This is a bit of a long story because I can’t tell if I have a genetic problem that only shows up under stress or just plain deficits due to extreme stress. I am a 58 year old woman having some pretty severe health problems that I have recently begun to think might be due to thiamine deficiency, malnutrition and/or possibly some sort of genetic problem.
Medical History
I was hospitalized with pneumonia three times before I was 5 years old, once again in isolation ward at age 7. I also had several childhood illnesses including Rubella, chicken pox, and mumps. At age 5, I was diagnosed with exercise induced asthma and prescribed Quibron. Once I hit puberty, my respiratory problems seemed to resolve themselves as long as I avoided aerobic exercise.
At age 9, I was diagnosed with progressive sensorineural hearing loss (an indicator of mitochondrial disease that I only recently learned about). I had a curved loss with 60% gone in the higher frequencies down to about 40% loss in the low ones. My mother was also diagnosed with hearing loss that had gone unrecognized. My daughter also has a mild hearing loss that was diagnosed as an adult.
Major Life Stressors and Emerging Problems with Nutrient Absorption
From 2000 to 2012, had several major life stressors including the death of my second husband to colon cancer, a dog snapped at me and severed my lower lip, my third husband lost his job and attempted suicide, early retirement, bankruptcy, foreclosure on my home and then moving to a new state. I was diagnosed with post-traumatic stress disorder (PTSD) and received weekly trauma therapy for a year.
During the aftermath of the PTSD trigger event, I began having problems with nutrition. I would eat a meal and get no energy from it. After taking an early retirement from my job and losing my house to foreclosure, we packed up and moved out of state.
I never recovered from the exhaustion and stress of the move. We were nearly homeless one night after our car broke down and I had no more money because we had just paid the deposit to rent a house. I managed to leave all our keys in the car at the repair shop. My first husband wired us money for a hotel for the night.
The problems with digestion continued and my health seemed to go downhill. I was tired all the time and my brain was not functioning well. I tried going for walks but would come home exhausted. To make matters worse, we were scraping by on one third of the income I had before I retired and I had no health insurance. I didn’t know how to go about finding help in those conditions. I’ve always been in the system.
More Digestive Problems
In 2013, my digestive problems got much worse and I had diarrhea almost continuously for three weeks before finally going to the local university emergency room where I was surprised to find my blood pressure was 230/140. I think they had to give me at least two potassium drips. After they initially got my blood pressure down, an intern came in to give me some sort of eye exam. He started lecturing me on using the ER for primary care. He then proceeded to interrupt me when I tried to tell him about zonking out (see below). My blood pressure went up 100 pts before he was finished. That experience just increased my reluctance to go to physicians when I am sick.
I was admitted for four days and my major systems checked and seemed fine. They gave me scripts for Lisinopril and Coreg and referred me to a local clinic.
The NP I saw at the clinic put me on 1000 mg Metformin ER. She referred me to a GI who diagnosed me with GERD, Pancreatic Exocrine Insufficiency of unknown cause and prescribed Omeprazole and Creon.
The diarrhea died down but I continued to have steatorrhea and my energy did not improve. I had a constellation of general vague symptoms as well as unusual ones. I also continued to have problems eating. The recommendations for GERD are to eat small meals a day. I found that five small meals of no more than about one cup of food a day were all I could tolerate. I also stopped eating vegetables or high fiber foods. Even following those rules there were many days when I had nausea and could not eat very much.
My type 2 diabetes has not been that bad, but my day to day glucose readings were very variable. My A1C was 6.5 2013, 5.8 in 2015, 6.8 in 2016, 7.0 in 2017, and 7.4 in 2018. As I try to get health care professionals to address my problems I keep running into diabetes. As if my diabetes where the cause of everything I could ever experience. I recently ordered a fasting C-peptide test which showed I was in the high normal range. Glipizide did me no favors as it likely increased my insulin resistance.
I know what is normal for my body and what is not and what I have been experiencing is NOT NORMAL!!
Catatonia-like Episodes upon Eating
Starting in 2013, I started having episodes that I call zonking. I would eat something and almost immediately get very sleepy and usually would just fall into a sort of zombie-sleep-like state for 10-30 minutes. Sometimes it seemed sort of catatonic and others is was more like a strong urge to sleep. It wasn’t normal sleep in that there was no dreaming. Sometimes I was in a kind of frozen pose instead of laying my head sideways or getting comfortable. At first it seemed like they were correlated with high-availability carbs, but over time they became an almost daily occurrence with any type of food I ate. These episodes would sometimes disappear for a few weeks and then reoccur. There was no pattern I could discern nor tie to hormonal cycles.
I have been keeping daily logs from 2013-2016. I reported the zonking episodes to my NP and she prescribed Lactulose which just made the diarrhea worse. She ordered an ultrasound on my gallbladder and liver and no major problems were found.
The zonking episodes were really disabling. I would be feeling fine until I ate something and within a 1/2 hour I would zonk out and feel very groggy afterwards. It didn’t feel safe to drive so my husband had to take me shopping or do the shopping himself when I was too tired. I didn’t drive from 2013 to 2016. At times, I didn’t want to eat at all so I could keep myself functional long enough to do something. I found out the limits of fasting pretty quickly.
Left Temple Headaches, Migraines with Visual Aura, and Cognitive Deficits
I also had left temple headaches starting in 2013 and a few migraines also involving left temple pain but mostly just visual aura. I never had migraines previously. After I fell going up the concrete steps to our front door, I became very cautious about moving when I was in one of these states. I noticed that I became very clumsy with tasks that you normally don’t think about like opening a can or a pill bottle.
I also noticed a significant decline in my ability to comprehend speech when I was in one of these states. This was first mentioned in my logs in 2013. I have always had a problem due to my hearing loss but there seemed to be a magic something taking place in my brain that took care of turning sounds into words. Somehow that process was failing when I was in the dizzy and ditzy state.
My condition was deteriorating in 2016 and I was experiencing more severe brain problems that are what I now call dizzy and ditzy. Dizzy and ditzy feels like being very drunk. I was spending more and more time in bed which was making my diabetes worse. When my brain was functional I was researching and trying to figure out what might be causing my condition.
