Inaccurate theories about how and why endometriosis develops are widely accepted by medical practitioners, despite much evidence against them. Acceptance of these theories leads to the perpetuation of medical therapies that do not work. It is important to understand the origins of endometriosis in order to move forward and develop effective treatments for this devastating disease.
Endometriosis and Sampson’s Theory
Endometriosis is defined as the presence of endometrium-like tissue outside of the uterine cavity. Many medical practitioners and lay press oversimplify this to state that endometriosis occurs when the lining of the uterus is found outside the uterine cavity. However, there are many publications enumerating the differences between endometriosis lesions and the endometrium found inside the uterus. Evidence for this goes back at least to 1981, and possibly earlier, and research into these differences is still ongoing. However, the common perception that endometriosis is merely endometrium outside of the uterus persists.
One prominently cited theory as to how endometriosis develops is known as Sampson’s theory. This theory suggests that retrograde menstruation, menstrual blood flowing backwards (away from the uterus) through the Fallopian tubes towards the pelvic cavity, deposits fragments of endometrium into the pelvis, which can then implant and grow into lesions.
There are numerous problems with this theory. First of all, there is no evidence that endometrial cells in the peritoneal fluid can attach to the lining of the pelvis (the peritoneum), and in addition, endometrial cells are not commonly present in peritoneal fluid. Furthermore, as stated earlier, there are many differences between the endometrium inside the uterus, and endometriosis lesions. In addition, 90 percent of women have retrograde menstruation, but only approximately 10 percent have endometriosis. Sampson’s theory cannot explain the presence of this disease in fetuses, in men, and in girls who have symptoms with the onset of puberty or even prior to puberty. And it cannot explain the presence of endometriosis in areas outside of the pelvis, such as the lungs and skin.
Alternate Theories – A Fetal Component
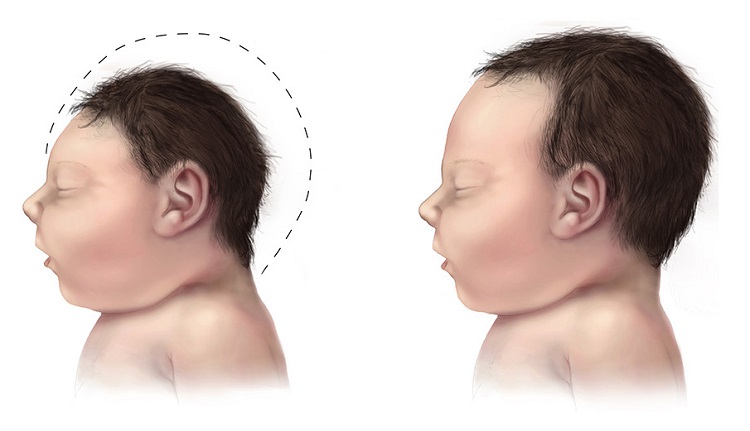
Alternate theories that fit better with the available evidence have been proposed, including metaplasia (changing of one cell type into another cell type), developmental defects (also known as Mullerianosis), genetic factors and environmental factors. However, no single theory has been proven to be correct, and most likely a combination of various influences contribute to the development of the disease. According to the current evidence, there is most likely some embryological component. The theory of Mullerianosis explains the development of endometriosis as endometrial tissue that was misplaced during fetal development, that later develops into endometriosis lesions. Evidence in support of this comes from the fact that endometriosis has been found in female fetuses with the same incidence as in women, about 10 percent.
The Persistence of Sampson’s Theory – A Safety Net for Inadequate Treatment
Why has Sampson’s theory continued to be so persistent despite all the evidence to the contrary? First, no alternative theory has been sufficiently proven enough to displace it, although certainly enough evidence against it exists that it ought to be displaced. Second, most doctors who treat endometriosis do not specialize in the disease, and the science behind its development is probably not something they have much interest in.
It is damaging to endometriosis patients to have Sampson’s theory continue to be accepted despite evidence to the contrary. It gives gynecologists a reason not to strive for complete removal of the disease from all organs, because there’s no point in trying to remove all of it, if it will just be re-implanted with the next period. Sampson’s theory provides justification for the high recurrence rates observed from surgeons who do not specialize in treating endometriosis.
However, surgeons who specialize in it, who carefully excise all disease, have shown that it is possible to have low recurrence rates following complete excision. This requires not only the knowledge of all the possible visual appearances of endometriosis, but the surgical ability to excise disease from areas most gynecologists cannot, such as bladder, ureters, intestines, or diaphragm.
Sampson’s Theory and Medications that Prevent Menstruation
Acceptance of Sampson’s theory gives pharmaceutical companies an excellent tool to convince doctors to prescribe medications that prevent menstruation. If Sampson’s theory is correct, then any hormonal treatment that stops women’s periods will treat endometriosis. Several drugs that are currently on the market can stop periods—Lupron and similar drugs, by inducing a menopausal state, and birth control pills, used continuously. However, as would be expected, since Sampson’s theory is not correct, these medications have never cured endometriosis. Some patients may experience temporary relief of symptoms, especially when the symptoms are primarily connected to having periods, but hormonal medical therapies do not treat the underlying disease.
The Origins of Disease Matter
Though debating disease origins may seem like an arcane point, not relevant to most endometriosis patients on a daily basis, it is highly relevant because it is so linked to the inadequate and ineffective treatment most patients receive. In order to truly move forward and make progress in how this disease is treated, wider recognition of Sampson’s theory as fatally flawed must occur. If endometriosis is present in the fetus, then it is an entirely different disease than one of retrograde menstruation. Understanding this is critical for better treatments options.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
lunar caustic, CC BY-SA 2.0, via Wikimedia Commons.
This article was published originally on October 2013.











