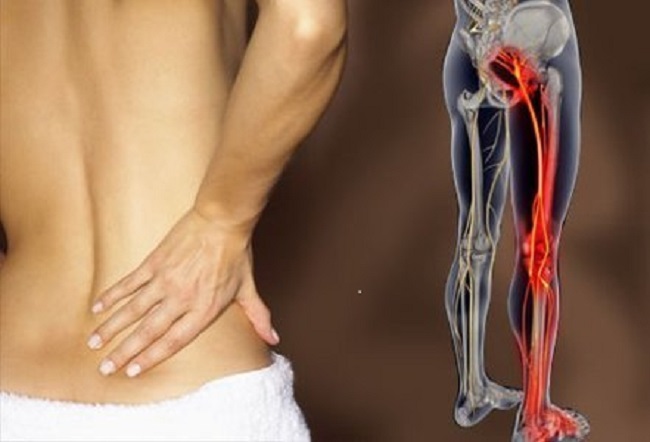
Chronic lower back discomfort. Stiff neck. Pelvic floor dysfunction such as pain with intercourse or urinary incontinence. Inability to sit squarely or for long periods of time. Pain with bowel movements. These are symptoms I see commonly grouped together in patients coming for treatment. What is the connection?
The tailbone.
Although it is a common site of injury, often taking the brunt of our many childhood and adult slip and falls, the tailbone is unfortunately an under-evaluated source of pain and dysfunction in both men and women. Once injured it can cause pain in sitting, pain with bowel movements, pelvic floor dysfunction, such as pain with intercourse, or even cause reactions up the spine, all the way to the neck and head.
What Is the Tailbone?
The coccyx, or tailbone, is the last piece of the spine. It is shaped like a triangle, and attaches to the sacrum by ligaments that run front, back, and both sides. To find your tailbone, just feel down your back, between the buttocks, until just above the opening of the anus.
In a healthy alignment it is mobile (moves slightly when pressed upon), center line, pain free, and continuous with the sacrum. However in a dysfunctional alignment it may be painful to touch it or the tissue around it, immobile, and even noticeably off-center. It may feel like it “points” deep into the body, rather than continuous with the rest of the spine.
How Does Tailbone Injury Happen?
Some patients know the moment they injured their tailbone. It is often a slip and fall, resulting in pain in sitting, and requiring the use of a donut pillow for some time until the irritation subsides. Usually, though, patients arriving with tailbone dysfunction cannot pinpoint a particular time that it was severely injured. They recall a multitude of childhood falls, none of which were particularly notable. And yet the tailbone is out of alignment and causing dysfunction.
Because the tailbone is attached to the rest of the spine by ligaments, it can be sprained just like any other joint. It can also be moved out of alignment. In many cases, a fall to the buttocks jams the tailbone forward, spraining the ligaments surrounding. As they heal the ligaments may scar down around the misaligned tailbone, effectively holding it rigidly out of place. Whether the fall was 2 months ago or 20 years ago, the tailbone may still be out of alignment.
What Are the Problems Associated With Tailbone Misalignment?
The most obvious symptom is coccydynia, or pain at the tailbone. However often patients have no pain at the tailbone until it is directly touched, and occasionally have no pain around it at all. This symptom may manifest as an inability to be comfortable in sitting. Often patients find themselves shifting from buttock to buttock in search of a comfortable position.
Pelvic floor dysfunction is common, as the pelvic floor muscles attach around the tailbone. Their ability to function optimally is affected by the positioning of the bones around them. Problems may include pain with intercourse, sensation of “tightness,” or pain with bowel movements. Bladder leaking may be aggravated by the inability of the pelvic floor to contract optimally.
Pain or tightness further up the spine is often a secondary symptom that patients don’t realize is connected. Since the spine and its contents are continuous from the skull to the tailbone, a tailbone out of place can affect alignment all the way up to the head. The most common two places I see this are the lower back and the suboccipital region, or area just below the skull on the back of the neck. Chronic nagging pain or tightness in these areas that shifts but never resolves despite care may be traced down to misalignment of the tailbone.
Treatment
The only way to treat most tailbone dysfunction is to work internally to mobilize the soft tissue around it and the joint itself. This is most directly done rectally, but sometimes can be accomplished vaginally. Pelvic floor physical therapists can do this, and some chiropractors and osteopaths may be trained to do it as well.
Why does this only work internally? Since the most common dysfunction of the tailbone is to be pushed forward by a fall to the buttocks, it needs to be mobilized in a posterior direction. This involves putting pressure on the front of the tailbone to move it back into place. In most cases the only way to access this angle on the tailbone is internally.
The therapist treating you should have specialized training to work internally, and have worked with tailbone issues before. As with all internal treatment, it is important that you feel comfortable and informed about what is happening. The practitioner will use a gloved and lubricated finger to mobilize your tailbone. You should be in a private room, draped for your comfort, and educated on what is found during evaluation and being done during treatment. Many patients are very anxious about being treated at or around the rectum. A skilled practitioner will be able to make your treatment as comfortable possible.
Does It Stay Fixed?
Usually, yes! Once the tailbone is mobilized it will not scar itself back into the old position unless there is a new injury. However, it is important to treat the ligaments, muscles, and bones around it as well, which may be contributing the dysfunction. Without treatment, these areas might pull the coccyx back out of alignment over time. The same concept applies to areas such as the lower back and the neck. Once the pressure of the misaligned tailbone is resolved, it is important to also treat the rest of the spine as it may have become tight or weak over time.
Often patients describe a sensation of “lightness” and ability to stand taller after being treated for tailbone dysfunction, as if a pressure was released. If you suspect that you have tailbone dysfunction, it is worth it to have an evaluation. You may find a connection piece in the puzzle for other symptoms you didn’t think were related.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
This post was published originally on Hormones Matter on September 10, 2014.