In August 2016, I came across a description of gluten ataxia. The symptoms seemed similar to what I was experiencing so I tried eating a gluten free diet for a few weeks and started feeling better. After two weeks, I decided I was imagining the improvement and tried eating something with gluten in it. After about two hours I began to experience the dizzy state and the left temple headache. From that time I have remained gluten free.
It was my intent to get tested for Celiac at my next appointment, but my husband was hospitalized in October 2016 for sepsis due to undiagnosed type-1 diabetes. This was the worst kind of trauma for me because my second husband died of colon cancer. Knowing that, I applied the techniques I learned during trauma therapy to keep my stress level down. As a result I was able to return to the hospital for his follow-up visits with no increase in blood pressure or other signs of HPA activation. I think it helped me overcome my doctor phobia and I have been increasingly more able to deal with medical situations. My health and energy levels were also improving due to the gluten free diet. I tried various diets and found that I had the best energy levels on a gluten free vegan diet.
Since I did not get in to see my primary until six months had passed gluten free my celiac tests were inconclusive. I found a really good allergist and in January 2017 was diagnosed with 44 food allergies including wheat, barley, oats, eggs, milk, and assorted nuts, fruits, and vegetables and yeast which is everywhere. Six months later, I was diagnosed with multiple environmental allergies. My condition began improving dramatically as I stopped eating the foods that I was allergic to. However I found that I was still unable to eat solid food and get energy from it. Meanwhile my NP added 10 mg glipizide which caused hypoglycemia when I was feeling well and active.
I didn’t experience any more dizzy and ditzy episodes from October 2016 through March 2018.
Diet and Malnutrition
I did have, and still have, episodes where I become very sleepy and nauseous after eating something. This leads to a feeling of being ill and not enough energy for normal activity. My condition improves if I semi-fast for the remainder of the day and then reduce my intake of protein and fat for a few days. As a result, I became more depleted nutritionally as time went by.
I don’t think I’ve managed to convey to anyone just how my diet has shifted from normal and especially what they seem to expect of diabetics. Many days I was unable to even manage 50 mg of protein and if I didn’t eat enough carbohydrates I had difficulty sleeping. I was on homemade liquid meals from 2017-2018 and only recently was able to transition onto whole foods after stopping Metformin.
I still struggle to explain why I suspect nutritional deficits in the face of a body that is down 10lbs but still 220. I think my body compensates by doing things like lowering my body temperature. It was 96-97 on a regular basis over the past 6 years, yet my thyroid panels are normal except for high TSH which may be due to my Biotin supplementation. In May 2018, I had more thyroid testing done.
- TSH: 7.5
- fT3: 3.1
- fT4: 1.34
- rT3: 22.2
- TPO: 12
- Antibody <1.
Sometimes my body heats up immediately after eating. I’ve also had iron deficiency anemia where my hands and feet got painfully cold. Sometimes I get chilled and find my body temperature is 95.8 – even in July.
Other Weird Symptoms
Visual Disturbances
I haven’t been able to match up these phenomenon with technical names so I am just describing them as best I can. There is some overlap as I am not sure what is part of which phenomenon.
- Problem: After-images occurring too easily
- Duration: 3-4 years
- Frequency: Intermittently – seems to be worse when I am having diarrhea episodes
- Details: Can’t find exactly what these are called. In normal vision if you stare at something for a long time then look at a blank surface you can see a phantom image of inverted colors. What has been happening intermittently with me is that I will see these images instantly and they take longer to fade than normal. This is especially bad in the mornings. I made up a test for myself to track how bad my vision was on any day by looking at the GOOGLE logo. On bad days it bounces around in afterglow very strongly; other days not at all or not as strong. Sometimes if we are out on a sunny day a glance at a bright reflection off metal will create a strong after image that persist for 20-30 seconds or more. I have to be very careful not to let my eyes linger on anything shiny.
Along with the above problem I also experience a kind of sparkle sometimes where if I look out the window, even on a gray day and then back inside there is a brief field of sparkle in my vision.
- Problem: Seeing my pulse in my eyes
- Duration: 6 years
- Frequency: Not as much these days, but was especially bad when my blood pressure was uncontrolled.
- Details: I would see a grayed pattern around the lower outer edge of my vision that would flash in intensity seemingly in conjunction with my heart rate.
Finally, my left eye seems to flutter and roll.
- Problem: Left eye flutter and involuntary eye roll and moving illusions in vertical images.
- Duration: 9 months in 2015, confirmed by eye doctor.
- Frequency: Started very infrequently but has progressed to almost daily.
- Details: Irritating flutterly feeling in my left eye. When I looked in the mirror I noticed the left eye was rolling left or attempting to roll left involuntarily. This may be related to another problem I have been having for several years where my vision wobbles. It comes and goes in severity, but if I look at any image that has strong vertical contrast it appears so move. For example a picture of a coliseum or tiger will appear to be moving like the way optical illusions move. The moving illusion also occurs more frequently when I am having bouts of diarrhea.
Migraines With Aura
- Problem: Migraines with Aura
- Duration: 2 years
- Frequency: 3-4 times a year – sometimes in clusters
- Details: I get migraines where I see an aura. It starts with a blind spot in the center of my vision, in less severe ones it is more of a sparkle overlay and not as blind. The circle then becomes a semi-circle of the outer edge of each eye that becomes bigger until it moves out of the eye. Then pain comes or not. I can sometimes reduce severity by immediately going into a dark room and lying down. Sometimes I get the headache and sometimes just the visual aura. I mention these here because I have wondered if some of my visual problems are migraine auras that haven’t fully developed.
Allergy Shots and More Symptoms: Ophthalmoplegia, Dizziness, Speech Impairment
In January 2018, I started desensitization shot therapy with my allergist. In February 2018, I had another episode of dizzy and ditzy that was complicated by additional symptoms of hypoglycemia. After consulting with my allergist, he set my shots back a few weeks and set up a standing lab order to see if he could tease out the problem. In March, I had the worst episode of dizzy and ditzy I have experienced to date. It included ophthalmoplegia, dizzy, very sleepy, altered consciousness, and personality changes. I was walking with a sort of limp as if my left leg were injured. I laid down on a bench outside the allergist office until the sleepiness passed. When the people at the allergy clinic got back from lunch they checked my blood pressure which was normal and did a blood draw for labs.
