Zoey. The name means life. She is beautiful. She is fearfully and wonderfully made. She has been labeled otherwise. She has been labeled broken and put into a “syndrome box”. She drips out additional diagnoses like a leaky faucet.
She has accumulated these leaky faucets over the course of 11 years. She drips health problems out slowly with an audible, “DRIP….DRIP….DRIP”. Each year we find out something new, but most of the time the doctors won’t follow her on these new leaky faucets because they have put her in a “syndrome box”. They say, “Oh, Zoey is just this way because she has 2q23.1 microdeletion syndrome, White Sutton Syndrome, and Non-classic congenital adrenal hyperplasia (NCCAH). That means she won’t sleep well, she won’t speak, and she won’t have a normal gate. She won’t, she won’t, she won’t”.
This year, a few of her best doctors stopped putting her in a syndrome box because the leaky faucet finally broke. This story centers around being placed in a kidney reflux and hydronephrosis box for 11 years to “watch and wait” to see if her hydronephrosis and reflux would spontaneously go away as kids typically just grow out of this. This watching and waiting was my biggest mistake. Now the pipes are broken.
Genetic Box Labels
- 2q23.1 microdeletion syndrome (MBD5 deletion)
- 7.29 MB DNA deletion from 2q22.1 through 2q24.1
- Mosaic White Sutton Syndrome (POGZ mutation)
- Non-classic congenital adrenal hyperplasia (NCCAH)
Leaky Faucet Labels
- Autism
- Cerebral palsy
- Diffuse cerebral function with epileptic discharges
- Esophageal Dysmotility with pharyngeal backflow
- Dysphagia requiring g-tube (she can eat solids, but not liquids)
- Insomnia
- Keratosis Pilaris
- Onychotillomania
- Impaired speech
- Kidney Reflux
- Hydronephrosis
- Sleep Apnea
- Ataxia
- Fine motor delay
- Gross motor delay
- Constipation
- GERD
- Chronic ear infections
- Chronic toe and finger infections
- Submucosa cleft palate s/p repair
- Tethered cord syndrome s/p repair and now fatty infiltration of thecal sac.
- Severe astigmatism (diagnosed at age 11)
- Growth hormone deficiency
The First Sign of a Leaky Faucet
Zoey has always had a weird urinary pattern. Ever since Zoey was a baby, she wouldn’t urinate at night. In the morning, she would only urinate a small amount, about 100 ml. After propping her up for a few hours she would urinate more and more. This continues to this day. The urologist praised me for my potty training efforts in a child with Autism because she is dry at night and during the day, but I didn’t do anything to potty train Zoey. She can’t pee. I have to rub her tummy to help her release urine. I asked about this and I was told, “She only has mild hydronephrosis. We don’t cath kids when it’s mild.” Honestly, though, Zoey would never let me do a straight cath on her. So that’s not even an option, but in case you have a similar issue, there is a suprapubic type of catheter that looks like a g-tube port. I was never offered that. Here is her weird pee pattern:
- 8:00 AM 50 ml
- 10:00 AM 300 ml
- 12:00 PM 300 ml
- 2:00 PM 400 ml
- 5:00 PM 800 ml
- 8:00 PM 400 ml
She seems to make more urine in the afternoon. I think this is related to gravity. As she is more upright, her kidneys drain into her bladder. At night she still sleeps with her knees tucked under her and her butt up in the air which worsens her hydronephrosis. She wakes up every morning feeling nauseated. It used to subside within a couple of hours, but by age 10 this was all day.
A Second Leak: High Oxalates
Zoey’s urinary issue has been going on for quite some time. When she was two years old, I ran a Great Plains Lab OAT test on her. She had many gut related issues, and evidence of metabolic issues for which I started many different supplements, but she also had severely high oxalate.
My husband also suffers from repetitive calcium oxalate stone formation, so there may be a genetic component. At two years old, Zoey had a nephrologist confirm two tiny little kidney stones. I was told to increase her fluids to 2400 ml per day. As a dietitian, I also changed her diet completely. I put her on a low oxalate diet, and increased her citrate levels through magnesium citrate (which also helped her constipation) so that we could dissolve the stones. It worked.
