Among the more consistent observations regarding COVID are disturbed platelet and endothelial -function, the time frame where severe illness presents (7-10 days into the infection), and the apparently self-reinforcing cycle of dysregulated immune function (cytokine storm). The prevailing hypothesis suggests that the SARS-CoV-2 pathogen causes platelet and monocyte hyper-activation and aggregation, inducing endothelial damage marked by micro-thrombi. These events initiate the formation of something called circulating immune complexes (CICs). The formation of CICs then drives excessive inflammation and further platelet activation, which, if not halted, becomes the self-reinforcing cycle of severely and ever-escalating immunopathology known as the cytokine storm. The net result of this mess can be everything from excessive lung damage and multi-organ damage to death. With this characterization in mind, the key questions that remain are 1) whether this cascade is unique to the SARS-COV-2 pathogen, 2) what sets off this cascade, and 3) why does all of this seem to kick in around days 7-10?
Is COVID Immunopathology Unique?
Currently, there is much debate as to whether this response is similar to other severe viral illnesses and simply more readily observed because of the scale of the pandemic or truly unique to the SARS-CoV-2 pathogen. Digging through the literature, it appears that while there are some unique features to this pathogen, as there are to all pathogens, neither the host response nor the time frame are particularly unique. The cascade may be simply ramped up in terms of severity and scale, and arguably, against a backdrop of increasingly poor metabolic health of the general population, while the time frame may reflect nothing more than the time it takes for mitochondrial exhaustion to develop.
Regarding the immunopathogenic cascades observed with COVID-19, we know that similar patterns are observed with other viral pathogens. For example, platelet and monocyte hyperactivation are common with severe flu and other viruses, as are endothelia damage and micro-thrombi and the CICs. Platelet and monocyte regulation are influenced in large part, by the severity of the threat, while the health of the host an his/her metabolic capacity determine homeostasis is managed and maintained. Similarly, the formation of CICs does not appear to unique to COVID. CICs are simply multiple antibodies and antigens bound together in one clump that circulate systemically to wreak havoc. They are very common with both bacterial and viral infection and in a variety of autoimmune conditions such as systemic lupus erythematosus and rheumatoid arthritis. Even the cytokine storm and subsequent multi-organ failure, viewed with much novelty at the onset of COVID, is common with severe illness or trauma and with various viral pathogens. A cytokine storm is an umbrella term used to describe the late phase host response to a variety of pathogens and stressors; the onset and duration of which vary according to the type of stressor and treatments administered. The self-reinforcing nature of hyper-cytokinemia may be linked more with host resources than with the actual pathogen. With the flu virus:
Clinical observations and animal experiments indicate that severe H5N1 and 1918 H1N1 virus disease is associated with cytokine dysregulation. However, because effects of multiple cycles of viral replication and host responses are inextricably intertwined, it is not clear whether cytokine dysregulation is a consequence of the severe disease (caused by direct viral damage) or contributes to pathology in its own right.
Although none these responses appears to be wholly unique and specifically related to the SARS-CoV-2 pathogen, the frequency with which this pathogen evokes these patterns, typically associated with only the most severe illnesses in the most severely compromised individuals cannot be discounted. Inasmuch as these are typical patterns, it is difficult not to question what about the interaction between this pathogen and the environment into which it proliferates is so different from other pandemics that precipitates such severe illness in so many individuals.
