Should birth control pills be available over the counter? In an unexpected and likely controversial position statement, the American College of Obstetrics and Gynecology (ACOG) announced its desire to see birth control pills sold over-the-counter (OTC). Stating that “oral contraceptives are very safe, and data show women can make these decisions for themselves.” Dr. Kavita Nanda who co-wrote ACOG’s paper, suggested that OTC birth control pills could reduce the rate unintended pregnancy significantly and save the nation $11 billion annually.
The bold move from prescription birth control pills to OTC is sure to remove barriers, provided the to-consumer pricing doesn’t skyrocket as is often the case when medications are sold OTC. Given the ongoing politicization of women’s reproductive health, returning the control of women’s health to women’s hands would be a laudable move and might even turn the volume down on current debates.
Imagine if birth control decisions were entirely personal and unhindered by political whims. Consider that greater access to birth control might be the key to reducing unintended or unwanted pregnancies. The availability of OTC birth control pills could be a very positive development for women’s health.
Are Oral Contraceptives Safe Enough to be OTC?
Unlike other over-the-counter medicines like ibuprofen that represent a single compound to be used for specific ailments – pain and inflammation – there are dozens of different birth control pills. Birth control pills are prescribed for an ever-increasing list of female ailments beyond simply preventing pregnancy. The question of whether birth control pills are safe must take into consideration the specific compound, dosage and woman. Some oral contraceptives have better safety profiles than others and some are quite dangerous (See Here).
Within the current market, determining which pill works best for which women, even in the doctor’s office, is a trial-and-error process. Much of the medication safety information is provided through the marketing channels of the product manufactures and–as has been reported here–those data are frequently biased and sometimes fraudulent. In that light, letting women self-select the appropriate birth control pill may be no worse than the current sub-optimal process.
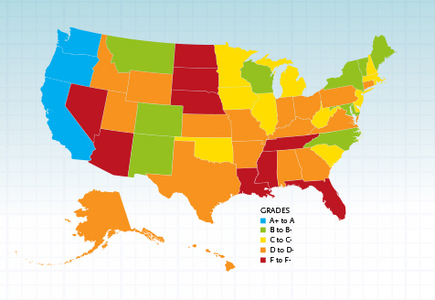
Over-the-Counter Birth Control in Other Countries
In other countries where for-prescription regulations are not enforced, oral contraceptives and other medications may be purchased over the counter already. Numerous studies suggest women are capable of self-screening for the contraindications or risk factors associated oral contraceptives. This supports the argument that women can manage their own oral contraceptive use, at least for its intended purpose of preventing pregnancy. Whether women would continue to utilize oral contraceptives for the myriad of other conditions for which these pills are currently prescribed, remains unclear.
Though no data exists for oral contraceptive usage, ease of access to non-prescription medication shows a direct relationship to the use and abuse of prescription medications and mortality by overdose. That is, countries with strictly enforced prescription drug laws (the US, Canada) have higher prescription use rates and higher mortality from overdose with no concomitant decrease in morbidity or mortality by disease or really any overall improvement in health. These data suggest that as prescription requirements loosen, use of more potent medications decreases. In the case of oral contraceptives, it is possible that OTC access could reduce the current trend of utilizing oral contraceptives as the magic pill that treats all reproductive disorders. This could be good thing for women, but it may not be a good thing for industry.
The Economics of Birth Control
Social and political benefits aside, women’s reproductive health is a market. Unlike other markets affected negatively by the economic downturn, the birth control market appears untouched, even bolstered. Sales of oral contraceptives are expected to reach $17.2 billion worldwide within the next few years. As one of the most commonly (over)prescribed medications in women’s health, oral contraceptives are used as a first line of treatment for a range of conditions unrelated to birth control. One has to wonder why the organization that controls access to this medication in the US would want to lose such a lucrative cash cow.
For millions of healthy women, the annual exam to renew one’s birth control prescription is the only reason to visit a physician. For the millions of other women with endometriosis, PCOS, PMS, and a host of other common conditions, oral contraceptives remain the first and sometimes only line of treatment. Selling oral contraceptives OTC would effectively remove those business segments from the gynecologist’s bottom line. When combined with other market segment encroachments on the business of obstetrics and gynecology (midwifery for healthy birth and maternal-fetal medicine for complicated birth), from a purely economic and albeit cynical standpoint, it is perplexing that that this organization would give away the largest remaining revenue stream of its members.
The economic drivers from the pharmaceutical industry’s perspective are no less perplexing. If priced correctly, over the counter oral contraceptives could increase sales–especially to lower income women who were previously locked out of the market by lack of insurance or access to healthcare providers. However, OTC access might also reduce the growing percentage of ‘off-label’ uses. For an industry unaccustomed to R&D in this sector, (why develop specialized therapeutics for the array of women’s health conditions, when birth control pills can be prescribed for all), the move to OTC could have serious financial ramifications.
There must an economic upside for these organizations, but for the life of me, I cannot figure it out.
Real Risk Study: Birth Control and Blood Clots
Lucine Health Sciences and Hormones Matter are conducting research to investigate the relationship between hormonal birth control and blood clots. If you or a loved one have suffered from a blood clot while using hormonal birth control, please consider participating. We are also looking for participants who have been using hormonal birth control for at least one year and have NOT had a blood clot, as well as women who have NEVER used hormonal birth control. For more information or to participate, click here.