My husband had damage to his kidneys from multiple stone formations and ultrasound lithotripsy, so I wanted to spare her kidneys from damage. I mentioned this to our nephrologist and he seemed to be not impressed. He said we didn’t need to follow up and that urology can manage her kidney issues. I wasn’t the advocate I am now, so I took that as a good sign that she was going to be just fine, and just did yearly follow ups with urology.
The Third Leak: High Testosterone and Early Puberty but Poor Growth
At age six, Zoey started what seemed to be early puberty. I asked her PCP to check hormone labs on her because being short and starting puberty early would mean she would stop growing too soon and be extremely short her whole life. He initially refused, but eventually acquiesced and ran the labs. She had very high testosterone levels. He sent us back to the same endocrinologist that told me she wasn’t growth hormone deficient. That endocrinologist said, “Let’s watch these labs for a bit.” We watched the labs for an entire year as the testosterone crept higher and higher.
I was so worried about testosterone hurting her body that I did a deep dive into journal articles and looked all along Zoey’s gene deletion to try to identify a gene deletion that was causing her hormone issues. I couldn’t find a single gene in her 7.29 MB deletion that could be a contributor. I was stumped. My then twelve year old daughter, after hearing me constantly talk about the damaging effects of testosterone and how Zoey will end up with a full beard, said, “Mama, if you are worried about Zoey, maybe you should be worried about me? I’ve been shaving my whole body and plucking thick hairs off of my chin.” And just like that, the older sister advocated for the younger sister.
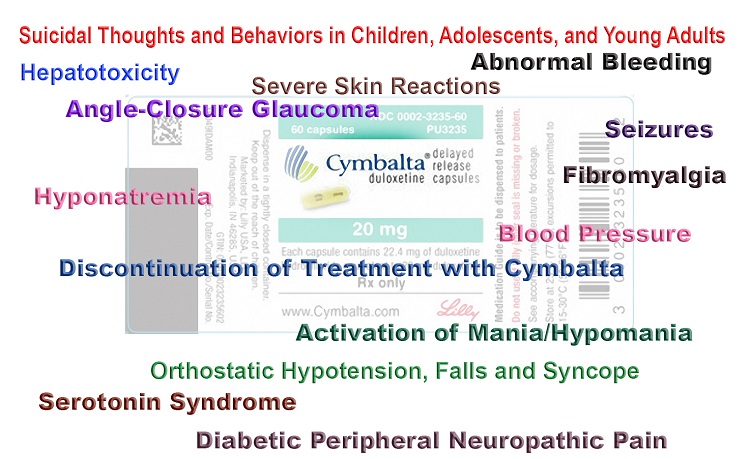
We went to a new endocrinologist and Zoey and her big sister were diagnosed with NCCAH. Their particular version of this disease is caused by mutations on each allele for the 21-hydroxylase gene. So it was genetics, after all, but it wasn’t within Zoey’s large gene deletion or related to her mosaic POGZ mutation. They don’t make cortisol efficiently. Instead, they make too much testosterone. The solution is to take hydrocortisone to meet cortisol needs and to suppress the hormone that triggers the adrenal glands to make cortisol. This lowers testosterone levels.
Having NCCAH can also cause a person to stop growing sooner in life so the new endocrinologist checked Zoey’s bone age. It was close to normal, but she obviously saw Zoey’s short stature. She said, “Why hasn’t she started on growth hormone?” I said, “Well, she definitely has a risk of deficiency because the mouse model of MBD5 deletion causes growth hormone deficiency, but our last endo said she didn’t have that because her IGF was normal.” The new endo just stared at me for a few seconds. I said, “And….he missed her NCCAH…and he didn’t test her correctly, right?” She said, “Let’s schedule a growth hormone stimulation test to see what’s going on.” Then I said, “And he is wrong isn’t he? Growth hormone does cross the blood brain barrier, doesn’t it?” She said, “Yes, but I can’t guarantee it will help her cognition.” Well, if you want to see the results of just one month of growth hormone on a person’s cognitive abilities, please go to my YouTube channel. Growth Hormone Isn’t Just for Height Gain.
