What Is a Syndrome?
A syndrome is the name given to a collection of symptoms and physical signs that have been observed in the past in a single patient or in a group of similar patients. This is often named after the first person to report this set of observations. It is called a syndrome when others have made the same observations, sometimes years later. The terminology is purely descriptive, even though there may be a constellation of abnormal laboratory tests associated with the clinical facts. Unfortunately, the underlying cause is seldom, if ever, known.
Chronic Fatigue Syndrome
Chronic fatigue syndrome (CFS) is also known as myalgic encephalomyelitis (ME). In a review, it is described as a “challenge to physicians”. Its prevalence is reported as approximately 1% in the general German population. The author states that there are no convincing models that might explain the underlying cause as an independent unique disease. A variety of conditions such as chronic infectious disease, multiple sclerosis, endocrine disorders and psychosomatic disease are suggested in a differential diagnosis. There is said to be a significant overlap with major depression.
Another review describes CFS as characterized by debilitating fatigue that is not relieved with rest and is associated with physical symptoms. In order to make the diagnosis, these authors indicate that at least four of the following symptoms are required to make the diagnosis. They include feeling unwell after exertion, unrefreshing sleep, impaired memory or concentration, muscle pain, aching joints, sore throat, or new headaches. They also say that no pharmacologic or alternative medicine therapies have been proven effective.
Fibromyalgia Syndrome
According to the American College of Rheumatology, fibromyalgia syndrome (FMS) is a common health problem characterized by widespread pain and tenderness. Although chronic, there is a tendency for the pain to fluctuate in intensity and location around the body. Deficient understanding of its true cause gives rise to the false concept that it is neurotic. It is associated with chronic fatigue and patients often have sleep disorders. It is estimated that it affects 2 to 4% of the general population and is most common in women. It affects all ages and the causes are said to be unclear. FMS patients may require psychiatric therapy due to accompanying mental problems. Gonzalez and associates concluded that the combination of psychopathological negative emotionality, interpersonal isolation and low hedonic capacity that they found in a group of patients has implications for the daily living and treatment of these patients.
Regional Pain Syndrome
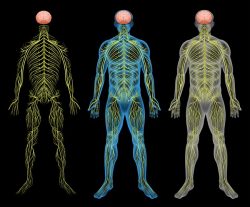
Complex regional pain syndrome (CRPS) is another common and disabling disorder, characterized by defective autonomic nervous system function and inflammatory features. It reportedly occurs acutely in about 7% of patients who have limb fractures, limb surgery, or other injuries, often quite minor. A small subset of patients progress to a chronic form in which autonomic features dominate. Allodynia (pain due to a stimulus that does not usually provoke pain) and hyperalgesia (increased pain from a stimulus that usually provokes pain) are features of CRPS and require a better understanding.
Sleep Apnea Syndrome
Apnea is the term used for a temporary cessation of automatic breathing that usually happens during the night. This syndrome is described as the most common organic disorder of excessive daytime somnolence. Its prevalence is highest among men age 40 to 65 years and may be as high as 8.5% or higher in this population. It is associated with cigarette smoking, use of alcohol and poor physical fitness.
Similar Cause with Different Manifestations
Complex Regional Pain Syndrome is related to microcirculation impairment associated with tissue hypoxia (lack of oxygen) in the affected limb. Without going into the complex details, hypoxia induces a genetic mechanism called hypoxia inducible factor (HIF-1 alpha) that has a causative association with CRPS. It has been found that inhibiting this factor produced an analgesic effect in a mouse model. The interesting thing about this is that thiamine deficiency does exactly the same thing because it induces biochemical effects similar to those produced by hypoxia (pseudo[false]hypoxia). A group of physicians in Italy have shown that high doses of thiamine produced an appreciable improvement in the symptoms of three female patients affected by fibromyalgia and are probably pursuing this research. Dietary interventions have been reported in seven clinical trials in which five reported improvement. There was variable improvement in associated fatigue, sleep quality, depression, anxiety and gastrointestinal symptoms.
