Longstanding Symptoms of Dysautonomia
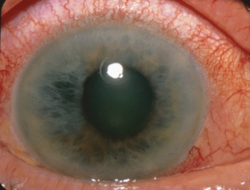
I am a 34-year-old male with symptoms of dysautonomia including small fiber neuropathy (SFN), postural orthostatic tachycardia syndrome (POTS), fatigue, insomnia, and problems with attention. I have had some of these symptoms for as long as I can remember but they have become worse after contracting COVID in December of 2021. I suspect I have issues with thiamine and possibly other nutrients.
History of Heavy Medication Use and Poor Diet
At around age 19, I felt what could be described as intracranial hypertension. I had multiple MRIs and CAT scans, but everything came back normal. At age 22, I began exhibiting signs of fatigue and insomnia coupled with anxiety. I most likely have some form of hypermobility too.
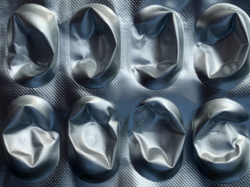
I was diagnosed with ADD and anxiety in my teens and prescribed Adderall and Prozac at the time. I was on those medications from the age of 16-25 years old. Then again from the age of 27-32 years old, I was given Adderall. I smoked and chewed tobacco until age 30 and was on and off hydrocortisone for poor adrenal function too. Evidently, adrenals can “fatigue” or become dysfunctional under high amounts of stress, even though blood cortisol was normal, saliva cortisol levels would always be low. Only functional doctors buy into this diagnosis.
I had strep and sinus infections a lot in my teens and early twenties and have probably had 40-50 doses of various antibiotics over the years. During this time, I worked out regularly with weight training and ice hockey. I was pretty competitive growing up. I would train 4-5 times a week and wake up early every Saturday to play hockey. I still work out around 5 days a week, mostly weight training now.
As a child and teenager, my diet was filled with carbs and crappy junk food like waffles and cereals and breads, and sweets. At around age 25, I began to eat a more healthy, paleo diet. I also began to avoid gluten. My diet currently consists of mostly carnivore/keto. I consume no alcohol at all. I did have a 10-year marijuana habit, from age 15-25, but I quit cold turkey years ago. I am currently taking Klonopin and have begun supplementing bone broth and a multivitamin. I have been taking 1mg per/day of Klonopin for a decade now. This may be affecting my symptoms.
Along Came COVID
In December of 2021, I got COVID and since then I have felt even worse. The COVID was mild. I took Ivermectin for 10 days and seemed to recover from the virus but all of my symptoms of dysautonomia have worsened.
Given my history, I am looking for advice on how to repair the damage I have done to myself with the poor diet, medications, and drugs. I have read about thiamine deficiency and it fits many of my symptoms but I am unsure how and where to begin. What else may be required?
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, and like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Photo by Gift Habeshaw on Unsplash.