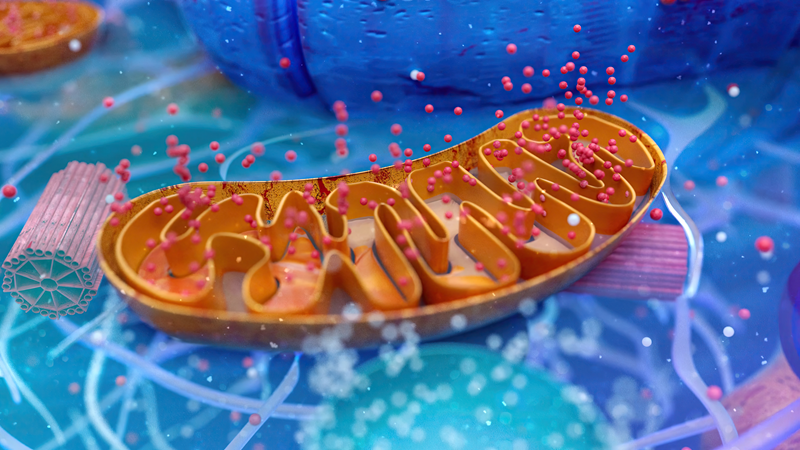
Mid December, I gave a talk on mitochondrial capacity and thiamine’s role therein (included below). My argument was that mitochondrial capacity e.g. their capacity to produce ATP efficiently from the foods we consume, and to meet the demands of living, drives health or illness. I also argued that thiamine drives mitochondrial capacity, and thus, is implicated in modern illness.
It is an argument I have made for years now, and of course, I wrote a book about it, together with the late Dr. Derrick Lonsdale. It is not something readily considered by western medicine, however. Even as our understanding of the molecular mechanisms and pathways connected to mitochondrial functioning has expanded over the last century, the fundamental nature of mitochondrial energetics remains underappreciated. We look to everything else the mitochondria do as somehow more important to health and disease than simple energetic capacity, forgetting that these other processes do not happen without sufficient energy.
Energy is the most basic unit of life. It is the capacity to transform something into something else. Absent this, we are nothing more than rocks.
That said, I did learn a few things when preparing for this talk. Namely, I learned how many discrete disease there are. Did you know that we now have over 26,000 separate disease entities recognized by the medical profession and over 18,000 ‘global’ or ‘systemic’ disease entities? I did not and was shocked. Before I looked this up, I thought we had maybe a few thousand, ten thousand if I were being generous. Never once did I contemplate 26,000. That is absolutely insane. Worse yet, apparently there are over 20,000 pharmaceutical products currently on the market. A pill for every ill – almost.
With all of this knowledge, one might think we have advanced in our capacity for health and healing. One would be wrong. According to the latest research, 76% of the population deals with at least one chronic condition. And quite unironically, despite the endless discrimination of discrete diseases, most symptoms, from 25-75% according to one report, remain medically unexplained. We are drowning in distinctions where perhaps there should be none, or at least far fewer, and we are none the wiser or healthier for it.
From my perspective, I cannot help but wonder how many of these discrete diseases are not simply expressions of poor mitochondrial capacity? Sure, there are potentially millions of combinations of interactions between genetics and the lived environment that are likely to affect disease presentation, but is each set of symptoms really representative of a separate disease? From a mitochondrial perspective, probably not.
Moreover, if mitochondrial capacity is the key to health, then instead of searching for and naming each permutation of disease expression and creating new drugs for each, we could go back to the basics and ask ourselves – what do I need to be healthy and am I getting it? If I am ill, chances are I am missing something, probably lots of somethings and those missing components to health, along with the long list of environmental toxicants and genetic interactions that lessen mitochondrial capacity, are what is driving illness. Perhaps if we support the mitochondria and view health from that perspective, we can reduce the burden of disease while culling the impossible and growing list of supposedly discrete diseases.
Alas, none of that will happen, at least not on a scale that would make a difference. That said, perhaps my lectures and articles might help a few people reclaim their health and their family’s health. For me, that is a win.
Here is the latest.
Mitochondrial Capacity, Thiamine, and Dysautonomia
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.