Some individuals experience negative reactions and the worsening of symptoms when they begin thiamine repletion therapies using the more biologically available formulations like thiamine tetrahydrofurfuryl disulfide (TTFD). Dr. Lonsdale calls these paradoxical reactions. In this article, I examine the chemistry beyond these reactions and provide some hypotheses regarding why they happen and how to mitigate them.
TTFD Basics
In order to understand why some individuals react negatively to TTFD supplementation, it is essential to understand the basics behind TTFDs molecular configuration and how it is processed by cells. The primary difference between ordinary thiamine and TTFD is an extra chemical group called a mercaptan group. The mercaptan is derived from allicin, a compound found in garlic, and is connected to the thiamine molecule via a special sulfur-sulfur bond called a disulfide bond. Importantly, it is this unique chemical group that accounts for TTFD’s ability to traverse membranes in the body without the need for a transport system.
Upon ingestion, TTFD is mostly absorbed into the blood from the gastrointestinal tract in whole form as TTFD. As it travels through the blood, it can penetrate the brain and other organs without cellular transporters. One of the main sites of absorption is the red blood cells. Upon penetration of the red blood cell membrane, TTFD must first be processed or “broken apart” before it can release the thiamine contained within its chemical structure. After thiamine is released into the cell, the ancillary mercaptan group must also be processed and/or detoxified through alternative pathways. It is therefore theoretically plausible that errors involved in the processing of TTFD could contribute toward negative side effects or reactions to this nutrient.
How TTFD Is Processed Inside the Cell: The Glutathione Connection
Of the few molecules which have been shown to reduce TTFD, glutathione performs this function most effectively. As the cell’s primary antioxidant, glutathione is responsible for donating electrons to neutralize reactive oxygen species, and can either be found in its reduced form or its oxidized form. Once a reduced glutathione molecule (GSH) has donated its electron, it bridges with another to molecule to form oxidized glutathione (GSSG). GSSG is then recycled back to two GSH molecules through accepting electrons from NADPH via the enzyme glutathione reductase (vitamin B2 as FAD dependent). 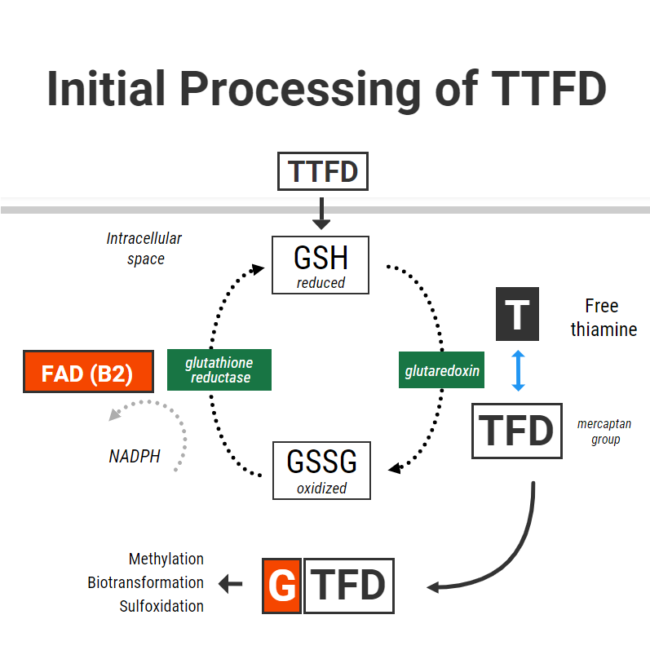
When TTFD enters cells, GSH in red blood cells chemically reduces TTFD via a process called “disulfide exchange” (presumably using a protein called glutaredoxin). Reduced glutathione becomes oxidized glutathione and TTFD “releases” thiamine to producing free thiamine inside the cell with an extra TFD mercaptan group left over.
The initial phase of processing TTFD requires that cells have enough reduced glutathione. Furthermore, the more GSH you have – the faster the rate of this reaction. So in simple terms, to obtain thiamine from TTFD the cells “use up” their reduced glutathione.
I recently had correspondence with one individual who only gained tolerance of TTFD after supplementing with 200mcg of selenium in the form of sodium selenite. Selenium supplementation in different forms has been shown to increase red blood cell GSH levels by up to 35%. This is thought to occur due to selenium’s ability increase glutathione synthesis through upregulating the enzyme gamma-glutamylcysteine synthetase. I suspect that poor glutathione status might be one of the reasons for benefit from selenium.