Dr. Marrs and I have published a book that emphasizes deficient energy metabolism as a single cause of many, if not all, diseases. The symptomatic overlap in these so-called syndromes is generated by defective function of cellular metabolism in brain. Fatigue is the best symbol of energy deficiency and the English translation of the Chinese word beriberi is “I can’t, I can’t”. Fatigue is a leading symptom in beriberi. When physicians diagnose psychosomatic disease as “it’s all in your head”, they are of course, quite right. However, to imagine or conclude that the variable symptoms that accompany the leading one of fatigue are “imaginary” is practically an accusation of malingering. The brain is trying to tell its owner that it has not got the energy to perform normally and the physician should be able to recognize the problem by understanding the mechanism by which the symptoms are produced. Every thought, every emotion, every physical action, however small, requires the consumption of energy. Obviously we are considering variable degrees of deficiency from slight to moderate. The greater the deficiency the more serious is the manifestation of disease that follows. Death is a manifestation of deficiency that no longer permits life.
Our book is written primarily for physicians, but it is sufficiently lacking in technological language to encourage reading by patients. It emphasizes, by descriptions of case after case, the details of how genetic risk and failed brain energy are together unable to meet and adapt a person’s ability to meet the daily stresses of life. Stress, genetic risk and poor diet all go together. A whole chapter discusses the functions of the autonomic nervous system and how it deviates when the control mechanisms in the lower brain are defective. This system is the nervous channel that enables the brain to communicate the adaptive body actions necessary to meet living in an essentially hostile environment. We show that an excess of sugar and/or alcohol produce deficiency of vitamin B1 and the so-called psychosomatic disease that results is really early beriberi “I can’t, I can’t”. Variability in symptoms caused by this effect is because the cellular energy deficiency distribution varies from person to person and is affected by genetically determined differences.
This is illustrated by the case of a boy with eosinophilic esophagitis whose first eight years of life were marked by repeated diagnoses of psychosomatic disease. At the age of eight, upper endoscopy revealed the pathology in the esophagus. There was a family history of alcoholism and he was severely addicted to sugar. Many of his symptoms cleared with the administration of a thiamine derivative and resulted in a dramatic increase in stature. No pediatrician or other physician whose attendance was sought through those first 8 years evidently had ever questioned diet or the gross ingestion of sweets. They simply treated each condition as a confirmation that they were “psychological”.
It is worth noting that references 1 through 4 refer to both CFS and FMS syndromes being affected by psychological issues. This implies that the patient is “inventing” the poorly understood (and often bizarre) symptoms as a result of neurosis. The unfortunate complainant may easily become classified in the mind of the attendant physician as a “problem patient”. I have become aware that this can rise to such a degree of misunderstanding that the patient is denied access to the physician and even to other physicians in the same clinic. It is indeed about time that an overall revision be made to the absurd concept that the brain can “invent” a sensation that has no importance in solving the electrochemical problem. When we see the statistics of incidence of these common syndromes we have to conclude that there is an underlying cause and effect that pervades the general population. We are very conscious that our cars need the right fuel to work efficiently but rarely take it into consideration that the quality of food is our sole source of energy synthesis.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Image created using Canva AI.
This article was published originally December 2019.











@Dr. Lonsdale & @Dr Marrs. THANK YOU for your dedication to helping a very difficult group of people to work with.
I have CFS and Interstitial Cystitis.
I was diagnosed in 2021. I tried mega doses of COq10 1200mg per day and for 2 weeks and felt amazing and then it abruptly stopped working. I understand that this would of helped the ETC transport more electrons to inturn pump more protons/hydrogen ions and this should result in protein complex 5 making more ATP….well that’s my theory and the limit of my understanding, I just a humble flooring guy not a medical expert.
Then I found Elliot Overton a couple months later and started TTFD shortly after.
I moved quickly to 600mg of TTFD per day along with all the supporting B vitamins and electrolytes (Threonate & banannas for K), selenium, molybdenum, and COq10.
I was 90% symptom free of both CFS and I.C within about a week or two and enjoyed this for 3-4 months then it abruptly stopped working.
Fast forward to October 2022, I had tried water fasting, to stimulate mitophagy, for 6 days and everything was going well until the morning of day number 7 and I felt like absolute crap, couldn’t get out of bed for 3 hours. I knew I had to commence the re-feeding protocol.
2 days later I get a blood test back from my Dr and find out I’m very deficient in manganese, less than 7nmols/L!! Consequently, I investigated what this trace element is all about…..OH. MY. GOODNESS!!
That would explain why the fasting ended so abruptly, I couldn’t metabolise fats or carbohydrates which leaves only protein. This also raises the question in my mind was I deficient in manganese while doing the ketogenic diet in 2019 and was that why I never had energy? Was this the straw that broke the camel’s back and tipped me over into full blown CFS and I.C?
