My scientific training is in mucosal immunity and I have been interested in lipids which help to dampen inflammation in the body for over a decade. One of these anti-inflammatory lipids is called Lipoxin A4. Some such lipids are made at sites of inflammation and others are metabolized from fats taken in the diet. Inflammation is a natural response to a wound or an infection and should stop or “be resolved”. Otherwise, inflammation becomes chronic, surrounding tissue becomes damaged and dysfunctions occur, which can manifest in symptoms such as pain. Inflammation was first described many centuries ago but we still do not understand how it resolves. This is a fascinating field and deserves more attention as it could help further our understanding of major chronic diseases, including diabetes type 2, obesity, cardiovascular disease, cancer and endometriosis. However, inflammation is necessary for implantation to occur and it is also an integral part of menstruation, when the endometrium (lining of the uterus) degrades and is shed. Such processes must involve the resolution of inflammation and this is one of the reasons I consider the uterus a fascinating organ.
Endometriosis and Lipoxin A4 – New Possibilities
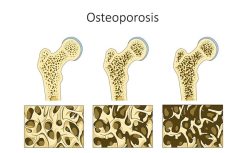
I first became interested in endometriosis in 2008 and began this research in 2009. It struck me that a good deal of endometriosis research is of relatively poor quality, with small study numbers and not very novel. Medical treatments for endometriosis are lacking and practically all target the hormonal system, resulting in unpleasant side effects. Medical treatments include progestagens, gonadotropin-releasing hormone agonists (for example Lupron) and oral contraceptives. However, the use of these therapeutics is limited due to the high cost, significant side effects (including premature menopause, decreased bone density and libido) and do not prevent disease recurrence after discontinuation of treatment. Additionally, each of these treatments preclude pregnancy. Therefore improved therapies, with fewer side effects, are necessary.
My group had been working on estrogen signaling and we observed, by chance, that Lipoxin A4, an anti-inflammatory molecule derived from the metabolism of fatty acids, had estrogenic properties. This was completely unexpected but when we looked at the structure of Lipoxin A4 it resembled that of Estriol, a weak estrogen. Using several different methods we confirmed that Lipoxin A4 did indeed act like an estrogen in the cells that line the uterus (endometrial epithelial cells) in vitro and that it also mediated effects similar to the most potent estrogen, estradiol, in the mouse uterus in vivo. So this was the discovery of a new hormone. Over twenty years ago, estriol had been shown to inhibit certain actions of estradiol. This is because they compete for the same receptor. Picture the hormone as a key and the receptor as a lock, in this case there are two keys trying to fit into the same lock. Lipoxin A4 also inhibited certain actions of estradiol.
As these dual characteristics, anti-estrogen actions and anti-inflammatory properties, are relevant to endometriosis, we decided to examine the effect of Lipoxin A4 in a mouse model of disease.
Lipoxin A4 and Endometriosis – The Research
Mouse models, though they do not mimic every aspect of the human disease, are useful to test potential drugs. These preclinical studies showed that Lipoxin A4 prevented endometriosis progression. We induced endometriosis in mice by transferring uterine tissue into donor mice. When looked at under a microscope these “lesions” resemble human lesions. We randomly divided mice into two groups: mice receiving Lipoxin A4 and mice receiving a vehicle, this is the liquid in which the drug (in this case Lipoxin A4) had been dissolved, which should not have an effect. Endometriotic lesions were smaller and inflammation was decreased in mice that had been administered Lipoxin A4 versus mice who had received vehicle. Many molecules involved in inflammation and cellular proliferation, which are also increased in endometriosis patients, were decreased by Lipoxin A4. Also, estrogen signaling was blunted. It is noteworthy that Lipoxin A4 did not alter the cycling of the mice, their cycle is shorter than the human menstrual cycle, and no other adverse effects were observed. Lipoxin A4 is an interesting molecule as it has never been associated with harmful effects and in this context can reduce inflammation and also impact estrogen-mediated signaling. These are two major components in the pathology of endometriosis.
Current research collaborations have as a goal to understand the role of Lipoxin A4 in human endometriosis; is more or less of it made? What is it doing and how?
The main problem here is that Lipoxin A4 is a short-lived molecule and is rapidly broken down. I hope that a more stable analog with the same functions can be synthesized which might eventually become a new, improved endometriosis therapy. I also hope that more discoveries regarding it’s role in the female reproductive tract will be made as it is almost certainly a significant player in this environment.
As referent biologist for a patient association I am saddened by how much women suffering from endometriosis endure and hope they can be heard and that they can participate in transdisciplinary research. For such a chronic and complex disease this would seem logical in order to move the field forward.