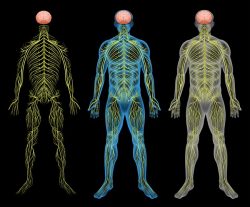
Physiological studies have long demonstrated the vital role of the autonomic nervous system in controlling blood pressure values. Beriberi, the classical disease due to thiamine deficiency, is the prototype example of dysautonomia in its early stages. The limbic system and brainstem are peculiarly sensitive to thiamine deficiency. Hypoxia is known to initiate sympathetic nervous system activity. Because thiamine deficiency has effects similar to those of hypoxia, these effects have been referred to in the literature as arising from pseudo-hypoxia.
There is much evidence that the common indulgence of empty calories, particularly those derived from simple carbohydrates and processed fats, is producing pathophysiologic brain effects due to what has been termed high calorie malnutrition. This form of malnutrition is totally different from that produced by starvation, the traditional form of malnutrition. Although the concentration of thiamine in the blood may be considered to be normal, it is only normal in the presence of a healthy diet. The excess of empty calories results in a high calorie/thiamine ratio that overwhelms the normal oxidative capacity associated with the presence of thiamine.
Patients suffering from high calorie malnutrition represent the “walking sick” of America. In its early stages it results in a polysymptomatic disease that defies our present concept of diagnosis. Traditional laboratory results may be quite normal or nonspecifically abnormal and the symptoms “written off” as psychosomatic. It may well be that some cases of hypertension, affecting millions, is part of the clinical effect produced by the dysautonomia of thiamine deficiency. The text that follows provides support for this hypothesis. It may also be true that failure to recognize the true etiology may lead over time to chronic brain disease in the untreated patient.
Autonomic Control of Blood Pressure
It has been well documented that the autonomic nervous system plays a key role in controlling blood pressure values. The hypothesis has been put forward that the origin, progression, and outcome of human hypertension are related to dysfunctional autonomic cardiovascular control, especially to abnormal activation of the sympathetic division. There is a consistent association between hypertension and pro-inflammatory cytokines of the innate and adaptive immune system. The sympathetic nervous system, a major determinant of hypertension, is pro-inflammatory, whereas the parasympathetic nerve activity dampens the inflammatory response through α7-nicotinic acetylcholine receptors. In the Goldblatt model of renal hypertension and the use of renal denervation in the treatment of drug-resistant hypertensive patients, autonomic mechanisms underpin the maintenance of this hypertension. Autonomic mechanisms initiate the development and maintenance of renal vascular hypertension. Obesity-associated overnutrition leads to neural inflammatory molecular changes, particularly in the hypothalamus, leading to elements of the metabolic syndrome. Increased sympathetic activation is a critical mediator.
Children, Hypertension, and Obesity
There are an increasing number of children diagnosed with primary hypertension, mainly in association with obesity. One of the factors considered is dysregulation of the autonomic nervous system. Emerging evidence suggests that the sympathetic branch plays a much broader role in the regulation of blood pressure, including the development and maintenance of sustained hypertension by a chronically elevated central sympathetic tone. A recent study examined the relationship between the autonomic nervous system dysfunction, anxiety and depression in hypertension. The sympathetic nervous system and arterial baroreceptor reflex control of renal sympathetic nerve activity has been proposed to play a role in long-term control of arterial pressure.
Abundant evidence supports the role of the sympathetic nervous system in the pathogenesis of obesity -related hypertension. The mechanisms are incompletely understood. A study supports the concept that increased renal sympathetic activity is the critical mechanism by which increased central sympathetic outflow initiates and maintains reductions in renal excretion function, resulting in obesity hypertension. Hypertension and obesity are risk factors for coronary heart disease in adults. Childhood weight problems and high blood pressure increase the risk of subsequent obesity and hypertension as an adult.
The Role of Hypoxia in Blood Pressure Regulation
Obstructive sleep apnea is one of the most common causes of hypertension in Western societies, causing chronic intermittent hypoxia. The normal homeostatic balance between HIF-1α-dependent pro-oxidant and HIF-2α dependent antioxidant enzymes is disrupted. Hypertension affects one in three United States adults and involves the integration of the actions of multiple organ systems, including the central nervous system, driving enhanced sympathetic outflow and increased blood pressure. There is increased understanding of hypothalamic activity in hypertension. Changes in the baroreflex and chemoreflex may contribute to the development of chronic hypertension observed in obstructive sleep apnea patients. Animal studies have identified induced hypoxic hypertension, but this is still conjectural in humans.