I’ve also learned that the Manganese Superoxide Dismutase enzyme won’t convert ROS without a sufficient amount of manganese. How rare is a deficiency in manganese? Is it common in CFS? And can mega doses of thiamine cause further manganese deficiency? Is this why the TTFD stopped working so abruptly? I suspect I’ve done a lot of damage to my mitochondria. I super charged my ATP production without having the mechanisms in place to deal with the exhaust (ROS).
In 2019 on the keto diet, I ate so many nuts but still wasn’t getting enough manganese and so now I’m supplementing.
Since supplementing with manganese and with the addition of chromium and vanadium I have noticed the following, I’m no longer insulin resistant (BG 5.8mmols/L is what I’ve typically test at for 20+ years, now 4.5-4.8mmols/L after fasting), I do a lot of healthy teflon poos now, my ear wax is no longer flakey or powdery it’s waxy and I’ve had a significant decrease in CFS and I.C symptoms without taking TTFD.
I’ve not been able to tolerate TTFD as well since it stopped working, this could be due to a lack of glutathione, so I am now taking 2000mg of NAC and glycine just before bed. I’ve also recently tried bicarb soda at that seems to have a significant improvement in brain fog and I’ve been able to tolerate TTFD since taking the bicarb soda. I am aware of alkalosis being an issue with bicarb soda. I believe thiamine is supposed to help with the lactate cycle. It’s a challenge not having a medical background trying to learn about so many complex systems and how they all fit and work together and with brain fog and memory loss. two mice fell into a bucket of cream one gave up and drowned the other never gave up and kept fighting till that cream turned to butter and he climbed out, I’m that second mouse.
Hello,
I have emotional flatness, major depression, terrible insomnia and chronic fatigue. After many tests I found via testing of the CSF I have low BH4. However, after a while on the replacement enzyme it seems it’s not absorbing and my symptoms are only worse. After starting the medication, and after dose increases improvement comes but quickly fades the next week. My CSF was also tested for amino acids which came back normal.
Dr. L or Dr. Mars, what should I look to or turn to, to uncover the root of the deficiency or help absorption??
Dr. Lonsdale – Thank you for the terrific article.
One question for you: A nutritionist and doctor I know told me that taking high dose b vitamins has been shown to cause organ hyperplasia/increased organ size. I believe he specifically mentioned this occurs with the liver… though I’m not certain of this. He seemed to be quite concerned about high dose b vitamins causing severe organ size increases and maybe even cancer.
This was surprising to me. Have you ever heard of these sorts of claims? Do they have any merit?
Drs. Lonsdale and Marrs,
I have a question about something that might fall into the “syndrome” category. My 84-yr-old mother has been diagnosed with Normal Pressure Hydrocephalus (NPH) and is slipping quickly into dementia. There is no doubt that she has been severely thiamine deficient for many years; she began her decline with what was labeled as “heavy leg syndrome” (she began to lose use of her legs), diarrhea, and significant edema (doctors said she needed to lose weight–which began rounds of diets that made it worse). She is now losing bladder control. As she does not drink alcohol at all, the neurologist will not consider that this might be encephalopathy caused by thiamine deficiency.
The neurologist was clear that no one really knows what causes NPH. The course of treatment will be to do a spinal tap to see if it relieves pressure on the brain, and then to install a permanent shunt.
She has been taking just 100 mg of allithiamine daily for several months. I was concerned about paradox and wanted her to start slow. It does not seem to be making her worse that we can tell, but no progress either. They are afraid to bump the dose up.
Is it possible the NPH is a result of thiamine deficiency, and overall bad nutrition? There is NOTHING that I can find online that links the two at all. Is there anything specific I could say to the neurologist that might get him to consider thiamine deficiency? Finally, I am considering taking her to a clinic to have a broad spectrum vitamin IV that included thiamine to see what happens, but this would not be with the support of a doctor.
It seems all of the symptoms of NPH are symptoms of severe thiamine deficiency. It is so frustrating for the doctors to refuse to consider this, especially since they don’t know what causes NPH.
As always, thank you so much for your work. I tell everyone I can about your blog and your book.