Host Mitochondrial Capacity
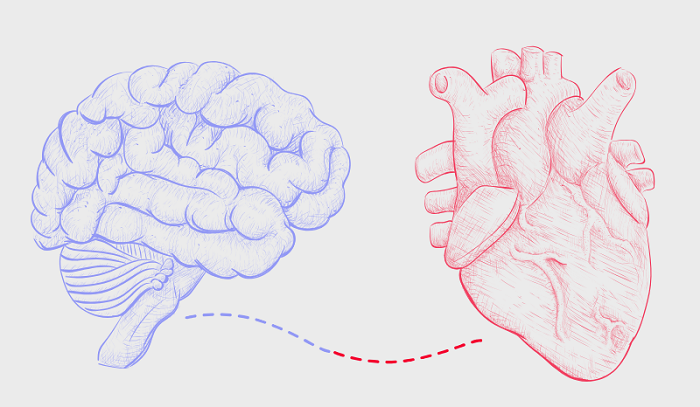
A paper published in 2015 found a similar, and perhaps even more rapid, progression of disturbed immune function and endothelial damage in cases of severe influenza A (IAV). Importantly, these events were attributed to mitochondrial collapse in the host, in part mediated by the pathogen, but mostly mediated by the host metabolic health. In other words, individuals with co-morbid health issues, the risk for mitochondrial collapse during a severe infection was greater than in healthy individuals. This makes sense when we consider that for survival, viral pathogens usurp and rewire host metabolic capacity e.g. mitochondrial energy production. In a healthy individual, this may not be problematic, but in a metabolically challenged individual the threat of mitochondrial energy collapse becomes greater because the very same pathways re-regulated by the virus are already stressed by existing illness, lifestyle, and diet. Specifically, in the case of IAV, and I suspect COVID and other severe viral pathogens, an enzyme called pyruvate dehydrogenase kinase (PDK – there are four isoforms of PDK with varying activity) is upregulated, while another enzyme called carnitine palmitoyltransferase II (CPT II) is downregulated. This limits mitochondrial energy (ATP) production capacity significantly by downregulating both glucose and fatty acid oxidation.
You may recall from previous posts, that glucose oxidation/oxidative phosphorylation begins in earnest with the enzyme complex called the pyruvate dehydrogenase complex (PDC). PDK, in its various isoforms, disables an important subunit of the PDC, which in turn reduces the amount of pyruvate that can be converted into acetyl-CoA and enter the tricarboxylic cycle (TCA; also called the Krebs or citric acid cycle) to produce ATP – energy. Simultaneously, these viruses downregulate CPT II, which limits the breakdown of long chain fatty-acids. Fatty acids are key fuel source for the mitochondria of many cells, including those of cardiomyocytes in the heart and endothelial cells that line the vasculature. That viral pathogens usurp these pathways is particularly problematic when one considers that these same patterns – upregulated PDK and downregulated CPT II (among others) are observed with obesity, diabetes, heart disease and cancer. With 476 million and 523 million people diagnosed with type 2 diabetes and cardiovascular disease respectively worldwide, this presents a problem.
From the standpoint of viral (or cancer cell) replication, this Warburg-like metabolic reprograming is a boon to the pathogen’s survival. It is not so helpful to the host, however, especially if the host’s metabolic capacity is already impaired with the aforementioned disease processes. It is entirely possible that, while COVID is certainly a serious viral pathogen, part of its capacity for destruction, lays not in the virus itself, but in the environment into which it enters. Data are clear that COVID severity is predicated on poor metabolic health. What is often missing from the conversation is how large a percentage of the worldwide population suffers from poor metabolic health. In the US, research estimates that only 12-20% of the population, depending criteria used, may be considered metabolically healthy.
Using a war analogy, with poor metabolic capacity/limited energy, everything is shifted towards fighting/winning the frontline battles e.g. activation of inflammatory cytokines. Few resources are allocated containing the damage e.g. activation of the anti-inflammatory cytokines. It is a metabolic blitz of sorts; hard, fast, and incredibly deadly, burning everything in its wake. The immune system recognizes the threat to survival and goes all in against the pathogen. The problem with such an approach is that there are no resources to tamp down the fighting as the enemy retreats and nothing to stop or even limit the damage to immediate landscape (tissue and organs). This, in turn, evokes a self-reinforcing cycle of increasing inflammation; one that become independent of the original response and further derails energy production.
This potentially fatal immune response has been termed the cytokine storm. Such hypercytokinemia alters the cellular redox state through different cytokine receptor and reduces the expression of our complex I subunits, oxygen consumption [7,8] and ATP synthesis in mitochondria, as well increasing mitochondrial O2_ production and the intracellular calcium concentration[Ca2þ]i [9] (Fig. 1). ATP depletion causes dissociation of zonula occludens- 1, an intracellular tight junction component, from the actin cytoskeleton and thus increases junctional permeability.