Thiamine Deficiency and Pseudo-hypoxia
Because mild to moderate thiamine deficiency results in pseudo-hypoxia in the limbic system and brainstem, emotional and stress reflexes of the autonomic nervous system are stimulated and exaggerated. Like chronic intermittent hypoxia that activates HIF-1 and suppresses HIF-2-mediated transcription, thiamine deficiency induces HIF-1α mediated gene expression similar to that observed in hypoxic stress. Thiamine deficiency induces an early, functionally significant central muscarinic cholinergic lesion that may be at least part of the reason for sympathetic overdrive. Details of the genetic determination in hypertension are poorly understood. A novel blood pressure locus that encodes a previously uncharacterized thiamine transporter has been reported, again perhaps emphasizing the importance of thiamine deficiency in hypertension. Evidence supports the likelihood that an increased cytosolic ratio of NADH/NAD+, caused by hyperglycemia, results in playing an important role in the pathogenesis of diabetic complications. Thiamine deficiency occurs in individuals with diabetes, leading to hyperglycemic-induced damage and oxidative stress. The potential benefit of long-term replacement is not yet known but may well reduce the cardiovascular risk and angioplasty complications. Thiamine deficiency should be considered in all patients with pulmonary hypertension of unknown origin.
Maternal hypertension is the most common medical disorder of pregnancy, varying from 4 to 6% of all pregnancies. The daily dose of 100 mg of thiamine has been given to over 1000 non-selected prenatals starting in the second and third trimesters. The expected number of toxemia patients in this group was well over 150, but the actual occurrence was zero.
Hypertension and High Calorie Malnutrition
Optimum nutrition is the level of intake that should promote the highest level of health. A deficit in nutrition may result in tissue depletion of essential nutrients that can lead to biochemical changes and eventually to clinical signs and symptoms. Adverse conditions prenatally increase the risk of cardiovascular disease, including hypertension. Obstructive sleep apnea increases over the course of pregnancy and is common during the third trimester. These adverse conditions have reportedly been completely prevented by the use of 100 mg of thiamine beginning even before pregnancy is confirmed. Thiamine deficiency, resulting in impaired oxidative metabolism, leads to a multifactorial cascade of events in the brain that include focal decreases in energy status, oxidative stress, blood-brain barrier disruption, glutamate-mediated excitotoxicity, amyloid deposition, immediate-early gene induction and inflammation.
Thiamine Tetrahydrofurfuryl Disulfide and Hypertension
This disulfide derivative of thiamine is the synthetic counterpart of allithiamine that occurs naturally in garlic. Allithiamine was discovered in Japan in 1951 and extensively researched by Japanese scientists. Experimental work in animals and human subjects revealed that its metabolic effect was much more powerful than the thiamine from which it was derived. Almost unknown in America, its therapeutic actions have been reviewed.
SHR rats are widely studied as a model of hypertension, exhibiting metabolic abnormalities that share features with the human metabolic syndrome. The SHR rat becomes hypertensive early in life and blood pressure continues to increase with age, often resulting in a cardiovascular event. Over the course of four months, blood pressure and body weight of two groups of SHR rats were monitored. The control group was fed normally and the TTFD group was given increasing doses of TTFD from 5 to 15 mg. There was a statistically significant reducing effect on the treated rats as compared with the controls. Of the 13 TTFD-supplemented rats, five showed a definite response with no rise in the expected blood pressure measurements, while the control group showed a 20 to 25 mm Hg increase in blood pressure across the experiment. The results showed that TTFD has a preventive effect on blood pressure in these genetically abnormal rats.