I also had the worst episode of speech impairment ever. I remember thinking it was funny because it sounded like they were speaking so much gobbledy gook. I used mindfulness to notice and try to quantify what it was like. I noticed that my intellect was intact, which distinguishes the condition from brain fog where it’s hard to think at all. But things like trying to speak or find words was hard and I got confused easily. Oddly, I had no problems reading and comprehending research papers and I could write, except I made more typing errors. I had a quarter sized mark on one of my arms from the previous day’s shots, but my allergist did not consider my brain symptoms to be due to the allergies. My movements and general condition was very much like being very, very drunk.
Up until that point I had associated dizzy and ditzy with gluten exposure. Once I was sure there was no gluten in the shots, I was a lot more worried about my condition. I regretted not going to the ER since that might have helped me get a diagnosis. As it was, the allergy doctor only checked my tryptase levels and blood sugar which was 119. That level of blood sugar is hypoglycemia for me. I start getting symptoms under 130. This second episode was much harder to recover from than the first and I had lingering symptoms for months afterwards.
Medication Reactions
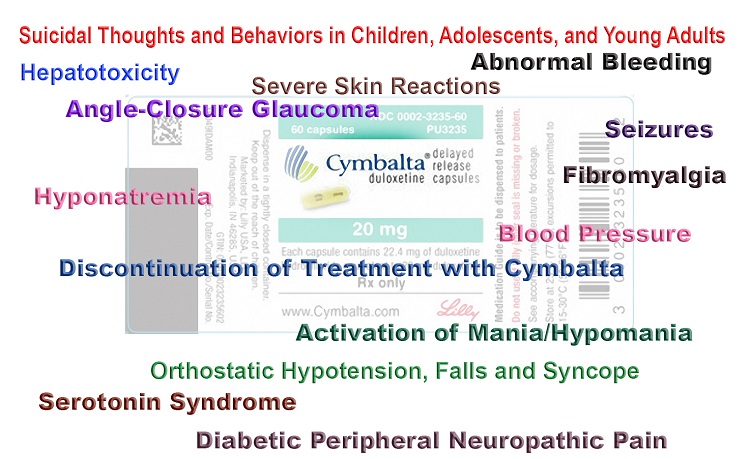
The glipizide combined with 1000 mg Metformin ER for the type 2 diabetes was causing me severe problems, even as my energy levels and inflammation was improving. The repeated episodes where I had to lower my protein and fat intake was really difficult with the medications I was on.
One day I had a different sort of drunk feeling with sweating and distorted vision while out shopping. It got better when I ate something. I got home in one piece and spent the entire afternoon eating every hour until things improved. That was the last time I took glipizide. I started looking for a new primary who understood nutrition.
I found a new primary two hours away who seemed like a good fit but this story is already too long to describe what went wrong. Sometimes a bad thing has to happen before good ones. I found myself without a primary and experiencing more dizzy and ditzy symptoms. The problems started at the request of my new primary PA, I changed my metformin dose from 2 500 mg tablets in the evening to 500 mg morning and 500 mg evening. After a few days I woke up with a 206 fasting glucose. So I doubled down and started taking 1000 mg 2 times a day. That made modest improvement of fasting glucose but also caused steatorrhea and diarrhea to return.
Thiamine Pyrophosphate Order Delayed
I began taking 13 mgs of thiamine pyrophostate (TPP) in 2014. Recently, I ran out of the TPP sublingual I normally take due to a shipping delay, so I switched to oral 500 mg Thiamine HCL capsule. Over the next two days, I had cramps in my calves, congestion and coughing after my normal light exercise and a body temp of 95.8 in the evening. Then another episode of dizzy and ditzy with mild ophthalmoplegia and dehydration. I was drinking salt water and still couldn’t retain water. I always drink my water with electrolytes and I went through a whole gallon in a day. My blood glucose was 289 in the evening.
I’ve been having problems with burning feet and neuropathy since March 2018, it comes and goes and makes it hard to get to sleep. I first reported mild symptoms of neuropathy in my logs in 2013. TPP and B2 and sometimes calcium supplements help.
Once TPP arrived I started taking it 3 at a time (3x13mg) as well as extra magnesium glycinate and other B vitamins, but my symptoms weren’t improving as much as I expected so I started looking for other causes.
While researching various genes, I came across a paper on thiamine transporters and metformin. I have at least one mutation in one of those transporters but it doesn’t have any established meaning that I can find. I had not considered thiamine deficiency as a possible cause for dizzy and ditzy even though the symptoms seemed similar because I was taking 13 mg of TPP sublingual daily.
I started easing off metformin and my energy and burning feet symptoms improved. A side effect was the metabolism issues that had kept me on a liquid diet improved and I can eat and metabolize solid food again.
Going off metformin caused a slight rise in my fasting glucose so I had a lab test run myself that shows I still have normal insulin production. My glucose response varies quite a bit but I sometimes get good response when I do daily treadmill with glucose in the 110 range two hours after a meal
One night I had a lot of congestion and couldn’t sleep so I took a dose of 3x TPP and the congestion went away and I was able to sleep. I have had ongoing issues with lung congestion since 2010. I think this may be a return of the lung problems I had as a child. I believe my body compensated with hormones and is now decompensating due to menopause. The fact that the congestion got better after thiamine intake is worrying. But I have a strong placebo response so I have to be careful about creating correlations. The lungs issue has been observed by both my primary and my allergist. I frequently get very thick mucus that may be due to inadequate fat digestion.
Ran out of Thiamine AGAIN!
I had a dizzy and ditzy episode with temple headache 7/11/2018. I went through three bottles of 60 Sublingual TPP in a few weeks and was unable to order more due to factory back order. I researched other versions of thiamine. Benfotiamine was having no effect that I could detect. Sulbutiamine helped with some of the brain problems like short term memory. I had concerns that I wouldn’t be able to absorb some of the other forms due to my fat malabsorption. Fortunately, I came across the blog where Dr. Lonsdale explained what “fat soluble” really means regarding lipothiamine and allithiamine, so I ordered both of those as well as liquid TPP from the UK.
