The cytokine theory of disease states that an over production of cytokines causes the clinical manifestations of illness. Much effort has been expended to determine how cytokines are regulated in normal health. Cytokines play a broad role to help the immune system respond to diseases and drugs. Cytokines may be considered “good” when stimulating the immune system to fight a foreign pathogen or attack tumors. They may be considered “bad” when their expression causes inflammatory disease as in rheumatoid arthritis, asthma, or Crohn’s disease. What is often missed in these considerations is that the inflammatory response itself is dependent upon the proper functioning of the autonomic system, which is dependent upon mitochondrial capacity and mitochondrial capacity is dependent upon proper nutrition.
The Inflammatory Reflex
The inflammatory reflex is a physiological pathway in which the autonomic nervous system detects the presence of inflammatory stimuli and modulates cytokine production. Afferent signals to the brain are transmitted via the vagus nerve, activating reflex efferent signaling, that releases acetylcholine in the vicinity of macrophages within the reticuloendothelial system. The production of acetylcholine is crucial to the activity of this reflex which is known also as the cholinergic anti-inflammatory reflex.
The peripheral nervous and immune systems were traditionally thought of as serving separate functions, but new insights into neurogenic inflammation suggest that this is not the case. Nociceptor neurons possess many of the same recognition pathways for danger as immune cells. Understanding the interaction of peripheral neurons with immune cells may lead to the suppression of immunopathology. We now know that the nervous system, through the vagus nerve, can modulate the cytokine response induced by microbial invasion or tissue injury. This cholinergic anti-inflammatory pathway is mediated by nicotinic acetylcholine receptors on tissue macrophages, leading to decreased production of pro-inflammatory cytokines. Activation of the sympathetic nervous system also has anti-inflammatory effects.
The cholinergic anti-inflammatory pathway is part of the parasympathetic nervous system and it can be also entitled as an anti-inflammatory reflex. Stopping production of pro-inflammatory cytokines is its major task. Acetylcholinesterase terminates the neurotransmission, so cholinesterase inhibitors can be beneficial by the prolongation of the reflex. It depends on termination of the vagus nerve into blood, and the release of acetylcholine. Acetyl CoA, used for the synthesis of acetylcholine, is derived from mitochondrial pyruvate dehydrogenase and there is a small pool of choline with cholinergic nerve endings available for acetylcholine synthesis.
Cytokines and Covid-19
The clinical effects of Covid-19 are reported to be from a cytokine storm and clinical and laboratory features confirm. Like sepsis, severe Covid-19, is marked by an overwhelming inflammatory response, central to the development of lethal organ failure. Immunologic complications such as macrophage activation syndrome result in cytokine storm syndrome and acute respiratory distress syndrome, which may also occur in some patients. Although the physiological and pathological aspects of Covid-19 infection are poorly understood, current research progress indicates the effectiveness of anti-cytokine therapy. Given the role of autonomic dysfunction with human inflammatory diseases, including rheumatoid arthritis, diabetes and sepsis, it is possible that dysautonomia is an etiology in common to those diseases. Recent work indicates that vagal nerve signaling mechanisms are strongly influenced by the nutrient status. Nutrient delivery to the gut activates neuroendocrine mechanisms that control digestion, energy intake and utilization. Could nutrient status impact cytokine response?
Nutrition, Immunity, and Autonomic Function
The immune system protects the host from pathogenic organisms. It is always active, carrying out surveillance and its activity is enhanced if an individual becomes infected. Increased activity is accompanied by an increased rate of metabolism, requiring energy, substrates for biosynthesis and regulatory molecules, all of which are ultimately derived from diet. A number of vitamins and trace elements have key roles in supporting antibacterial and antiviral defense. Dietary approaches to achieve a healthy microbiota can also benefit the immune system. Thiamine is an essential cofactor for 4 enzymes involved in production of energy and the total body stores are relatively small. Thiamine deficiency (TD) can develop in patients undergoing acute metabolic stress, such as any form of severe infection, surgical procedures or severe trauma. TD can cause heart failure, peripheral neuropathy, Wernicke encephalopathy, gastrointestinal beriberi and/or the appearance of unexplained lactic acidosis. Consequently, clinicians need to consider TD in patients admitted to intensive care units.