I suspect that NPH, because dementia is involved, is an end result of brain energy deficit. The work of Dr Costantini in his successful treatment of Parkinson’s disease suggests that the high dose thiamine (4 grams) he used, means that thiamine is being used as a non-toxic drug. It is possible that it is an undiscovered biochemical effect of Th in brain, beyond its enzymatic role. I can’t understand the rationale of a shunt in NPH and I would not hesitate to use high dose Th. Dr C has also treated CFS and fibromyalgia, suggesting that the various diseases are all due to the degree and distribution of brain energy deficit.
Dear Doctors,
I started TTFD 400mg per day since June after having read your book. My main symptom are fatigue, urinary dysfunction (frequency, hesitancy, nycturia), sleep issues, very oily scalp and face, redness, and dry flaky skin.
I added very high doses of riboflavin and niacinamide and my hands are no longer dry, also I don’t need to apply lip balm 3 times per day anymore. Fatigue and urinary symptoms seem to fluctuate, and sleep is still very rarely refreshing.
Skin oiliness and flakiness didn’t improve at all despite my attempt to take high doses of B6 (P5P), zinc, or B5, and it even causes adverses reactions. Could you please let me know if you have any suggestions?
Thank you very much for your work,
Adrien from France
Dr. Lonsdale and Dr. Marrs, I have a quick question for a friend with narcolepsy. He is about 30. While I cannot find any literature that discusses a possible link between narcolepsy and thiamine deficiency, it seems that since the sleep/wake cycles are regulated by the autonomic nervous system that it’s possible high-dose thiamine may help. I have found a couple of articles (but not many) that do say narcolepsy might be caused by ANS dysregulation.
I was interested to read that episodes are often triggered by increased stress, which again would line up well with all of your research.
My question is, would this friend be likely to experience more frequent narcoleptic episodes when he begins to take thiamine? I am concerned that with narcolepsy, “getting worse before getting better” might be dangerous as well as inconvenient. I will print out your articles that discuss paradox for him to read. If my friend does indeed try your protocol and sees improvement, I will post his results here so you can add them to your arsenal of information.
Thank you very much for your book–I have purchased several copies to loan to friends and doctors!
There are several mechanisms of interest that would be impacted by thiamine and influence sleep/wake cycles. In the hypothalamus, there is a set of neurons called the orexin or hypocretin neurons – same neurons, different names – that regulate wakefulness. I have a number of articles on them on the website. These neurons act as an energy sensor of sorts and stop firing when brain energy is low as a way to conserve critical resources. Stress e.g. higher energy demand relative to need, would shut these neurons down, at least temporarily, making maintaining wakefulness difficult. Genetic aberrations to these neurons are involved in many cases of narcolepsy. They can also be damaged epigenetically/environmentally by a number of toxins. As energy sensors though, if we can improve the energy supply to and from the mitochondria we can minimize the episodes. As to whether these episodes will become worse initially, I do not know. The only case of narcolepsy I have worked with did not have a worsening of narcoleptic episodes when she began, but did have other symptoms, tachycardia specifically, that was difficult to manage at first. Everything stabilized after a period of time.
Thank you—I found and printed a bunch of your articles about orexin and narcolepsy. My hope is that he will add a good vitamin supplement, magnesium, and allithiamine; lower his refined carbohydrate intake, and cut out sugar. Maybe that will do the trick. I will let you know how it goes!
Popping in for an update. Have been taking 100mg Lipothiamine, 150mg alternating Mag Citrate and Glycinate, topical magnesium for a few days shy of a month. Added in potassium a few weeks ago because noticed was having cramps. That helped. This has been in addition to full dosage of 12 different Beef Organ Supplements and a vitamin B complex.
I’m dedicated to going for a full two months. I have noticed that anxiety, negative thoughts, and irritability have continued to be high since starting the thiamine. Not super fun and not typical for me, but doable for the time being. I’ll keep at it until the two months are up and reassess then.
I was able to go for a hike yesterday without significant difficulty today, no significant crash, though I can tell I’m a little more worn out than usual this morning. So my PEM from Long Covid seems to have abated. Was already headed in that direction before thiamine, so not 100% sure if the ability to recover from exertion is due to thiamine or not.
Still experiencing significant fibromyalgia pain, some joint pain, allodynia and an overall feeling of weakness…weak muscles. Weather related symptoms still high.
If you have any other suggestions or thoughts, I’d love to hear them. Either way, I’ll keep on plugging away for another 4 weeks and we’ll see what happens!
Thank you,
Lorrie
Keep at it. It requires patience
“Rivers know this: there is no hurry. We shall get there some day.”