Neither of those had arrived by July 14, when I took my last TPP. I had a return of symptoms over the next few days. I started using a B-complex that had TPP in it, but even with that I had another dizzy and ditzy episode that lasted several days. During that time, I got sleepy every time I ate a meal. My meals are small to start with because of the GERD: one cup lentils with tofu or a tofu taco with avocado. Both of those meals that were normally well tolerated gave me symptoms of sleepiness and fatigue.
I found a comment somewhere about the need for manganese, so I got manganese glycinate supplements and that helped ease the neuropathy until the Lipothiamine and TPP liquid arrived. The first Lipothiamine was like magic, my eyes cleared up in about 15 minutes. They do that sometimes after I eat. The neuropathy symptoms were down by the time I went to bed in the evening. In the morning, my feet were hypersensitive and I had leg cramps due to low magnesium. I still have to take extra magnesium during the day and at night as well as other B-vitamins. I have some mild brain symptoms too but they may be due to the stress of starting with a new primary.
The big difference is in my energy levels, which are sufficient to make it through the day and no burning feet at bedtime. I still have limited ability to metabolize food, I tried to add 1/2 cup brown rice to my daily lunch and it sent me into borderline dizzy and ditzy. A typical day’s intake for me is 1 slice tofu, 1/2 cup lentils, and tofu taco with avocado, some vegetables, and a big leafy green salad with avocado, beans and nuts. Sometimes I can have a snack of fruit but more than that I start having problems. I suspect I have other deficits that may be slowing my recovery. I am waking up at 1 am and having to eat something to get back to sleep.
I had another episode this past week. I was preparing my allergy records for a trip to ER and was very dizzy and clumsy and a band of pressure in my forehead. I had been taking 2 50 mg enteric tablets 3 times a day of Lipothiamine but was experiencing symptoms of illness after eating and tiredness. I was only rescued from ER by modifying Lipothiamine dose so that it would be absorbed in my stomach instead of my intestines. I’ve had symptoms of intestinal malabsorption which haven’t yet been evaluated by a GI. I have checked several nearby GI practices without finding one who takes a self pay patient.
Genetic Testing
Genetic testing has helped me discover other problems I have involving metabolism. I haven’t cataloged all my mutations but I have a diabetes related set of 3 homozygous SNPs called TCF7L2. The way I understand it is that people with this phenotype have increased signaling mechanisms such that when they have excess fat, the pancreas responds by lowering insulin response to food and the liver increases morning glucose. Losing the weight, reduces the expression and returns things to normal. I have other genetic mutations which may be impacting me such as MTHFR(++), MTRR(++), and a rare BCHE mutation that impacts my choline levels. It also makes me vulnerable to pesticide exposure. I have to take Trimethylglycine (TMG) and various B vitamins to keep homocysteine in check. If I don’t take enough TMG and CDP choline, I get depressed.
I am seeing a new primary who is a doctor of Internal medicine. The new doctor’s choices for medications are spot on for my genetic type, they both work on the GLP-1 pathway, but they also increase insulin response. I don’t see how that doesn’t cause hypoglycemia, since I have normal insulin production. I have more research to do before making a decision on new medications.
While I can see that the deficiency symptoms I have been experiencing may be a result of poor diet and digestion, the fact that Thiamine HCL did not work and my condition improved so much after stopping metformin leads me to believe I may have a genetic condition. I really need to find a university that is researching metabolic and genetic conditions so I can get a diagnosis.
Medications and Supplements
Most of these supplements were added in 2017 after I started homemade liquid meals. Prior to this I was taking a sublingual B-complex & Magnesium glycinate.
Current Medications
- Singular 10 mg x 1
- CoReg 12.5 x 1
- Lisinopril 10 mg x 1
- Cetirizine HCL 10 mg x 1
- Omeprazole DR 40 mg x 1
Most of these were added when I started liquid diet
- B-6 Pyridoxal-5-phosphate sublingual 15mg x 1 (more if homocysteine symptoms)
- B-1 Thiamine pyrophosphate (TPP) sublingual 13 mg x 1 (the one that is backordered)
- *TPP liquid 3 x a day or as needed with malabsorption due to intestinal swelling
- *Lipothiamine tetrahydrofuryl disulfate 100 mg 3 times a day with extra Mg.
- *Liquid CoQ10 100 mg x 3 times a day
- B-2 Flavin mononucleotide sublingual 18 mg x 1
- B-3 27 mg as Inositol Hexanicotinate, 25 mg as NAD sublingual 25 mg x 1
- Liquid B5 + Carnetine
- MethylCobalmin, sublingual 1 mg x 1
- MethlyFolate (S6)-5-MethylTetraHydroFolate glucosamine salt sublingual 800 mcg x1
- Biotin 5000 mcg sublingual 1 x
- Chelated Zinc, zinc glycinate 22 mg x 1
- Selenium as L-Selenomethionine, capsule 200 mcg x 1
- Kelp 325 mcg Iodine, 325 mcg x 1
- TriChromium Chromium Picolinate, Chelavate, & polynicotinate, 500 mcg x 1
- Magnesium Glycinate (capsule at home) ~ 800 mg per capsule 50% Mg x 2
- Liquid chelated Iron biglycinate 10 mg, Yellow dock 10 mg x 1 (not long term)
- D-3 5000 iu with K2 1 sublingual 125 mcg D3+ 90 mcd K2
- Ultra K with K2 softgel, K1-1000 mcg + K2 1400 mcg x 1
- Algae DHA 200 mg x 1
- Phosphatidylcholine softgel 1300 mg x 1
- Source Naturals Vitamin A as palmitate 1 x 10,000 iu
- Buffered C-1000 complex Calcium Ascorbate 1 g x 2
- Southwest Botanicals Mucuna Powder (self capsule) ~ 810 mg x 1
- Citicholine (self capsule) ~820 mg, 1-2 as needed
- Nootropics Sulbutiamine 200 mg (thiamine derivative) 1 capsule, 200 mg x 4
- TrimethylGlycine (Betaine) 1 g x 2 with each meal containing methionine
- *Taurine 1000 mg
- Liquid Calcium, Magnesium, D3, Phosphorus as needed for sleep
*Recent additions
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Share Your Story
If you have a complicated health story to share, send us a note.