Acetylcholine synthesis, the neurotransmitter used by the vagus nerve, depends on the presence of its precursors, acetyl coenzyme A (AcCoA) and choline. AcCoA is derived from mitochondrial pyruvate dehydrogenase, the cofactors for which are thiamine and magnesium. There is a small pool of choline within cholinergic nerve endings available for acetylcholine synthesis. The prevalence of TD in critically ill patients due to coronavirus disease 2019 is higher in patients with diabetes, a disease in which TD is common. When in excess, pyruvate and lactate that accumulate from TD, can increase the stabilization of the hypoxia-inducible 1-alpha transcription factor, independent of low oxygen. For this reason, TD causes what has been called pseudo-hypoxia. HIF stabilization activates pro-inflammatory cytokines.
An HIV positive woman, four days after recurrent episodes of vomiting, the herald of gastrointestinal beriberi, developed severe dysautonomia, frequently its earliest sign. TD, often overlooked, is frequent in HIV infected patients. Treatment with parenteral thiamine in this patient induced dramatic improvement within a few days.
A significant number of SARS-CoV-2 (COVID-19) pandemic patients have developed chronic symptoms lasting weeks or months, symptoms that are very similar to those described for myalgic encephalomyelitis/chronic fatigue syndrome. The current literature reveals an understanding of the role that mitochondria, oxidative stress and antioxidants may play in this syndrome.
Covid-19, Cytokinemia, and Thiamine
Although the inflammatory characteristics of the Covid-19 infection are incompletely understood, there is strong evidence of cytokinemia, typically found in macrophage activation syndrome and marking the degree of severity. Since we know that inflammation is controlled by the cholinergic anti-inflammatory reflex, it presents a potential for treatment by stimulation of the vagus nerve or by prolonging the action of its neurotransmitter, acetylcholine. Its synthesis is dependent on acetyl CoA from the citric acid cycle and choline from endogenous synthesis or diet. Thiamine is essential in processing glucose as the primary fuel of the brain and its deficiency causes beriberi, the prime example of an energy deficient disease. Although vitamin deficiency is considered to be rare in America because of vitamin enrichment by the food industry, it has been shown that a high ingestion of empty calories, particularly from carbohydrates, overwhelms the oxidative power of the micronutrients, particularly thiamine. We have called this high calorie malnutrition, a classical oxymoron since malnutrition is generally associated with absence of food, leading to starvation. Beriberi has a vast number of symptoms, none of which are pathognomonic. If TD is suspected, a common laboratory test is to measure the blood concentration of thiamine or the activity of the thiamine dependent enzyme transketolase, both of which are generally in the normal range even in moderate TD. This is because the thiamine content would be satisfactory for a diet containing a healthy concentration of calories. The calorie/micronutrient ratio is the important measure required.
The symptoms are produced by energy deficiency in the controls of the autonomic/endocrine axis in the hind brain that is particularly sensitive to TD. They are not crippling and the many sufferers are able to visit a physician where a series of laboratory studies are either nonspecific or normal. Beriberi has a long morbidity and a low mortality and is the prototype for dysautonomia in its early stages. The patient may appear to be relatively well and may even be obese. The usual and customary laboratory studies are usually normal or misleadingly nonspecific. The patient is often told that it is psychosomatic. The evidence suggests that high calorie malnutrition is common in America and may lead to energy deficiency, particularly in the brain, ensuring an essentially unfit individual. If and when such an individual is infected by the Covid -19 virus, there is insufficient energy to drive the complex activities of the cholinergic anti-inflammatory reflex. A deficiency of micronutrients, with a particular emphasis on thiamine, would ensure that the defenses of the body, organized and guided by the brain, would fail to perform an adequate protection from the invading pathogen.