Having enough glutathione is clearly very important, but recycling it is also essential to maintain a pool of glutathione in its reduced form. Unfortunately TTFD can place a burden on this system, and this was demonstrated in one old study from Japan which showed that TTFD administration rapidly lowered red blood cell GSH. Interestingly enough, that same experiment showed that GSH levels were restored within 5-10 minutes. This restoration was accomplished by the vitamin B2 (as FAD)-dependent enzyme glutathione reductase, which donates electrons to GSSG with the reducing power of NADPH to recycle it back to two GSH.
What this basically means is that cells require a robust antioxidant system to properly process TTFD and return back to their original state. First, cells need enough of the antioxidant GSH to cleave thiamine. Second, cells also need to be able to recycle the oxidized glutathione back to its reduced state.
Poor Glutathione Status and Difficulty With TTFD
In someone who has poor glutathione (GSH) status, they might theoretically be less able to cleave thiamine from TTFD. There are many reasons why someone may have poor glutathione status:
- Low precursors (cysteine, glutamate, glycine)
- Chronic oxidative burden and/or inflammation
- Deficiencies in the nutrients required to generate, process, or utilize glutathione (B6 or selenium)
A total and/or functional riboflavin deficiency is the probably the most common culprit responsible for poor glutathione reductase activity. The glutathione reductase enzyme also requires adequate reducing power from NADPH to drive the enzymatic reaction. NADPH is derived from niacin (vitamin B3) and is generated in the pentose phosphate pathway which, ironically, requires the thiamine-dependent enzyme transketolase.
In the context of poor enzyme activity, without the reducing powder to drive GSSG back to GSH, the oxidized form of glutathione can theoretically drift towards the path of generating a free radical called the glutathione radical. This alone could further contributes to oxidative stress and cell damage.
Below is a hypothetical scenario to demonstrate my point:
- An individual suffers from long-term thiamine deficiency and has suboptimal riboflavin status
- Thiamine deficiency leads to lower activity of transketolase
- Low transketolase activity produces a lack of NADPH
- A lack of NADPH and a lack of FAD means that glutathione reductase is unable to efficiently recycle glutathione, which produces an imbalance between reduced/oxidized glutathione.
- Intracellular GSH is further lowered by taking high dose TTFD, and there is not enough enzyme activity to recycle it back
- Oxidative stress is made worse
In the above scenario, taking a high dose of TTFD may not be appropriate. Rather, restoring NADPH levels through supplementing with ordinary thiamine and supporting the glutathione system via other measures might be advised before starting with TTFD. Optimal riboflavin status is also necessary for the above processes to run smoothly.
Older research in Japan showed that TTFD supplementation could lead to a secondary B2 deficiency through increased urinary excretion. The increased need for glutathione reductase could at least also contribute to this effect. When taking TTFD, it has downstream effects on other nutrients. Hence, these supporting nutrients should also be taken in conjunction when someone is supplementing TTFD in high doses.
Some basic laboratory measurements of glutathione status include:
- Whole blood glutathione (low)
- Gamma-glutamyl-transpeptidase (high)
- Urinary pyroglutamic acid (high)
Furthermore, there are several functional markers which can be measured to assess riboflavin status, including direct measurement of red blood cell glutathione reductase activity:
- Urinary glutaric acid (high)
- Whole blood B2
- Urinary adipic, suberic, ethylmalonic acids (high)
- Urinary succinic acid (high) can also be suggestive along with a few other organic acids
- Erythrocyte glutathione reductase activity (low)
To summarize, the initial cellular processing of TTFD requires adequate levels of reduced glutathione. Glutathione becomes oxidized, and so TTFD has can have a depleting effect on GSH and increase the requirement for recycling. If there is insufficient active B2 (as FAD) or NADPH levels, glutathione is not likely to be recycled sufficiently and may lead to GSSG radical formation.
It is therefore possible that the glutathione-depleting effect of TTFD could be responsible for some of the side effects associated with supplementation. This is probably most applicable in individuals with poor glutathione recycling and underlying oxidative stress. Therefore, nutrient therapies that may support this initial phase of TTFD metabolism include:
- Selenium (improve GSH levels)
- Riboflavin (improve GSSG-GSH recycling)
- Niacin (increase NADPH)
- Ordinary thiamine (increase NAPH via PPP)
- NAC, glycine and/or glutathione TAKEN HOURS AWAY from TTFD (GSH precursors)
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
















I am taking half tab of 100 mg of the dissolving lozenge vitamin B1 by superior source. I take it on Monday, Wednesday and Friday for my Parkinson’s. The only thing I’ve seen Change is that I am not constipated any longer. It has not helped my tremors. I also get a little nauseated after taking it. So I think I’m going to need to cut my dosage again to 1/4 of a lozenge. I’m wondering if anyone else has tried the lozenges and what their experience was.