Once Zoey started on growth hormone in 2020 she grew quickly. She actually grew about four inches in one year! By September of 2021, we achieved the results I wanted to see on her kidney reflux. Her ultrasound showed resolution of kidney reflux completely and growth of each kidney! Woohoo!! Urology wanted to discharge us because she had finally “grown out” of her reflux. I was so happy, but being a more cautious advocate than previously, I asked to continue to follow up, due to my husband’s history. I requested a follow up. Again, the physician refused at first, but acquiesced with coaxing.
In September of 2022, Zoey went back for her follow up appointment. I had some concerns to talk about, because Zoey’s morning urine was cloudy, but cleared up as the day went on. She was also struggling with peeing and crying in pain. They tested her urine and she didn’t have a UTI. We actually had gone to urgent care a few times to test for UTIs because it was an ongoing issue. She had no infections at all, but was having serious urinary symptoms and nausea. The ultrasound revealed that Zoey’s kidney reflux was back and that she wasn’t emptying her bladder. The urologist thought it was probably neurological in origin though because she didn’t have any evidence of UTI or cloudy urine in his office.
A Few More Leaks: Elevated Vitamin A Concentrations, More Oxalate Issues, and the Return of Kidney Reflux
In September 2018, after having a g-tube placed, and being on a blenderized diet, her GI doctor checked Zoey’s vitamin A for the first time, and it was 40 mcg/dl (normal is 26-49). I was not supplementing with vitamin A due to the difficulty of dispensing it, and the tube feeding I made had natural sources of vitamin A such as egg yolks. Her doctor was pleased that she wasn’t malnourished from a blenderized diet that was a bit limited due to being low oxalate.
As Zoey was able to eat orally, she started back on a low oxalate diet with small amounts of plantain chips or random bits of plantain flour based on a handout I found that indicated this was a low oxalate food. Her vitamin A was creeping up slowly, but still in the normal range until March 2021 when it was 59 mcg/dl (normal range: 26-49). When I saw it, I put myself on a “watch and wait”, but asked the gastroenterologist about it. She said she wasn’t concerned and that she sees it go up sometimes. They only treat low vitamin A. I was comforted by the fact that in January 2022 it had come down just a few points to 51 mcg/dl.
Zoey began to refuse our once a week snack of plantain chips. She would shake her head “No.” I should have realized then that there was a problem, but I thought it was because they were too hard to chew. She was struggling with painful baby teeth that she had ground to bits from bruxism. In August 2022, Zoey’s vitamin A had shot up again to 65 mcg/dl and I was quite alarmed. Looking back on this, it is easy to explain, as we had been giving her a full sandwich with two slices of bread that contained plantain flour, instead of just one half of a sandwich that had plantain flour.
With this change in diet, Zoey was extra tired all the time and she was having hypoglycemic episodes on and off. I asked her gastroenterologist about her increasing vitamin A and she recommended I ask the eye doctor to check Zoey’s eyes because I was concerned about the risk of a side effect of vitamin A toxicity, intracranial hypertension. Zoey had an eye checkup in August in September 2022 and all seemed fine except for a tiny change in her lenses.
From a Drip to a Flood
In January 2023, I decided to make banana muffins for Zoey only out of plantain flour and bananas. “So much better than white flour,” I thought. That week she asked for two at breakfast every morning, and because she had been so tired, I didn’t see a problem with it. Over the next five days she declined rapidly. She was walking as if she was drunk, and she couldn’t walk more than ten steps without having to sit down and rub her legs. She was telling us that she was sick by making sick sounds and asking for a thermometer, but she never had a temperature. She would tell us with her AAC, “headache, headache, vomit, vomit.”