– AA Milne, Winnie the Pooh
I’ve just ordered Lipothiamine for Long Covid after reading your excellent work. I had severe ME/CFS for 8 years 20 years ago and I believe, have had FM my whole life.
My main question: I’ve always been extremely affected by weather. I can have all the energy in the world for a day or a week or…ex: teach two back to back power yoga classes, followed by a high intensity interval training workout and then work a full day in my business. And feel fine the next day and do it again.
Unless there is weather coming in. In which case I can’t get up off of the sofa and/or sometimes the FM pain gets so intense during those times. Or if it’s a high pressure system, can’t get to sleep and/or have trouble breathing and/or restless leg. Other various specifics, but that’s the basic idea.
And of course, there’s always weather coming in most places. I currently live in the southeast, so lots of weather here. My energy levels are all over the place. When I lived in Los Angeles, I had much more consistent energy and high energy.
As I said, this has always been the case for me, even when growing up. I didn’t realize it was weather at that point. But I would miss school because of it. Or I’d achieve an incredible amount in a very short amount of time.
We’ve always known that my ANS is funky…I have hyperhydrosis as well. But I have never found any information about what would cause my body to respond so strongly to weather or what I can look into to do to alleviate it. And I have looked and asked…for decades (I frankly no longer go to doctors because of my experience with CFS those 20 years ago…I am my own best doctor and advocate).
Do you have any theories or speculations as to the “why”?
And especially any suggestions for what I can do? Or just the B1 (+mag) protocol?
I’m curious to see if the B1 will even the energy out once I’ve gotten past the Long Covid (it’s mild…no longer experiencing PEM, but still have some lingering symptoms). I would love to hear your thoughts on the weather thing.
PS. I eat a carnivore diet with lots of fatty fishes, fatty meats, egg yolks, organ meats, bone broth, etc. I’m also currently dealing with oxalate dumping and am working on addressing that in various ways. In the past, I’ve eaten protein heavy 90% paleo for 20 years (very few carbs…just never agreed with my body once I went paleo).
Thank you so very much!
I am a great advocate of Hans Selye who researched stress in animals. He published the details of the General Adaptation Syndrome (GAS) that required energy to resist the stress. He said that human diseases were “diseases of adaptation”. A student of his reproduced the GAS by simply making the animal thiamine deficient. Evidently weather is for you a source of “stress” . My interpretation is that you are a high energy consumer and weather makes extra demands. Try taking a supplement of 100 mg thiamine and 150 mg of magnesium a day and see if it modifies the next dose of weather. Let me know.
Very interesting. “Diseases of adaptation.” Your further interpretation completely makes sense to me…for some people external situations or emotions or…whatever…are stressors. For my body (a “high energy consumer”) it’s weather. Therefore I’d need more thiamine during those times of stress. Very cool, Dr. L. First explanation I’ve ever run across that resonates. (Well…first possible explanation anyone has ever given me, really!!!)
I’ve just started 600mg Thiamine HCl because I had it lying around…waiting on the Lipothiamine to get here. Usually take 100mg mag/day, I’ll up it to 150.
Still dealing with residual Long Covid symptoms (including fatigue, POTS, etc), so it may take some time for me to know for sure if the weather issue has been ameliorated by your recommendation, but I’m optimistic 🙂
I’ll let you know, definitely. Thank you for your fast response, for the valuable information and for your very in tune hypothesis!
Thought I’d let you know what my experience has been thus far (also for those who are just starting their Thiamine journey and/or have Long Covid or ME/CFS/FM). It’s still very early on (first week), so I’m not expecting to have any definitive results at this point.
Please keep in mind that 1. The weather has been all over the place, so it’s hard to know what’s weather and what’s thiamine. 2. I’ve also just gotten up to taking full dosages of 12 beef organ supplements, so there’s a lot happening with that as well. Again, not a great way to do an experiment. But when I listened to internal guidance, this is what felt right and thus far it’s serving me well!
3/19: started Lipothiamine 50mg + 100mg mag citrate (take citrate form to assist oxalate reduction) + transdermal magnesium morning and evening. Seemed to feel a good bit better after taking the Lipothiamine. More even emotionally. Still wanting to sleep all day.
3/20 – 3/23: 100mg Lipothiamine 100mg + same as above. Increase in symptoms like peripheral neuropathy, balance issues, POTS, tachycardia, anxiety, etc. Decreased every day.