I’ve recently found and joined a PEI (Pancreatic Exocrine Insufficiency) support forum. Many of the issues I have are shared by fellow sufferers. My DNA test didn’t give me anything that was diagnostic, but I found 75 mutations in my PRSS1 gene which codes for trypsinogen. PRSS1 is involved in hereditary pancreatitis. My father had acute pancreatitis at age 50 and recently was diagnosed stage 2 pancreatic cancer. I also found a controversial mutation that causes thiamine related Maple Syrup Urine Disease.
I improved my energy levels when I found a patch form of iron, I have long term low grade anemia. The problems with muscle weakness improved with calcium supplements. I still take 300-450 mg allithiamine daily, my energy doesn’t start until I do that and put on the iron patches. I found out omeprazole inhibits carnitine resorption in the kidneys so I have to take carnitine daily or I get elevated ammonia levels and associated symptoms.
My diabetes progresses unchecked. I can inject tons of insulin without effect. Potassium seems to improve the insulin response, but I get a strong pulse of glucose at sundown that spikes me over 300 almost daily. Every time I have to go any length of time without CREON (digestive enzymes), my glucose setpoint rises. Fat and protein digestion are totally dependent upon how much Creon I have. If I eat too much fat or protein I can get diarrhea and that depletes me pretty fast. It costs $650 a month so I have to purchase it overseas and can’t afford to up my dose even if I could get a GI to pay attention to my problems. They mostly don’t know squat about the pancreas.
I hope to someday get into a pancreatic cancer early screening program or get referred to a research clinic so someone can evaluate my genes and pancreas. Meanwhile I’m surviving.
I too had that issue with insulin Susan when I was eating a low carb diet. I struggled to process meat regardless of what I tried. In the end I abandoned it & adopted a whole food plant based diet 3 years ago. It seemed counterintuitive, high sugars & all that, but I persevered, just juicing mostly veg with some fruit for the first month.
To my utter amazement & although my blood sugar was somewhat unstable & higher Initially as my body was clearing out the ectopic fat, by the end of the month my blood sugar had dropped, my insulin sensitivity had returned & I had to radically cut my insulin intake by more than half. I also lost some of the even more VERY stubborn weight I had gained during the 8 years of low carb.
For me, it’s the fats that drive my insulin resistance. The more fat I eat, the more insulin I need. I try now to eat according to the ‘Mastering Diabetes’ protocol as much as I can. Natural, unprocessed plant foods. Even fruit is no longer an issue without fats. I’ve been totally gluten free for 12 years & avoid processed & refined foods like the plague. My body doesn’t detox very well & I suspect my gut lymph is very backed up. I may go back to juicing at some point & do an extended juice fast, but at present I am experimenting with some Ayurvedic herbs/spices that hopefully will help my body detox all the toxins stored in my excess fat, & can help lower blood sugar.
That’s pretty much how my body works as well. In 2007 I became vegetarian and stopped all the junk food, lost 60 lbs and got off of all medications. I used a whole plant food diet. But in 2010 I started having episodes where I would eat a meal and not get any energy from it. That progressed until 2013 when I had bad diarrhea and wound up in hospital with hypertension. Later, I was put on Creon prescription digestive enzymes with a diagnosis of Exocrine Pancreatic Insufficiency (EPI). I can’t eat very much fiber or the enzymes don’t work and I get loose stools. I’m vegan now and also gluten free – mainly due to allergies to eggs, wheat, dairy and a host more. I finally found a patient forum for EPI and many of my problems are common to other patients with that condition. I found calcium supplements help when my leg muscles feel weak. I’m getting my b12 and others from a patch as well as iron. Still taking the B2+allithiamine+magnesium glycinate. I’m having iron deficiency anemia – my ferritin is 7.
I experimented with chinese herbals in 2007 and eventually found that although there is much wisdom, there is also much foolishness. I only take serrapeptase as an herbal now.
I’ve narrowed some of my problems down to branched chain amino intolerance. The initial reaction for breaking them down is very dependant on TPP. When Leucine and isoleucine build up in blood they cause problems in the brain. The brain winds up swapping out aminos needed for neurotransmitter synthesis for Leucine. That is what causes my Wernicke’s like symptoms and dizziness. I’ve had 2 MRI and one CT scan of my brain with nothing to show for the dizziness.
The problem with my TSH being high went away after stopping metformin and taking allithiamine with B2 and magnesium for over a year now.
I think some of my other problems may be due to omeprazole. I found an article that said it blocks carnitine in vitro. Carnitine supplementation is helping with my protein intolerance. Getting off omeprazole is a real problem as it has kick back effects and my food allergies elevate my gastric acid.
The allergies may be due to carboxypeptidase N deficiency, I have a genetic variant for that but no way to test it at the moment.
Metformin blocks b12 and folate. I see you have 1 mg methylb12 and 800 mcg methylfolate listed, but you might try increasing the b12 and then the folate. Also it’s worth noting that injections are far superior when it comes to B12 — that might just take care of your neuropathy.
Also, for what it’s worth. The doctor who created the b12-oils says that molybdenum, selenium and iodine are needed for B2 to work, so if you’re deficient in those you might see if adding those helps.
I agree with Kelly, B12 is vital. Both Thiamine & B12 are crucial for nerve support & repair in different ways. B12 deficiency can affect cognition, too & a host of other things, triggering anything from depression, anxiety, panic, cognitive impairments, dementias, even psychosis if the deficiency is very bad. Ocular issues, ataxias, etc, too. https://www.b12deficiency.info/signs-and-symptoms/
Many things can impact on our ability to either absorb or utilise B12 including Metformin & other drugs, gastric surgery, weak stomach acid, a lack of Intrinsic factor, an inability to methylate or metabolise it, & declining ability to absorb/utilise it as we age, etc. Having ‘normal’ levels does not preclude deficiency as everyone’s tipping point into deficiency varies. High blood levels may actually mean it is not being utilised but is just floating aimlessly around the bloodstream.