After five days of plantain muffins, I went into her room to give morning meds and found her in her sleep safe bed lying in a puddle of vomit. When I opened the zipper compartment, she wretched and vomited some more. My heart immediately started to race because this is my child who aspirates liquids. She was going to aspirate her vomit! I turned her onto her side as she wretched some more. I wasn’t able to give her the hydrocortisone through her g-tube because she would just vomit it back up! I ran to get the inject-able hydrocortisone, solu-cortef injection, injected her, gave her Zofran, and rushed her to the emergency room. They started an IV and ran every test they could think of, but found nothing and diagnosed her with “vomiting”. Well, no one else in our family was sick or ever did get sick. While at the ER we left a urine sample and it was extremely cloudy. They checked it for a UTI, but said it was clean. They sent it off for cultures, but they came back normal later that week. After we left the hospital with a prescription for Zofran, the results were published to her medical portal. I saw what her urine and ultrasound of her bladder results said: Amorphous Crystals in Urine and Bladder Debris. Then it hit me. The only thing I had changed that week was plantain flour!!!
Hindsight has shown me that the cause of her returning kidney reflux the previous September was actually an increase in dietary oxalate from giving Zoey more plantain flour. I had been using the same handout for the past ten years from a kidney dietitian. The handout listed plantain flour as 1 mg of oxalate based on data from Harvard about 40 years ago. Well, plantain is now thought to have up to 524 mg per cup of flour. The oxalate in plantain flour actually was causing the kidney reflux as well as an alteration in Zoey’s ability to metabolize vitamin A leading to increasing serum vitamin A levels. Zoey is not metabolizing dietary vitamin A into retinoic acid, which has multiple functions throughout the body, and is the only form of Vitamin A that can leave the body.
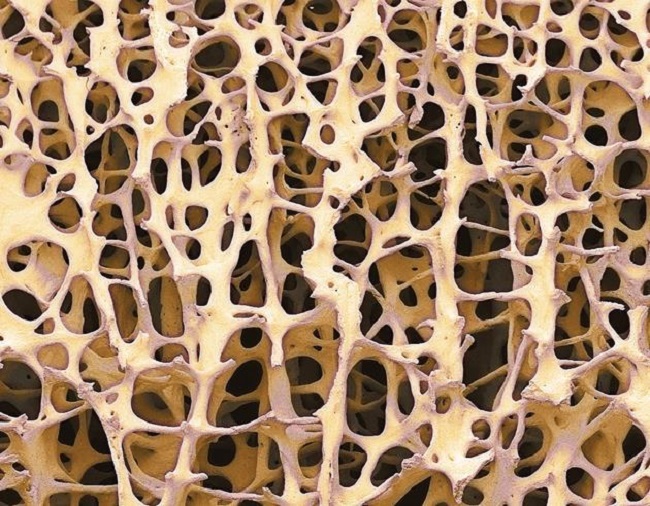
Now that we haven’t been giving Zoey plantain flour for the past three months, her kidney reflux has completely resolved. She still has cloudy urine, but that is related to hypercalciuria. Her serum vitamin A (retinol) levels remain high. I have learned that elevated retinol triggers calcium loss from bones due to alterations in osteoclast activity, although triggering of parathyroid hormone may also be involved. This causes hypercalciuria. My sweet girl has developed 10+ cavities in the past six months from rapidly depleting calcium stores. Her dentist was shocked. He joked that he didn’t know what to do…because he eats oxalate all the time. In addition, Zoey now has severe astigmatism and has to wear “coke bottle” glasses. Astigmatisms can be caused by retinoic toxicity. Zoey now be making retinoic acid to quickly. However, we are on a path of healing now and working out ways to help her metabolize vitamin A better in her body. She even can walk a straight line now and has energy!
History of Supplements
- Birth -1 years old: No extra vitamin supplements. Was using Neocate Junior, 1 scoop per feeding of breast milk (8 scoops per day usually).
- 1-2 years old: No supplements. During that time her diet was horribly high in oxalate because I didn’t know about them. Had GPL labs done at 2 years old showing hyperoxaluria and multiple vitamin issues.
- Age 2 to 6 years: Calcium Citrate 300 mg at all meals. No multivitamin because she was allergic to cobalt. She would break out in hives. She refused to take the separate vitamin supplements orally, and when I did give them to her, she would vomit, so I gave up because the vomiting was horrible for her.
