Every now again, I stumble upon research that upends my thinking about a particular topic. Over the last few months there have been three such articles that point to metabolic factors in the development adenomyosis and endometriosis. With adenomyosis, endometrial tissue grows aberrantly in the muscle wall of the uterus, a region called the myometrium. With endometriosis, endometrial tissue can implant itself virtually anywhere in the body. Both are incredibly painful, affect millions of women, and to date, have no known causes or effective treatments. I would like to review briefly some of that research here, as I continue to delve more deeply into this topic.
Of Stem Cells and Metabolism
The first was a story posted on the online journal called Quanta reviewing the latest in stem cell research. I dug into the research and wrote about it here. The gist: while genes provide a plan for cell development, and epigenetic variables fine tune that plan, metabolism ultimately determines whether or not, how, and in what location that blueprint is carried out. If metabolism is weak, everything changes, all the way down to whether or not that cell will become what it was ‘genetically programmed’ to become. In other words, metabolism drives genetic expression and cell fate decisions and not the other way around.
Paper two, identified active stems cells in menstrual blood that can be coaxed into becoming just about any cell type including: cardiomyocytic, respiratory epithelial, neurocytic, myocytic, endothelial, pancreatic, hepatic, adipocytic, and osteogenic cells. Not only that, stem cells from menstrual blood, in addition to being much easier to collect than those from bone marrow, the typical medium, they propagate rapidly, doubling every ~19 hours and can undergo up to “68 doublings without losing karyotypic normality or developing tumorigenic potential.” So, that stigma-ridden, presumed waste product turns out to be one of the most therapeutically and potentially diagnostically useful fluids in medicine. I wrote briefly about that research here.
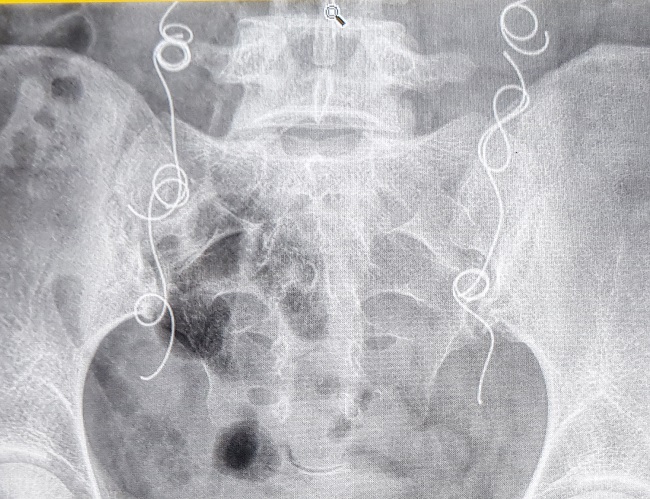
Paper three – women with adenomyosis have demonstrably defunct Schwann cells at the interface between the endometrium and myometrium – a region called the endometrial myometrial interface (EMI). I suspect this is the case with endometriosis too, but have not found any research to confirm – yet. Briefly, the endometrium is outer layer of the uterus, where fertilized eggs embed should there be a pregnancy or that sloughs off monthly when there no pregnancy. The myometrium is the middle layer of uterus comprised of smooth muscle and innervated by adrenergic nerves that contract the muscle during pregnancy or monthly during menstruation. These nerves are lined with a protective covering called myelin. Myelin is comprised of Schwann cells. With adenomyosis, the myelin is frayed and so nerve conduction is problematic and incredibly painful. This is a neuropathy, just like the neuropathies in other nerves, only here it is in the uterus. That neuropathy is an important component of the disease process; one that potentially links the stem cell research and metabolic capacity to adenomyosis and endometriosis. Let me explain.
Connecting Some Dots
Combined, these three articles tell us a great deal about the unending pain some women experience monthly. Firstly, if stem cells need nutrients to become what they are supposed to become and to remain in their genetically programmed region of choice, disorders like adenomyosis and endometriosis that are marked by aberrant tissue growth, in the myometrium with adenomyosis, and potentially all over the body with endometriosis, these disorders are quite clearly driven by regional, if not systemic, and perhaps even genetically reduced, nutrient capacity. Why else would the stem cells responsible for growing the endometrium each month implant themselves in non-endometrial tissue? The stem cell research has demonstrated repeatedly, albeit in different cell types, that poor metabolic capacity, e.g. poor mitochondrial capacity/poor nutrient capacity, determines cell fate decisions. Applied to adenomyosis and endometriosis and we get poor metabolic capacity underlying the aberrant tissue growth.
Secondly, the pain women feel with these conditions, while certainly impacted by the physical obstruction of errant tissue growth or the response of that tissue to monthly hormone changes, may be largely neuropathic, and again, driven by poor metabolic capacity. Demyelinated nerves, wherever their location, causes intense pain. When nerves in the myometrium, those responsible for uterine contractions are demyelinated, the pain will be immeasurable. Importantly, demyelination can be attributed directly to insufficient metabolic capacity. In other words, the stem cells responsible for growing appropriately differentiated and healthy Schwann cells forming the myelin sheathing around the uterine nerves are essentially starving and thus forced to stay in what is called a de-differentiated state. In theory, this could be correctable with the appropriate metabolic factors. The two most clearly involved metabolic variables appear to be thiamine and l-carnitine. I will be exploring these pathways and their implications relative to adenomyosis and endometriosis in subsequent posts. For now though, know that both of these nutrients affect mitochondrial metabolism significantly.
Finally, the stem cells and other molecules sloughed off monthly in the menstrual fluid provide a window in to these disorders. Perhaps more so than any other test diagnostic test, it is entirely possible that by investigating stem cell development in the local environment from which they emerge, we could identify and ultimately correct, or at least support, the metabolic needs for proper cell function. In doing so, I believe it is possible to help millions of women live with less monthly pain.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Photo by David Travis on Unsplash