I reversed my Peripheral Neuropathy, raging restless legs, acid reflux, hiatus hernia, palpitations, high blood pressure and rampant Candida & fungal issues 12 years ago by dumping wheat/gluten, refined sugar (another nutrient-robbing ‘empty calorie’ pseudo-food), & most dairy apart from a little butter or ghee & addressing the rampant nutrient deficiencies it had left me with, with a host of supplements, especially magnesium & those beautiful B vitamins.
Whilst you may have dumped the wheat, if you are still consuming sugar &/or dairy that could explain the wipe-out after eating. The modern diet burns through B vitamins something awful. I recall even in my 20’s (I’m now in my mid 60’s) feeling so wiped out after eating – especially sweets/candies – it was as much as I could do not to lay down in the street!
Some of my symptoms very much mirror yours. Just one addendum. I do find that increasing Thiamine means I need to increase B12 & make sure I am getting enough Folate, .biotin & B2. I don’t absorb oral B12 very well. Sublingual drops work better for me. The B12 you are ( or were) taking may not be being absorbed or utilised very well, & that could make a big difference. Have a look at the B12deficiency.info site. Lots of very interesting info on .b12 on there.
Susan, did you try increasing your B12? I find sublingual ‘active’ B12 drops work much better for me than any tablets. I take 10 drops every few days. Taking Thiamine also seems to increase the body’s need for B12, well it does for me.
Supplementing selenium without iodine made what I think was a pre-existing iodine deficiency even worse. I absolutely cannot take one without the other for any length of time, which isn’t surprising since they work together in the production of thyroid hormones.
Susan, I wonder if you have considered a low oxalate diet? I had a host of unexplainable health problems and I discovered my gut was no longer breaking down oxalic acid in my food (due to dysbiosis from overuse of antibiotics), which caused oxalate crystals to build up in various organs, bones, etc. One of my number 1 signs of eating something too high oxalate is zombie sleepiness after eating (the same kind you’ve described). Your diet is very high in oxalate, from what I read. Oxalate build up in the body can cause so many symptoms that seem unrelated. You might check out the private Facebook group “Trying Low Oxalates” run by researcher Susan Owens. Good luck to you
I agree! Susan, Oxalate toxicity is a possible cause of many of your issues. The fact that you are taking 1000mg per day of vitamin C will cause the body to covert the high dose of C into oxalate! In addition to the Trying Low Oxalate Group on Yahoo, as Amy suggested, please go to the Sally K. Norton website. She has some great information and free downloads for people who want to start on a low oxalate diet.
I would also talk to your doctor about getting off of Lisinopril and trying a different blood pressure medication. I also took Lisinopril for a while and it gave me visual migraines or migraine with weird “ sparkly” visual aura. Once I stopped the Lisinopril, the visual migraines stopped.
I am reading this because I am looking for answers to my husband’s cramps. They are caused by the antibiotic Levaquin but there is no known cure for being “floxed”–taking quinolone antibiotics. He has lots of allergies with mucus and going into bronchitis. He has had candida to some degree for the last 40 years but we were keeping it under control. We found that when we started taking Bone Broth it evidently helped his leaky gut. With the first cup, he said it felt like his brain woke up and he has been able to think clearly. He was already taking lots of vitamins and other types of supplements but evidently was not absorbing them due to the leaky gut. I also have had relief from my digestive issues after taking Bone Broth. I am going to check into the thiamine to help with his leg cramps. Just maybe this is the missing link. Thank you for this post.
Try magnesium glycinate for leg cramps as well. If you take thiamine you need extra magnesium. I have absorption issues so lots of problems getting vitamins. I have used sublingual or liquid to bypass that problem. The thiamine may be most helpful with the digestive issues. Glad you found something useful.
Have you ever looked into inducing autophagy, the recycling of aged or dysfunctional cellular parts? You can do this with a fasting mimicking diet or spermidine. I wonder if this would help the quinolone toxicity people by helping stimulate the generation of new mitochondria.
Hello, I have neuropathy from head to toe. I was found to have lots of lactic acid in my body. So I got tested for thiamine deficiency. It came back lower than normal. So I thought problem solved. Its been over a month and I’ve supplemented with thiamine, even got my levels rechecked, they were high this time. No improvement, probably feel worse a month later. Is there any chance my body is just not responding to the thiamine yet? Is there a way to find out if I’m doing this wrong? Any advice if I’m not being patient enough?
You may need a different form of thiamine like benfotiamine or allithiamine. You also need magnesium, and other B vitamins deficiencies can cause problems they all work together.
If you are taking metformin or other drugs they can interfere with it. (don’t stop the medication, you’ll get your doctor pissed at me)
The solution is to try the benfotiamine with b-complex, magnesium glycinate (or other chelated magnesium) and see if that helps. There are numerous writeups on this site by Dr Lonsdale and Marrs Chandler that talk about what can happen when you try to get your thiamine levels back up.
https://www.hormonesmatter.com/navigating-thiamine-supplements/
was really helpful to me talking about the various forms of thiamine. Benfotiamine has been written about extensively in medical literature in terms of helping neuropathy. I have fat malabsorption so it didn’t work for me. But if benfotiamine doesn’t work then try allithiamine. Also look at other b vitamins like B2 helped get rid of the burning feet problem I was having. And the allithiamine stopped the neuropathy as well. My feet feel too sensitive right now.
Read the articles about refeeding to see what other nutrients may become depleted while you are restoring thiamine.
Hope this helps you, this site has been a tremendous resource for me.
Did your doctors check to see if you have some sort of disease process going on in your body producing the extra lactate? There may be some problem that needs attention.
They did check me for a different reason for my lactic acidity and they couldn’t find any other disease process. My liver and kidney functions were all normal. It’s a month later and have been supplementing with allithiamine and my neuropathy is still getting worse. I’m at a loss for words at how bad this is. I don’t know what to do. I have been also taking magnesium. No help.
