still close to 2000 so I do not know if you are in or not: https://www.facebook.com/groups/219182458276615/
Looking forward to trying to help you as best we can!
Hugs,
Angela
Thanks for commenting on this article. I take large doses of tryptophan and my doc wanted to add an antdepressant and I refused because I have been on this medication for almost 20 years and am able to tell when I am getting too much — I get TOO talkative like someone who has had too many alcoholic drinks. BUT I often have the opposite effect from medications — tryptophan is supposed to make a person sleepy/relaxed and I get “energized” which is what I need since I also have Fibromyalgia with the main symptom being FATIQUE — AND maybe that is mostly hypothyroidism like Dr. John Lowe talks about in his book The Metabolic Treatment of Fibromyalgia. His info seems to apply to me — he talks about thyroid hormone “resistance” and I am not sure what exactly he means by that but I likely have it.
Jean-Marie, I hope that you are NOT still taking that Serzone — it was supposedly pulled from the market because of causing liver damage. I was on it for a bit over a year and my stools got paler and paler. The pharmacist called to tell me to dump that med but I never heard anything from the doc who prescribed it and at the time didn’t know that I was getting liver damage from the Serzone!!
Gloria,
I am also working on fibromyalgia and have a group specifically for that but it is still very small.
https://www.facebook.com/groups/738392076228348/
Many of the members in the FM group are also members of my migraine group and use the migraine protocol. It apparently benefits them though does not “cure” the disease. However, I have a few ideas (I am always full of ideas for better or worse) and so I want to ask you a question: Have you had Mononucleosis or any other types of encounter with the herpes virus, like a cold sore or similar, when you were a child?
Angela