Very good info, people need to know more about this and how parasites can be the cause of many diseases
I suffer with endometriosis and ovarian cysts – the only thing that helps (birth control made it worse) herbal hormone balancers that also are antibiotic/antiviral/anti-fungal/ and antiparasitic
I definitely think parasites are underrated by the health care professional – the best herbal formula for parasites that I have found is a mixtured tincture of wormwood, (green/fresh) black walnut hull, and red cloves
This mixture can kill over 100 diff kinds
That is great information… I have been looking for something like this for quite some time as to my wife has been dealing with a few of the same issues.
Philippa Bridge-Cook – when you refer to ‘endometriosis’ in fetuses can I ask what you mean exactly?
For more information you can read the reference linked in the article. Endometriosis is generally defined by pathology as glands and stroma in lesions outside of the uterus. This type of pathology has been found in female fetuses.
Dr Sinervo. You mention ‘likely’ origins of endometrosis as opposed to ‘definite’.The use of the plural indicates that you would consider more than one origin of potential tissue. Since there is room then for multiple theories of origin that might be concomitantly at play can I ask why this precludes altered endometrium in women with endometriosis as one such theory of several, especially given the different phenotypes of endometriosis?
This is an interesting article indeed! I have been asked by my gynac for a histerectomy 3 years back. I was on hormonal therapy for 5 years. Meanwhile I had to undergo removal of a surgical scar endometriosis (C- section) (Post operatively I had massive pain for hours and my hospital was not prepared for it. Post operative pain is not a joke). Since then my symptoms have reduced by 70 percent. I have also incorporated vegan diet, pelvic floor therapy, meditation, cardio workout, affirmations, staying more social. Adopting a superactive lifestyle does seem to contribute greatly. It’s been a year since I have not taken hormones therapy. However, recently I have noticed a new lesion on my skin next to my surgical scar. Last year my reports said diffused endometriosis throughout uterus blocking my fallopian tubes. However the pain is managable currently. If things go out of hands I am preparing for Uterine artery embolization. Hoping for the best. Don’t want to remove my precious organ which was once home to my baby.
Well pointed out! Many reasons for this disease, but pollution, stress and the over all bad food nowadays, are the most important factors, I think.
Well said and informative article. Conventional blinkered medical mindset thinking is focused on only the ‘WHAT’ and ‘HOW’ of disease in general, not just Endometriosis. Nobody even considers asking the ‘WHY’. Whytech does? I agree a likely varaible combination of the following Environmental, including pollution and others, medication, diet, emotional stress among others may all play a part. To find out the individual combinattion for a particular case lies in asking the right questions to the sufferer (source), to get to the ‘WHY’? Then you have ‘REAL’ targetable cause(s) to act on. Previous experience. Involved in ‘Endometriosis Research Trial’ in early 1990’s with the IFA International Federation of Aromatherapists, UK. Endometriosis Society, UK. provided the volunteers. The results were way beyond our expectations and confirmed by two top independent university research departments.
Wishing you all success in your endeavors.
PS. ‘Whytech’ is unrelated to the Endometriosis Research Trial.
Thank you for this interesting article. I am wondering about the fact that for example birthcontrol pills are not the cure for endometrioses. After several operations and a lot of pain, I now use the birthcontrol pill for 10 years already and I can say that I have no endometrioses since then and because I don’t have any periods anymore, also no pain in my life.
Birth control pills are not a cure because they do not treat the underlying disease. Some women may experience symptom relief on the birth control pill, especially if their pain is mostly with periods, and the pill is used continuously. For some women, no periods means no pain, but for others, their pain will persist on birth control pills because the endometriosis is still there. Also, it is comon to have a return of pain if you stop using the pill. As long as the endo lesions are still present, there is the potential for pain and inflammation.
It was nice to read your article. I’d said all those things and more during my 35 year career as an endometriosis surgeon, during which I saw only a little change in my profession’s view of the origin of endometriosis. My theory of origin, called Mulleriosis, was published in the late 1980’s and speaks to an embryologic origin of the disease in men and women.
Thank you Dr. Redwine! It’s a real shame for women with endo that the cycle of ineffective treatment can’t seem to be stopped.
So what is the approach to this treatment. I’ll be trying out visaane to stop my period and give me some relief.
Hormonal methods don’t treat the endo itself, they suppress the symptoms by stopping your period. The only treatment that is know to treat the actual endo and gives you a better chance of long term relief from symptoms is excision surgery. Many gynecologists don’t use this approach more. Are you in Canada or in Europe?
Visanne didn’t help me much. But led to severe depression. Got off of it and got Mirena. It holds the periods off and really have cramping. Switching it every year, since after year symptoms coming back. But that somewhat a solution I’ve found so far. Stage IV, two surgeries.
Finally! I’d love to participate in research. I have extensive endometriosis AND amniotic band syndrome. This makes so much sense in my particular case. Thank you!
I tried to take the Lupron side effects survey and it says it’s now closed? I would
Really like to share my experience. Thanks!
We just closed the survey yesterday to begin data analysis. We’ll be running it again soon. In the mean time, would you like to share your story in a post, published on the blog itself? If so, send us a note using this link. https://www.hormonesmatter.com/write-for-hormones-matter/
Thank you so much for this excellent article debunking the outdated notions associated with retrograde menses. It is unacceptable to use academic work from 1920 to excuse (the ongoing) poor treatment of this disease today. Keep up the great work and thank you for being a powerful, educated voice.
Thank you Heather!
Thank you Paula and Dr. Sinervo. I’m glad you liked the article!
Philippa – great article – it really hits on most of the important points regarding the inadequacy of sampson’s theory and the fact that either through metaplasia or through embryonic rest theory, these are likely the true origins of endometriosis. Thanks.
Great article. Spot on. I wish every doctor/ gynae could read this.