Elliot is a master of biochemistry explanations. Once again, the whole situation shows how hard it can be to bring back a healthy state of biochemistry inside a body once a pathological bifurcation event had occurred. B1 is rarely enough by itself, the whole spectrum of enzyme catalyzers is needed to be able to push the normalization process forward, continuously surmounting the plateau effect.
Hi
Any thought on this would be helpful.
I started THCL for a couple of weeks before adding TTFD. All seemed fine for a couple of weeks more with TTFD, bar some minor lip swelling and bumps/hives on the body when starting TTFD.
I had an MRI with gadolinium 3 weeks ago and since then the bumps/hives/itching have increased a lot and got worse each time I took TTFD and Benfotiamine.
I’ve had to take anti histamines every day since as the discomfort of the hives and serious itching has been unbearable.
I stopped all thiamine derivatives and i’m still experiencing the hives/itching though the past couple of days it has not been as much. I also added TMG since Monday to see if it helps but not sure yet as I started taking it at the same time as stopping TTFD/benfo.
Could this be a methylation issue or is there something else at play? Could the gadolinium have played a part or would these symptoms have gotten worse even if I didn’t have the gadolinium MRI?
Would topical thiamine also have this same issue. I have been applying a multi-b to my scalp and feeling really good.
Does low glutathione cause thiamine deficiency or is it the other way around?
I’ve been trying different kinds of supplements for my ME/CFS, some of these being thiamine supplements, choline supplements and also glutathione.
I have symptoms of dysautonomia, feels like I have low blood flow in my body. Heavy brain fog and slow gut motility, numbness and neuropathy. When I tried choline supplements for a few weeks such as Alpha GPC and Citicoline my motility improved and I got more normal bowel movements, as well as more energy. When I tried TTFD (with co-factors) for a few weeks I experienced a paradoxical reaction at first, but I then I started experiencing some improvements such as increased energy, dysautonomia symptoms improve, better gut motility and bowel movements and my neuropathy improved as well. Overall I’d say I felt 20%-30% better on the TTFD.
But when I try glutathione supplementation, either with Liposomal glutathione or precursors like NAC, I experience major improvements in a lot of my symptoms momentarily. My brain fog and cognition becomes a lot better and I start feeling like myself again before I got sick. Numbness also improves, it feels like the glutathione kicks circulation back into gear again throughout my body. But after some days of these improvements I crash, my brain fog, heavy head and body come back with a vengeance again and I start to feel even worse for a while.
I can’t make sense of it, obviously this means I’m likely glutathione impaired but does that also explain my possible thiamine and choline deficiencies too?
This person found that taking the liposomal glutathione and b12 and other Bs only occasionally helped her not to crash like taking them everyday.
https://forums.phoenixrising.me/threads/if-glutathione-supplements-are-so-bad-for-b12-deficiency-cases-why-does-liposomal-glutathione-help-me-so-much-momentarily.89782/
I have every symptom you have but I don’t seem to be able to tolerate TTFD right now. At the same time, antioxidants seem to immediately make me feel much worse. It feels like my body is stuck running on fat for fuel and antioxidants slow that process down to where I barely have enough energy to move or think. They also exarcerbate my feeling of severely impaired energy availibility.
In your case, I would try NRF2 promoters aka indirect antioxidants instead of direct ones like glutathione. The reason being that taking glutathione chronically may downregulate your endogenous antioxidant system as other direct antixoidants do (I believe, tho I could be wrong) which would be why you feel better at first but then end up even worse than you were at baseline. Examples of NRF2 promoters are flavonoids, such as [micronized trans isomer] resveratrol, hesperidin [methyl chalcone form], sulforaphane [get a good brand like Avmacol], etc.
Personally, I’m planning to try high thiamine hcl and/or thiamine cocarboxylase as I believe my chronic oxidative stress (I think from gout but nutrient deficiencies may be at play also) is making ttfd intolerable for now. I’m definitely interested to know if anyone has tried thiamine cocarboxylase in particular as it seems to be potentially very useful but relatively unknown.
This is something similar for me with regard to improvement with liposomal glutathione that is solid, but transient.
Thank you so much. May I ask why NAC is best taken a few hours away from TTFD?
May I ask why NAC is best taken hours away from TTFD for maximum benefit? I won’t hesitate to start implementing this method but I am curious as to what advantage taken them separately has. Thank you so much.