All of this is a result of poor metabolic fitness. With hyperglycemia, in particular, micronutrients deficiencies abound necessitating a shift from the primary and secondary pathways of glucose metabolism (OXPHOS and the pentose phosphate pathway) to tertiary pathways (the polyol/sorbitol, hexosamine, diacylglycerol/PKC, AGE pathways). This necessarily leads to a reduction in ATP, which in turn leads to micro – and microvascular cell damage. It is conceivable that the damage to vasculature presumed directly related to COVID, may have been there already and simply worsened or expedited with the addition of the virus. That we are seeing it so clearly now, may be only related to the scale of this pandemic.
Why the 7-10 Day Shift in Severity?
All of this appears to manifest around days 7-10. Before then, patients are said to be able to persevere from home, but between days 7-10, either the patient begins to recover or everything hits the fan and hospitalization is required. What underlies that critical shift in severity? Once again, mitochondrial collapse is likely to play a role. While altered metabolic capacity would affect the individual systemically, I believe that we see some of the more obvious issues evolving from platelet dysfunction.
The body carries about 150,000-450,000 platelets per liter of blood. In addition to their most well-known role in clotting and blood hemostasis, platelets are also active immune mediators (hence, their relationship with the circulating immune complexes), involved in wound healing, inflammation (elevated cytokine and cytokine storm if unregulated), infection control, endothelial function (platelet aggregation/clots adhere to endothelium causing stress and damage), and angiogenesis and tumor metastasis.
Managing these functions is done largely by the release of various signaling molecules, like serotonin and adenosine diphosphate (ADP) from dense granules within the platelets, and clotting, growth and immune factors like fibrinogen, platelet derived growth factor, and cytokines from the alpha granules. Platelet serotonin release may be particularly relevant to question of time and severity of COVID illness, as it occurs readily in damaged and dying platelets, drives immune reaction, and when severe enough, may elicit something called a serotonin storm, which symptomatically is almost identical to the cytokine storm (and to acute thiamine deficiency). In other words, when platelets are hyper-activated and spill their contents, if not tempered appropriately, there can be system-wide damage.
Importantly, platelets are quite small, have no nucleus, and carry only 5-8 mitochondria per cell, upon which they are critically dependent for energy production and survival. About 40% of platelet energy production is derived from the mitochondrial process called oxidative phosphorylation. The remaining 60% is derived from glycolysis. In both cases, however, micronutrients are required to power the various reactions involved in the production of ATP. Thiamine is top among them and is critical for both pathways. It is also commonly deficient in type 2 diabetes, heart disease and can be easily depleted in any severe illness or trauma.
I believe the purported gearshift from manageable to deadly results from the interplay between failing energy capacity, failing mitochondria, and platelet life and death cycles. This time frame parallels the natural lifecycle of the platelet and overlaps a cycle or two of platelet biogenesis from the megakaryocytes (5 days) suggesting problems with the equilibrium between platelet apoptosis and biogenesis. This time frame also represents a simple case of energy depletion, where not enough ATP is available to manage the immune response to the virus and maintain normal functions simultaneously. Seven to 10 days of a hypermetabolic state in individuals who, because of pre-existing metabolic disorders are likely poorly nourished in advance of the illness, and may not eat during this illness due to both the loss of smell and taste and severity of infection itself, will deplete energy reserves. This will affect immune response generally and platelet response specifically.
So Now What?
Feed the damned mitochondria! This may not prevent symptoms and other treatments may be required, but if we were to just support the damned mitochondria with the appropriate micronutrients, it would certainly help the patient to meet the energetic demands of the illness.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.










Amazing observation. I seen my father-in-law go down after about a week of illness at home. He did end up in the hospital and did not make it.
I love what you said, “Feed the damned mitochondria!”
Thank you so much for such an insightful and detailed article. If only the doctors in the hospital helped the patients with such therapies, many people might had a chance of surviving the COVID especially people who have metabolic conditions.