Thiamine Deficiency > Hypoxia > Hypertension
It has been shown in the above text that hypoxia and pseudo-hypoxia have virtually identical effects in the area of the brain that is peculiarly sensitive to thiamine deficiency. Since any phenomenon that causes inefficient oxygen consumption is dangerous to the organism, activation of the fight-or-flight reflex seems to be entirely logical. Repeated hypoxia in sleep apnea syndrome induces persistent chronic sympathetic dominance and is obviously an abnormal state of metabolism. It is possible that sleep apnea represents a combination of brainstem thiamine deficiency and recurrent obstructive hypoxia. Lonsdale and Marrs have published evidence that thiamine deficiency is widespread in the American population and that its effects in the brain are diverse and the resulting morbidity prolonged. Evidence could be accumulated by proving thiamine deficiency and attempting clinical trials with TTFD.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
This article was published originally on November 17, 2020.









What is your opinion on serum B1 test? My serum B1 is in “normal” range. But I’m wondering with the problems I have if I could actually need B1. Hypertension/ history of preeclampsia in pregnancy, (also pregnancy loss in the last 2 years), palpitations anxiety etc. ( anxiety and palpitations started After being on and stopping a diuretic and antidepressant that I think mightve caused some deficiencies ) I feel drained, muscle fatigue, I used to be dizzy all the time, now seldomly. Bp is hard to control. I feel like my nervous system is out if whack. But all my tests are “normal”. I’ve gone very low carb and have lost 65lbs so far. Many things have gotten better. But a few things need help, like bp. I definitely have something that’s low or missing! Looking for that root cause. Thanks!
They have a lot of false negatives. Moreover, there are number of mechanisms by which someone can be functionally deficient – e.g. need more thiamine than others. Because of the problems with testing many people will treat based upon symptoms rather than the labs.
This piqued my interest concerning my issues surrounding Thiamine deficiency. I suffer from spinocerebellar ataxia and my symptoms mimic those found in Worneckes Korkisov syndrome (sp?). I supplement with 100 of B1 every morning to counteract neurological symptoms, including tremors and shakiness.the irony of this is that I have been sober for 8 years and would have developed this anyway with the quantity of ethanol I was ingesting.
This does not mean much. Why not call it Wernicke since I gather that you are a recovered alcoholic? You should slowly increase thiamine to find the “right dose”. If and when you find it, increasing it will exacerbate symptoms.
Reply to Anthony. I presume that your growth was slow when you were getting growth hormone. Lack of growth is a very important sign of dysautonomia which occurs as a result of thiamine deficiency, the main cause of energy deficit in brain. You are getting thiamine and although the dose is unknown, it is non toxic and can be titrated to symptomatic response.
B12 requires energy to become active. If energy is in short supply, the inactive B12 and folate (also energy activated) both pile up uselessly in the blood, a strong indicator of ATP deficiency resulting from lack of thiamine. That is why a recent medical article that reported high blood levels of B12 and folate in a pregnant woman predicted an indication that the infant would become autistic after birth. This supports thiamine deficiency as a cause of autism, a fact that has recently been published elsewhere. This MS studied the thiamine content of breast milk and showed that thiamine deficient maternal malnutrition was a cause of ASD by inactivating B12 and folate as a result of thiamine deficiency.
Hi Dr. Lonsdale. Thank you (and Chandler) for sharing such valuable and needed information about thiamine and mitochondria. I’ve read your book. I have many autoimmune issues and have had very high blood pressure (120/200) for years (untreated). I’ve eaten organically for well over a decade but couldn’t really take much vitamins because I tend to react to them from mold intolerance and chemical sensitivities. I have been trying again to take b-complex 100 (I had to make my own mix from bulk to avoid fillers) and magnesium chloride and ttfd. So far I’m doing well on them. My question is after what is likely decades of thiamine deficiency, how much healing of the body should one expect? Do you think my blood pressure could come down to healthy levels over time?
Sorry for the typos, have been sick with the flu. I just noticed the bp is backwards, lol. Should be 200/120 average.
Bless your heart for all the work you have done through the years (just found out your age).
Many years of mental and physical fatigue spells “brain energy deficit”. Thiamine stimulates energy metabolism so a lengthy trial is warranted?
Dear Dr Lonsdale,
Would you think that trying thiamine supplementation is warranted in the following case?
20+ years vegetarian.
Long history of on-off constipation.
Always had salt cravings, eating much more salt than anyone else without apparent problems.
No other health issues for many years.