3/24: Woke up with hands sweating like crazy…dripping. Tells me ANS was doing interesting things! Also recognized that…I’d been taking the B1 + mag first thing in the morning and realized I had more energy before taking it. Started taking it in PM, which is currently the best time to take. Alleviated the feeling like I needed to sleep all day and lack of focus thing. Continued PM for B1 and oral mag here on out.
3/25-3/26 (which is today): Started trading off 115mg mag glycinate (+ transdermal am and pm still) and 150mg mag citrate every other day. Lots of energy yesterday and earlier today…definitely weather related. Had a warm weather spike come in, which is typically much higher energy for me. Now cold front about to come through (just looked) and sure enough, my energy dropped significantly starting about an hour and a half ago.
I’ll continue to update every week or two. Thank you for this wonderful website and for all the information!
Dear dr Lonsdale and Marrs
Thank you so much for your work and for the time you spend to let us know about all this stuff.
I’m young girl (26 yo), I’ve been sick for about ten years: CFS, dysautonomia, low T3 and T4, SIBO, GastroIntestinal problem like delayed gastric emptying. I have olso problem whit weight, I have a tendency to gain weight, I am always on a diet and I eat very well and healthy.
I have also mood swings that sometimes make me feel crazy. I feel without energy in my muscles and I feel I can’t do anything (although above all this I was a girl full of energy and always very cheerful)
After reading your site I was sure my problem was low thiamine, so I started with B1HCl 20mg a day intramuscular 8 weeks ago.
Is it possible I don’t see results (I have read on your website that healing begins between the fourth and sixth week after the onset of thiamine).
I also integrate B12, B2, biotin, myoinositol, magnesium citrate and treonate.
Do you think I may still have thiamine deficiency? (next week I’ll get allithiamine, can’t wait to get started).
According to you I have to integrate something else?
I’m missing a piece of the puzzle.
I really thought I was solving the problems with thiamine, I bought your book too, but I can’t figure out what else I have to do … do I have to supplement the potassium? and the other vitamins? how do I know if my neurotransmitters are working well.
Do you know the problem of under-methylated or over-methylated?
I hope you will read this post and answer me sincerely with your advice
Thank you very much
Thank you for sharing your experience
Thank you for saving life of many people
Goodbye
Claire
Well, of course I don’t know the answer to your question. You certainly have symptoms that I would put down to energy deficiency, but the machinery is very complex. Fortunately, I have found that many people with these symptoms do in fact respond to megadoses of thiamine. But there are many surrounding issues which complicate it, not the least of which is the genetic background. I can only suggest that you try the allithiamiine and magnesium, together with a multivitamin. In some cases intravenous vitamins are necessary and that is subject to a shortage of doctors that understand the principles involved.
Thank you so much for your rapid reply
In the next few weeks or months, I hope to come back here to tell you that I am getting great results and that I am finally recovering.
Thanks for the work you do.
Thank you!
Claire from Italy
I take super high doses (500-750mg) and get dysautonomia/neuropathy results. You might also have other issues that need to be individually resolved, even if they are all related. Check out some of the interviews at https://www.youtube.com/c/drmarkhyman/videos – they’ve been super helpful for me. You’ll get tons of ideas for what to try, how much you need to optimize (e.g. if you’re gluten sensitive, you might need to cut *all* gluten and not just *most* gluten), how drastic your changes need to be, etc. Hope you feel better!
Thank you so much for your reply
I will look at the mark Himan page right away.
I’ve tried a lot of therapies since I’ve been sick,10 years 🙁
I am sensitive to gluten and I agree with you about eliminating it completely (I did the same with milk and dairy).