I know this is a few years old but Dr Lonsdale mentions that supplementing with thiamine can unmask other nutrient deficiencies. You may want to look at B12 for your neuropathy. Intramuscular injection of B12 is the best way to determine if you are deficient (blood tests just aren’t reliable) – if your neuropathy improves after several injections then you know B12 is the issue.
I’m 99.9% sure thiamine deficiency is causing a lot of my problems including dizzy & ditzy.
I’ve been taking (100 mg TTFD + 800 mg Magnesium Glycinate = 400 mg Magnesium) three times a day for several weeks now. I’m also having to supplement almost all the minerals and B-vitamins.
I had a glitch that resulted in almost no absorption of the Lipothiamine (enteric coated) for about 4 days. I was getting ready to go to the ER because dizzy and ditzy came back. On a hunch, I crushed up two tablets and put them in a normal capsule. I took it and the symptoms were gone in 1/2 hour so I did not go to the ER.
Someone wrote a helpful post on the facebook page that said allithiamine had absolutely no garlic in it. (i’m allergic to thiamine) So I ordered allithiamine and have been taking that. I may have undiagnosed damage to my small intestines. I seem to have intermittent malabsorption of some things. I get a lot of swelling in my small intestines when I have an allergic reaction.
So now I am ravenously hungry, I can’t seem to eat enough food to last me very long My carb tolerance has increased greatly and I can eat things like brown rice with quinoa and buckwheat groats without having any problems. I also seem to be able to eat more foods with methionine in them.
So I feel like I’m on the mend. My new doctor has ordered an MRI, depending on what that shows, I think I need a mitochondrial panel done. It may not be mitochondrial, because I have so many genes that impact my metabolism, but the hearing impairment is definitely genetic and it would be good to know if it is a mutation that affects other organ systems.
Two major clues. 1. weight 220. 2. Diabetes. This is metabolic syndrome due to mitochondrial energy deficiency. Diabetes = thiamine deficiency. What is the intake of sugar?
I have 1 teas sugar in my morning coffee usually have 2 cups. There is 1 g in my soy creamer. Also 3 g in my salad dressing but I probably use several T of that. First thing in the morning I eat a slightly green banana or else my blood glucose goes up if I don’t eat anything. Next I eat lentils + tofu for breakfast, usually got to gym for 30 min treadmill, come back and glucose is 119-130. I eat a kiwi, peach, or mango while I make lunch Tofu taco and various vegs like squash or green beans, snack is popcorn or pistachios. Dinner is big leafy salad w dried cranberries, dried blueberries, cashews, flax seed, garbanzos or tofu.
My glucose control is relatively good when I am up and active but I sometimes lose days to extreme tiredness and that makes me more insulin resistant. When I was 190 my diabetes was in remission and I was taken off all meds. Stress caused a regain. I was 240 when I was hospitalized with an A1C of 6.5 so I’m down 20 lbs but my A1C is going up.
I have 44 food allergies that includes wheat, barley, oats, dairy, eggs, yeast, tomatoes garlic assort fruits and vegs. I cannot eat meat, it causes inflammation and I have an APOE E4 as well as MTHFR (++) & MTRR(++). So I am very carefully measuring out how much methionine I eat each meal. Basically I have problems metabolizing all 3, fat, protein, & carbohydrates. It’s just a matter of choosing which one does the least damage. I have fasted intermittantly trying to deal with things and my fasting glucose just gets worse when I do that.
I just got my fasting lactose measured and it was 1.1. I suspect I have a mitochondrial problem because my mother and my daughter are both hearing impaired and I have been since childhood. My daughter had unexplained epileptic fits when she was a teenager.
My condition improved after stopping metformin and starting TTFD although I had some problems with absorption due to accidentally doubling my omeprazole dose. I’m taking 100 mg Allithiamine 3 x a day with magnesium glycinate and occasionally dicalcium phosphate. My homocysteine was 8 one 6 g of Betaine + P5P.
I forgot my avocado, 1 a day for potassium and fat.
I have found some mutations in thiamine transporter genes but it is very difficult to tease out the mechanisms involved.
One of them is rs6656822 in SLC19A2, my results were TT. I found this in literature but can’t access the full paper.
“Genotype/phenotype analysis revealed that TKT activity was lowest in carriers of SCL19A2 rs6656822 genotype TT (P = 0.008), however eythrocyte TDP did not differ.”
I would be a really good guinea pig for a genetics dept, I’ve got a lot of weirdness. Estrogen would really simplify my life a bit since all of these things seem to have unwound during menopause but the clotting risk is high.
Also I noticed that I have had high RDW values since 2013. It was 15.7 last lab but before that I had one that was 17.3.
Candida is not a real illness. However I do have a genuine Yeast Allergy (IgE pinprick tested). Yeast allergies have been implicated in conditions like Crohn’s disease.
https://www.healthline.com/health/allergies/yeast
I couldn’t recall what brain part it is, but thyroid is not the only thing that is involved in body temperature.
Hypothalamus – This is a region of your forebrain that connects the autonomic nervous system and the endocrine system with the pituitary gland. Your hypothalamus is important in maintaining bodily homeostasis – through regulating sleep, emotions, body temperature, hunger, thirst, and more.
What explains your very high A1c levels?
Why are you not even mentioning hypothyroidism?
Leaky gut occurs over time due to many causes, pill taking is just one if them. Just because you weren’t taking pills at the time you had diarrhea does not mean you don’t have leaky gut!
An all liquid diet of pea protein, rice milk and canola oil would definitely cause digestive issues. Reflux does not necessarily mean high acid.
What about gut fermentation aka auto brewery syndrome causing your bouts of feeling drunk? Why no mention of candida? I don’t want answers. These are rhetorical questions. I wish you well.
The system is eating my comments – shouldn’t have tried to respond from my laptop.