Diagnosed with severe iron-deficiency anemia 2 years ago (Hb <60 g/L).
Around same time: severe stress and intestinal issues (diarrhoea, bloating)
Since then, Fe + Mg + Zn + multivitamin and betaine-HCl supplementation. Also, gradual transition to very low-carbohydrate, meat-rich diet.
During the transition and supplementation period, frequent swelling of knuckles (arthritis), which has now stopped.
By now, Hb is in the normal range (though ferritin remains low), intestinal issues seem resolved.
But, within the last year, starting together with a newly stressful period, now very persistent acid reflux (never had it before).
At the same time, also odd, unidentified pain in knee over a few months, and later in arm muscle.
Brief period of feeling more energetic (seemed to coincide with switch to meat eating), but now feeling tired frequently (similar to before introduction of meat).
Increased feelings of stress and depression again.
Continuing supplementation with Mg; it seems large amounts are tolerated (and maybe necessary to prevent constipation).
Note: transition to a diet rich in meat also seems to be leading to frequent "oxalate dumping" symptoms.
Another question: Is there a risk of overdose with Allithiamine, since it is not water-soluble? Allithiamine is the form I can easily get here.
Thank you very much for all the writing on this site, it is very interesting!
Vegetarianism can lead to thiamine deficiency. Salt craving is classified as one of the dysautonomias and would strongly suggest TD. Allithiamine is only classified as fat soluble because it can enable the open ring form of thiamine to pass through the lipid barrier of the cell membrane. TD can produce constipation because it affects bowel neurotransmission. Yes a trial on megadose thiamine is justifiable.
Thank you so much for your reply Dr Lonsdale! I will trial the Allithiamine, and report back.
I am also planning to get your book, because the excerpts available on Google Books are very interesting.
I am very curious now about another thing, which I forgot to mention: It is a reaction I have always had after eating sugar and other simple carbohydrates (even fruits):
Around 2h after eating the sugar, I will get dizzy, sweaty, light-headed, completely unable to concentrate, desperately need to eat something to stop it. Others in my family also have this. If we eat the sugar together with fats, protein, fibre, it is much less likely to produce this reaction.
I have never been able to find out what could be the cause of this. Some of us were tested for diabetes, and found negative. My best hypothesis until now was that it was something bacterial. However, after reading many of your articles here, I wonder if this could also be part of thiamine deficiency. What do you think?
Look up the catatorulin effect in our book. It is indexed.
Dear dr Lonsdale,
I’m a 60 years old famale
Since i was 50 i started having some health problems.
Perhaps my main problem is the lack of balance but there are other disabling problems too. I have Vertigo dizziness, Digestion/digestive issues, nerve related pain in my leg.
I feel physically tired too, I am slightly bradycardic without playing sports.
I read your book, and I think thiamine can be useful to me. Lipothiamine or allithiamine are not available in my country so i started with 30mg intramuscular b1HCl. In ten days I had three injections. But I had a serious problem:
For the 48 hours after the injection I have some extrasystoles… can you explain me why I have this problem with such a small dose?
I would like to continue with b1 but I am scared of this problem
What do you think about? is it safe to take b1 for me?
I thank you for your time and for the immense work you do making it possible for everyone to know the benefits of b1
Sincerely
Elisa
You are experiencing paradox, not toxicity. You can read about paradox in the Hormones Matter Forum, Add manesium and B complex
Thanks for your reply dr lonsdale.
As per my update I have been using 300mg of allithiamine per day since August.
I still experience the lactic acid pain on my thighs with exercise and the index finger rsi pain.
Should I continue to increase the dose or any other suggestions?
Have you read any literature relating adolescent lack of GH to thiamine deficiency?
Antony’s wandering question is relatively easy to answer——why not just try thiamine or one of the forms of TTFD. The answer to “girl” is that a high B12 and/or folate is an indication of thiamine deficiency
Dr Lonsdale,
I wondered if you could offer some advise.
For many years I have been suffering with mental/physical fatigue.
The first noticeable “debilitating” system was in my thigh muscles, I suffer from a “burning” like sensation. similar to an over exertion squatting heavy weights in the gym producing lactic acid.