Because cysteine can reduce TTFD to thiamine+TFD mercaptan. This means that you would risk converting TTFD to ordinary thiamine in the gut before it is even absorbed, lessening the beneficial effects of the molecule
Thank you so much. I’m sorry for the repeated question. I was having connectivity issues and I thought it hadn’t posted. Would three hours be enough of a delay for the proper utilization of TTFD? Thank you so much
Does this also apply to glycine or just specifically to NAC?
Should we avoid taking magnesium glycinate at the same time as ttfd?
Michael, Allithiamine is TTFD. It’s just a brand name but it is the same stuff. On my bottle of Allithiamine, on the back it lists the TTFD as the main ingredient.
I discovered benfotiamine a few weeks ago, after having a reaction against a B multivitamin- my moods crashed and burned I was incredibly irritable and making a spectacle. I shortly thereafter discovered benfotiamine and I felt 100 times better. Fast forward 3 weeks later and the symptoms I had relief of – digestion of wheat products and beer was slowly going backwards. I have had a reversal followed by a forward movement with benfotiamine. I do worry its effects were short lived. However, there is consistency in that there is more energy in my muscles than before, breathing has improved, and brain fog is all but gone, aside from agitation in mood remaining. I have stayed with a lower dose as to not aggravate myself – things like sleep could be effected by it, but I am not 100% sure. I will stay on benfotiamine and keep you informed. Any suggestions or advice would be appreciated
Thanks,
Stop consuming wheat and beer? One is full of anti nutrients and causes gastrointestinal irritation in virtually everyone and one is a straight up poison.
Oh for pete’s sake. Wheat, if properly prepared isn’t full of “antinutrients” and to suggest it causes gastro irritation in “virtually everyone” is just absolute nonsense.
The same can be said for beer. It’s not a ‘straight up poison’. It’s not health food either, but a beer now and then never killed anyone. Sheesh…
Therapy route dot com has a great article on the root causes of lashing out.
Feel better soon.
This is a most interesting conversation. I thought that Overton’s explanation was superb because the fact is that the disulfide in TTFD has to be reduced at the cell membrane in order to produce an open ring compound. Another complex in the reaction is that the open thiazolium ring must close in the cytosol in order to produce an intact molecule of thiamine. The prosthetic group derived from TTFD has been well studied by Japanese investigators but it is still an unknown entity in regard to therapy. Obviously, the open ring transition that makes TTFD fat soluble is another complexity that does not take place with the S acyl group of thiamine derivatives. The prosthetic group is removed by an enzyme that occurs in the liver and kidney, so the resulting thiamine molecule that circulates in the blood is a normal thiamine molecule. It seems that it’s only advantage is that it passes through the intestinal wall as a complete molecule with its prosthetic group intact. Bettendorff has studied the difference between Benfotiamine (a S acyl derivative) and TTFD in mice and found no evidence of Benfo in the brain, whereas TTFD did cross the blood brain barrier. Whether you can extrapolate from mice to man raises another question, but if Bettendorff is correct, each has to be recognized for its difference in using it for therapy.
Dear Dr. Lonsdale
Thank you for your work!
Questions about Melatonin-the strongest antioxidant below.
I had all symptoms and paradoxical reactions, since I had Ciproxin 500 1999. The fatigue , heart-problems and sleepless and dreamless nights caused by this drug have lead to another desaster: toxified by construction chemicals, because I was not concentrated for a wrong moment, and high lactic acid and decreased muscle strength, high blood pressure-false normal blood pressure, and probably undiagnosed diabetes type 2 / endothelial underfunction
(According to Dr. Kraft, diabetes epidemic and you-might be interesting for you, to read his book, if you don’t know it already)
I had everything, Inclusive psychosis and the wrong treatment.And since Ciproxin, I feel nervous after coffee and green-tea.
Before that, I was able to run 8km with 130 m height-difference in 29 min. barefoot, weight 95 kg, unfortunately lactic acid was not measured at that time, but my anaerobic threshold was at 16.8 km at that time..
Now, I have 1.5 lactic acid already by only 40W on the ergometer, and there is no progress.
Body-temperature decreased to 34.8 C
GSH is decreased, ADP to ATP reconversion low, (If I take creatinephosphate, my bloodpressure goes to high. Endothelial underfunction.
Before, I was very calm, and able to relax deeply, now my hrv is bad, parasympathetic weak.
What Riboflavine supplementation is safe?