I believe my high A1c is due to glipizide + metformin causing hypoglycemia and hyperinsulemia. I have high normal fasting insulin levels but possibly impaired conversion of proinsulin to insulin due to a genetic mutation. No one bothered checking insulin production before putting me on glipizide. Glipizide works by causing my pancreas to put out more insulin in the morning. So in addition to my high normal insulin there was added more insulin. When I had no energy prior to starting the liquid diet, I didn’t have much problem with glipizide. Once I started the liquid diet and eliminated all the foods that were provoking inflammation I started having more energy and doing things like walking to the library. I thought the sweating episodes I was having was hot flashes but now I think it was hypoglycemia. Also when you have hypoglycemia the body thinks it is an emergency and activates the HPA which increases cortisol and therefore makes me more insulin resistant. (My HPA is overactive due to the PTSD and a lifetime of high stress, I do what I can to keep it calm.)
One morning when I had a particularly high fasting glucose I went for a walk to try to get it down. When I got home my glucose was 15 pts higher than when I left the house. So now I eat something first thing in the morning to tell my liver it’s day shift and it can stop with the glucose already.
All of my thyroid numbers are in the normal range and have always been in the normal range. I have been taking selenium and Kelp. There is nothing to indicate that there is any problem there. The high TSH may be due to biotin supplementation.
My liquid diet started after the allergy diagnosis because I was not getting much energy from my food which has been a problem since 2010. It did not cause my digestive problems. I believe thiamine deficiency and metformin caused the lack of energy from food.
I have a yeast allergy and antibodies to yeast in my body. I eat NO foods containing yeast of any kind as well as no fermented foods and no foods with yeast coatings like grapes or blueberries. I have been very careful in my diet to avoid gluten and all of my allergens but some are almost impossible like pepper or onion. So how do I get candida in that situation? I have a strong immune system and have only been on antibiotics 1 time in the past 10 years and have no colds or flu in that time.
Alcohol of any kind gives me diarrhea. I last had a drink New Years 2000. I do not now have diarrhea in response to the dizzy & ditzy episodes. That one just seems unlikely to me. What exactly would it be fermenting?
I can only go by the evidence which I have that is a GI did an endoscope and measured my ph and it was 2.0. I was very sure it would be non-existant. In addition to that taking omeprazole and creon stopped the chronic diarrhea although I continued to have steatorrhea off and on until I stopped gluten and the allergy foods. Any time I have run out of omeprazole and missed even 1/2 a dose it takes me 4 days to get the diarrhea to stop. If I accidentally eat something with an allergen or have a large environmental allergy exposure, I get very excess acid that is resolved by taking liquid bicarb. Histamine known to cause excess acid as is stress which I had a lot of.
I have been taking my B and many other vitamins in liquid or sublingual forms so there is not a problem.
The website you reference is not valid and the gentleman in question had his license revoked.
Some things stand out quite clearly:
1) clearly hypothyroid … tsh of 7.5 and many symptoms, cold hands, tiredness, low body Temps, overweight, etc. Natural desiccated thyroid can help, as well as taking selenium and iodine to support the thyroid and conversion of t4 to t3.
2) very likely has candida overgrowth, which can cause severe tiredness after eating and overall fatigue. Very common after several rounds of antibiotics… likely began in childhood with multiple bouts of pneumonia and antibiotics
3) maybe has auto-brewery syndrome which actually is self fermentation in the gut causing high levels of alcohol. Often the result of candida or other yeast overgrowth.(https://gundrymd.com/auto-brewery-syndrome/)
4) very likely does not have GERD but rather low stomach acid, which results in malabsorption of B vitamins and other vitamins and nutrients, and causes other digestive issues. Likely has leaky gut from so many medications, causing the food “allergies” which can be reversed by healing the gut lining and raising stomach acid.
5) with such consistently high A1c readings, it appears she consumes lots of refined carbs, sugary foods etc. Altho auto-brewery syndrome may cause this not sure. Recommend following Paleo way of eating… lots of fresh colorful veggies, moderate grass-fed protein, lots of good fats like butter, coconut oil ghee
6) focus on STRESS REDUCTION by not focusing so much on minutiae, but taking a more global, holistic approach. Recommend EFT techniques for calming the limbic system and reducing stress.
7) Addressing the hypothyroidism and candida overgrowth and low stomach acid will go a long way to healing her main symptoms. Follow the work of Roby Mitchell MD (www.drfitinfo.com) for more info on these approaches.
My theory: Hypoglycemia based in disturbances of the citrate cycle and the Pyruvat- Dehydrogenase. In this case Pyruvat is transferred into Lactate and this results to a lactacidoses.
Typical symptom is sudden tiredness after meals high in carbs or after musslework. Those patients often develope Sympathicus over reactions as protective mechanism against low bloodsugar. Often they wake up in the second half of the night due to a lack of ATP (mitochondrial energy ) with sweating, heart palpations, trembling or panic attacks.
Recommendation: no sugar , law carb diet and mitochondrial support.
In acute ‚ sleeping attacks/Zonks/Fressnarkosen‘ press the juice of 2 lemons into 1l water and drink it continuously over the day. This helps to avoid the citrate cycle blockage.
(Sorry for mistakes in the scientific terminology ! I usually operate with these terms in German , not in English.
That makes some sense given that I get hypoglycemic symptoms like sweating, blurry vision, altered brain if my blood glucose goes too below a certain point that is not what the medical community calls hypoglycemia.
I’m doing the best I can with diet – low carb vegan anyone? I have problems with meat due to the methionine and tyrosine content as well as having APOE E4 and other Alzheimers genes which means I need to keep my fat content down.
I can’t do the lemon thing because I’m allergic to all citrus. Maybe I can capsule citric acid and try that.
Your English makes sense to me fine, my dad lived in Germany most of his adult life and I learned a little of the language during visits. Thank you.
My electrolyte mix that I put in my water has citric acid in it. I can add a bit more to see if that helps. I’m eating as little carb as I can get by with and still get to sleep at night and not overload the protein pathways nor the oil ones. I feel like I’m between 3 rocks and a hard place sometimes.
Hello, I have neuropathy from head to toe. I was found to have lots of lactic acid in my body. So I got tested for thiamine deficiency. It came back lower than normal. So I thought problem sovled. Its been over a month and ive supplemented with thiamine, even got my levels rechecked, they were high this time. No improvement, probably feel worse a month later. Is there any chance my body is just not responding to the thiamine yet? Is there a way to find out if I’m doing this wrong? Any advice if I’m not being patient enough?