Consider Thiamine for Covid-19
It has been shown in an animal study that thiamine tetrahydrofurfuryl disulfide (TTFD), an over the counter drug for attenuation of fatigue, improves energy metabolism, using the forced swimming test. The swimming duration using TTFD, was significantly longer than that of control rats and was not achieved using thiamine. The clinical use of TTFD has been reviewed. It is hypothesized that TD is precipitated in Covid-19 patients as in sepsis, both being examples of a severe form of energy requiring stress, as defined by Selye. Even if TD cannot be proved in the ER, a simple clinical trial with TTFD might expose the truth of the many symptoms attributed to the virus and particularly those experienced by the so-called “Longhaulers”. The polysymptomatic incidence is mindful of the clinical expression of beriberi. It is worth remembering that as long ago as 1936, Sir Rudolph Peters found that there was no difference in the respiration between TD and thiamine sufficient pigeon brain cells until glucose was added to the preparation. The cells with adequate thiamine immediately began to respire while there was no effect in the TD cells. He called this the catatorulin effect.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
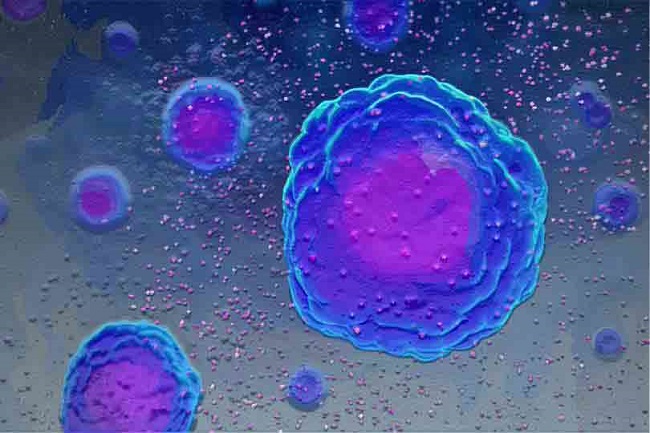
Image credit: www.scientificanimations.com, CC BY-SA 4.0, via Wikimedia Commons.










The clinical evidence strongly suggests that the virus robs the body, and particularly the brain, of energy. Megadose thiamine stimulates ATP synthesis and is probably therapeutic.
As far as cytokine overproduction is a problem, boron should be mentioned. An unjustly neglected microelement, essential for proper cytokine management https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC4712861/
Since thiamine deficiency affects mitochondrion it therefore affects literally everything; one wonders how could thiamine deficiency arise in modern humans. But as personal experience shows it does in fact happen, even with supposedly healthy & vitamin-full diet.
After chancing upon a twit mentioning this site I have tried supplementing thiamine; I greatly like the effects. I would like to thank every author of this site for their hugely needed work. Thank you!
Thank you for this excellent article, Dr. Lonsdale. I’m at the tail end of Long Covid and suspect I’ve been TD my whole life (most probably passed on from my mother).
I currently serve a large population of Long Haulers and ME/CFS/FMers and am holding a summit in coming months to explore Holistic Approaches to Long Covid/ME/CFS/FM.
Would you and/or Dr. Marrs be willing to speak? So far Dr. Sarah Myhill and Dr. Jacob Teitelbaum are among the speakers.
Your work has been a revelation for me and so many others that I see in HormonesMatter and FB groups and I believe it is VERY IMPORTANT to get this information out to those who need it…especially considering that such a large number of “newbies” are entering the scene because of damage sustained with Covid (now leading to TD and therefore Long Covid/ME/CFS/FM and other fun syndromes).
I serve a large community of Long Haulers and ME/CFS/FMers through my online Relief & Transformation course, through the Body Politic support group, and through various other Facebook groups online. My mission is to offer HOPE and HELP to these groups in tangible, workable ways to improve their lives by using a Holistic approach (mind, body, emotions, nutrition, etc). In addition to having gone through severe ME/CFS/FM myself and now Long Covid and having made my way out of them (well…almost with Long Covid…:), I’ve also been successfully coaching people with ME/CFS/FM for 20 years now (emotional intelligence, nutrition, pacing, etc). Though I now believe that the thiamine connection could be a missing piece from my clients’ and students’ recoveries.
I am happy to contact you to work out the specifics or you can reach me here: lorrie@livingfrominspiration.com
Thank you from the bottom of my heart for all you do and for having the cajones to get it out into the world.
Sincerely,
Lorrie Rivers