I am grateful for your comment. Any other advice is welcome
Virtual hug
Claire, Italy
Hello Dr Lonsdale.First of all i wanted to express a huge gratitude to all your work which you have been doing for a lot of years and hope will in many decades.Age is just a number))My question is about my specific case.I also had very similiar symptomes of beri-beri.I have the same cardiovascular case as this man https://www.hormonesmatter.com/functional-dysautonomia-peripheral-circulation/ (cold and blue feet and hands during cold and stress,red feet after running or any other blood circulation acceleration,exposure of vessels net on the backside of my wrist+excessive sweating out of nowhere,panicing and fear even i consciously understand there is no stress to be.These symptomes aggravate in winter.Also i have crunches in my wrist,ankle,shoulder joints and a feel of stiffness and tightness in muscle in the morning.I also have some kind of POTS syndrome when i change my position from horizontal to vertical,for example, when i get up from the bed or stand up from the chair i experience sort of dizziness and can perceive for a few seconds visually.To addition i have cognition problems.I cant very often pick up a words to express my thoughts especially during stressful moments lt looks like 80% of my vocabulary disappear from my mind for a limited period of time,bad memory and focus,unexpected fussiness despite of the fact that i am quite intelligent as well as strong-willed person.I also obtained digestive issues half a year ago,massively reduced them but still have some tention in upper abdominal.Very curious observation that i have quite fit and slim upper body(male),but legs are completely disproportionately thick and flabby,very big hips, tender and wide calfs it manifests more when i hold my leg horizontally.I mention about leg part because most of my life (i am 19 years old now) i have been doing anaerobic sports like tennis and martial arts where legs were involed much more than upper body constituents.I probably had other symptomes but i dont remeber them.So with all of your profound information which your provide hear it looks like i found the last puzzle of my struggles which follow me last 10 years,approxiamtely from the age of ten.I assume that it could be a huge energy loss in my body during thiamine deficiency,i would like to order some TTFD,but i am not sure because i was diagnosed with Gilbert’s syndrome last year and bilirubin increases amount of free radicals in the body which aggravates oxidation and that can be also a factor,so question is whether it can be another source of energy deficiency except thiamine as you write previously as a result of Gilbert’s syndrome,may be implementation of reduced Glutathione can be also reasonable move?Once again highly appreciative to your work)
You seem to be out dated as regards functional neurological disorders (FND). CFS is not FND where CRPS and fibromyalgia are. They certainly are not “Mystery” illnesses and no longer count as “Medically Unexplained” neither are they “all in the head” however you look at them. They are only counted as “Psychosomatic” because there is a malfunction in conscious and unconscious processing in the brain – a great deal of research concentrated on the amygdala at first, but there are other changes in the FND brain.
A great deal more is now known about FNDs largely through the work of Prof Mark Edwards at St Georges, London and Prof Jon Stone at Edinburgh and thankfully a great many more joining in the research of what has been rightly described as a “crisis in neurology”.
Please do the FND community a great favour by becoming better informed. Especially as I believe you and your research could be useful . The symptoms are caused by a build up of glutamate in areas of the brain. Areas shrink and consequently malfunction – people can recover. There is no overlap with non-FND patients. Scans can indicate prognosis and severity of the illness. They also include movement disorders and functional seizures.
I could go on but you could start by visiting FND Hope and neurosmptoms.org
I certainly found that having FND due to a sulfite sensitivity was no fun at all. I certainly feel that nutrition in FND needs a closer look, but as Prof Edwards often remarks “there is no panacea for FND”. I do believe, as do many of the researchers, a multidisciplinary approach is needed and that your input could be of great value, but first please do some updating. FND patients make up 30% of neurology referrals. Over a 14 year follow up 11% of FND patients had died, heart disease being the most common cause (Stone et al).
I saw many cases of what you call FND and virtually all of them responded to megadose thiamine. With so many different symptoms responding to thiamine and magnesium, I had to conclude that all of these “different diseases” were deficient in energy metabolism.
Hi this is what DR JACK KRUSE has to say about B1 and Mirochondria
The conversion of tryptophan (Trp) → nicotinamide (Nam) is an important pathway for supplying vitamin niacin to make NAD+, serotonin, and melatonin. The key reasons these matters are tied to the following two phenomena: (1) severe calorie restriction led to an increase in the Trp → Nam which can augment NAD+ in aging and in disease generation to extend survival; (2) the conversion of Trp → Nam is also increased by a vitamin B1 deficiency. This begs the question………..does B1 deficiency confer a survival advantage by creating a pseudohypoxic state in mitochondria that are badly damaged? The answers in this new blog and new series might surprise some of you.
Did you know the production of Nam from Trp is important for maintaining cellular NAD+ concentration? For example, half of the niacin supply is accounted for by Trp intake. Tryptophan is an essential aromatic amino acid. Many environmental effects of light affect various factors on the conversion percentage of Trp → Nam and most people seem oblivious to this fact. It has been well researched and reported that vitamin B1 deficiency increased the conversion percentage of Trp → Nam. Now ask yourself what this implies and what the collateral effects of this might be in a world built around alien lights? https://www.patreon.com/posts/32419906
I would have thought that it was an energy backup as an emergency.