- Age 6 to 6 years 8 months: She had a g-tube and was on a homemade blenderized diet where I added the vitamins listed below (except only 25 mg of thiamine) to her g-tube including the calcium citrate. She tolerated them fine in microdoses over the day through her g-tube.
- 6-11 years old: All vitamins were given via her enteral tube feeding bag with just water. It’s basically more of microdosing every 2 hours with 400 ml of vitamin infused water. If I push them all at once she vomits. During these 5 years, the routine was not consistent because I had to rely on a hired caregiver when I was at work. Again, during this time she only received 25mg of thiamine and not the amount on the list.
- Last three months: We have been consistent with the vitamins and the higher dose of thiamine and she has come back to life and appears to be recovering. I currently have Niacin on hold due to I’m exploring the relationship between NCCAH and the Kynurenine Pathway.
Current Supplements
- 500 mg Thiamine HCl
- 400 mcg 5-methyl folate
- 25 mg Pantothenic Acid
- 17 mg of B6 (Pyridoxal -5- Phosphate)
- 5 mg Niacin
- 5 mcg Biotin
- 25 mg Alpha Lipoic Acid
- 250 mg Vitamin C
- 500 mg Acetyl L-Carnitine
- 500 mg Glutathione
- 325 mg Calm Magnesium (Magnesium Malate)
- 2 Capsules of Mega Multi Mineral (half of a dose) contains:
- 500 mg of calcium amino acid chelate
- 11 mg potassium phosphate
- 5 mcg iodine (from potassium iodine and kelp)
- 5 mg Zinc
- 25 mg Copper
- 25 mcg selenium
- 5 mg Manganese
- 25 mcg chromium
- 25 mcg molybdenum
- 59 mg Potassium
- 5 mg Boric Acid
- 5 mcg Vanadium
- 25 mg Glutamic acid
Why My Kid?
Sometimes I wonder why it has to be my kid that suffers. Maybe it is only so that we can help other people. This experience has actually helped me with my own clients who have disabilities of various origin. Many of them are also suffering from this same inability to metabolize vitamin A. I was only able to spot this after I learned what the symptoms of this condition looks like by experiencing it with Zoey.
I tell Zoey every time that something I learned from her health circumstances helps another person. She will clasp her hands under her chin with one elbow up in the air and one elbow down and squeal in delight. It is the only thing that keeps us going. We love to help other people with nutrition. I definitely understood nutrition before Zoey was born, having been a dietitian for 10 years before she entered this world, but her health circumstances forced me to fine tune my nutrition knowledge. She made me dive deep into the research. She made me learn how to read metabolic tests such as plasma amino acid tests and urinary organic acid tests. I have been a dietitian for 22 years, but the past 11 years has turned me into a nutrition detective. I am thankful for all that my sweet Zoey Abigail has taught me.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.












I am 25 years old, diagnosed with NCCAH at 19 years old, and it is so frustrating I feel as though there are virtually no forums or much information about it. Thank you for sharing this, it was very interesting. I am so glad your daughter has a health-conscious mother like you.
Antonia, I’m so sorry your feel alone! I have a 17 year old and also Zoey with the same NCCAH. There is a facebook group run by the magic foundation that has a few adults with NCCAH in it. Here is a link https://www.facebook.com/groups/181860751861656
Also, you might need to read this post that I have on my own blog about NCCAH and the risk of stress dosing on NAD. Many NCCAH find stress dosing improves mood but it may be at the cost of NAD production. I think that most people with congenital adrenal hyperplasia are at risk for low NAD levels which will contribute to poor metabolism of vitamin A. https://weakthereforestrong.com/nad-disruption-and-hydrocortisone-therapy/
Also, having been diagnosed late in life, you may have always had very low levels of cortisol. Cortisol is needed to start the Kynurenine Pathway of NAD production. So…maybe you have felt low energy for a while? Let me know if you every need a chat.
Thank you so much for your encouragement. It’s been quite a struggle, but seeing her smile on a good day makes it all worth it. <3
I just wanted to say good job and never give up. You’re doing a great job. I have tears in my eyes because I recognize how you must feel somedays but always remember you’re such a blessing to your daughter. She is very lucky to have you as a mother.