Each year i’d feel more pain in my thighs after little exertion. I was always off sick in bed for a week or two, by 2015 noticed I was usually off work several weeks per year where my body was completely wiped out and I was unable to get out of bed. fevers, flu, norovirus and other such related issues.
Prior to that as a child I had tons of energy, I was always good at athletics ; one of the fastests sprinters at school’s, hurdles and high and long jump.
By 2016 I had crashed completely, I was frequently urinating, always thirsty. Poor digestion – loose stools/diarrhea – ( My digestive system was never good since I was child and I believe I became more and more intolerant to foods).
Constantly absolutely exhausted, felt like my body was not able to produce ATP at all. I would have to lay in bed most of the day , sleep was unrefreshing By now I was struggling to stand statically for more than a minute or two. I could walk 0.5 mile or so, but I felt so wiped out.
My shoulders would burn, even sometimes using my phone would tire my muscles.
I had numerous GP visits, paid to see Physiotherapists, Endocrinologists, Chiropractors, Rheumatologists, Neurologists. They all had no idea and labelled it as a “post viral” issue and or CFS.
Luckily my brain still functioned well, I was able to work.
After researching answers myself and not giving up hope I came across the RCP. – For several years (3 years) I have been following the RCP (root cause protocol). Reducing my unbound iron, increasing magnesium, ferroxidase activity and other related vitamins from food. working out my food allergies brought me out of bed and functioning well, the clock has definitely turned back. But I lost a lot of weight (79kg -> 68kg, 6ft tall). No sugar, very low carb (as cant digest grains/rice/pasta well)
I am still unable to “exercise”, I can walk several miles but I am unable to climb many flights of stairs without my legs burning. Even 5 squats with no weight will cause me to feel lactic acid burn, which I am still trying to connect the dots too.
Recently I have had a sore right index finger (feels like RSI) for 5 months, if I rest it it feels okay, only sore under use. Most other symptoms have slowly resolved.
I read a lot of papers on thiamine and lots of posts by yourself, including various youtube videos by Elliot. I decided to start increasing thiamine via raw garlic several times a day and lots of pork. Slowly moving on to tiny amounts of Allithiamine by August 2020. I have been slowly titrating and am up to 300mg Allithiamine. I consume 1tsp of Bee pollen daily, several tsp of unfortified nutritional yeast, 300mg of Ox liver per week and recently added a whole food b complex (garden of life) to support the other B vitamins as you suggest. 600mg of magnesium per day, potassium and salt are also supplemented.
I definitely feel like i’ve shifted a gear, but this lactic acid issue in my legs has not gone away.
My question are:
1.) Does this sound like a Thiamine deficiency? – As a child I was unable to produce enough Growth hormone and had to be injected daily 0.25ml since 3->17. I was then tested and deemed normal at 17. I have not read any relation to this before, but wondered if you had come across anything?
Test Readings:
19.8 mU/L in 1987
in 2001 – 104 mU/L at 60 minutes on the ITT. GH then discontinued.
link to my bloods – https://docs.google.com/spreadsheets/d/1NIRFdw7F_ZF3Gj7PdkChn8S9QjMvFwd5bhOJNmTpi9I/edit?usp=sharing
as you can see i did have a high B12 reading, I also read this can be due to a thiamine deficiency as it’s not being utilised in the blood.
2.) I have not seen many report of supplementing Allithiamine over 300MG. I have read you state many times it is safe, but I don’t want to overdo it and cause other functions to go out of balance after all this progress.
3.) Would this b1 test be sufficient enough to determine a deficiency,m? if i understand it correctly they do apply thiamine to the blood to measure the difference – how long would i need to stop supplements before an accurate test?
https://www.biolab.co.uk/print.php/cmsid__biolab_test/Vitamin_B1_(Thiamine)_-_transketolase_activity
Thank you so much for all your research, articles and post replies.
High B12 can also be functional B12 deficiency. It was for me. I needed B12 injections in addition to the other things you’re trying. B12 is uniquely digested, and parenteral B12 can troubleshoot any malabsorption issues.
(I did also test positive for anti-intrinsic factor antibodies, but this test is only 60% sensitive! I was supplementing B1 at high doses the entire time.)
You have typical energy deficiency. Read the many posts on this subject on Hormones Matter.