(I took BVitamins from BodyBio). P. Kane
Stomach acid lower than before, low protein level, 64
Ataxia
High LDL and small,dense LDL, low HDL
B6 levels are high always, maybe because Tryptophan goes down the Kynurenine-pathway?, instead to Serotonin/Melatonin since Ciproxine 500?
I was doing the glucose-test with insulin-assays according to Dr. Kraft.
(Fasting glucose/insuline, 75g of glucose, measuring again after 1,2,3,4 hours.)
Additionally, I had B Vitamins IV, interestingly, within the hour of B vitamins, LDL lowered about 10%, if I remember correctly.
Before I became conscious about the importance of Bvitamins, especially B1, because of your work, I have heard about the synthesis-pathway of Melatonin- the body’s strongest antioxidant., produced in every cell with mitochondria
( Dr. Russell Reiter, Dr. Been, and Dr. John Lieurance) YouTube Dr. Reiter is 60 years in Melatonin-research
UT San Antonio
Melatonin seems to recycle GSH, support SOD, CAT (preventing grey hair), transforms peroxynitrite, and is capable of at least 5 antioxidative steps… 95% of Melatonin is produced in mitochondria of all cells – not only in the pineal gland.(only the melatonin of the blood seemingly ends up in the blood)
In a study, I have seen, Melatonin prevented disbiosis in gut microbiom as result of stress.
Are microbes with better mitochondria dying more with antibiotics?
Or are microbes producing B Vitamins more suffering from antibiotics than other types of microbes, with lesser content of mitochondria?/producing toxins instead of beneficial substances?
Are microbes existent, which are able to switch on/off oxphos, ore are they either aerobic or anaerobic?
If you are interested in some melatonin-research I have collected, please let me know
Do you think,supplemented melatonin could prevent the paradoxical effects of b1 in its 3 forms?
Or should 5-HTP, Pantothenic acid, and Pyridoxal5-phosphate being supplemented, or 3. both?
Best regards from Zurich
Benjamin Kramer
Hey Everyone,
I’ve been reading the site for a while and just wanted to share a very interesting experience I’ve had this past week where I’ve inadvertently managed to completely stop my paradox reaction overnight. Before I get into it, I suppose I should give you a bit of background about how I got here.
I was, as much as I can remember and my parents tell me, a normal young child. Healthy, energetic, social, you name it. But at about 7 years of age, I suddenly started gaining a lot of weight along with developing ravenous carb cravings. A few years later I started developing issues with anger and irritability, and started getting into trouble in school. Around the age of 13, this disposition transformed into one of deep depression and anxiety instead. Ironically this worked in my favour as I went from being a troublemaker to the “good kid”. I also started having mild problems with short term memory and recall. Conversation was difficult for me as my ability to spontaneously think of things to say was diminished. Naturally this affected me socially, which only worsened the depression. Fortunately I did quite well in school and ended up getting into an Engineering program in university.
Up until this point, any problems I had were emotional, but at the age of 18 or 19, I started to develop physical symptoms. The first one was frequent urination. This was not an increase of the total volume of urine being voided, but rather frequent voids of small volumes. It was as if my bladder couldn’t fill up all the way, or wasn’t emptying all the way. Then I began to develop ataxia. Both of these symptoms were precipitated by smoking cannabis. At first they would only appear a few hours after smoking and then disappear, but then gradually they just lingered longer and longer after smoking until they were permanent, sans cannabis. Unfortunately I only made the association in retrospect. The ataxia got bad to the point where I’d feel embarrassed walking past someone on the sidewalk because I couldn’t maintain a straight line no matter how hard I tried, or I would stumble awkwardly (and I’m talking about being completely sober for weeks or months here).
A year or so after this I started to feel the beginnings of mental and physical fatigue. It was relatively mild at that point, but it affected my ability to study enough that I went to see the doctor. She was very nice (and sadly my last time dealing with a kind doctor with my issues) but all she found was that my B-12 was “kind of low but still in range”. I was offered injections but at the time just opted to get it in pill form since it was still in range.
All of the problems described so far continued to very slowly but surely progress. The depression and anxiety got worse, the ataxia got worse, the memory and recall got worse, the mental exhaustion got worse, and I started to develop a loss of interest and apathy toward many of the hobbies and interests I had loved before. I managed to finish school, albeit my good grades in first year had diminished to merely passing at this point. I found my first professional job and started working but the depression had gotten bad enough at this point that I caved in and went to the doctor for antidepressants. This was one of my biggest mistakes in life. The SSRI I was prescribed (Lexapro I believe, and then later Zoloft), precipitated all new symptoms and kicked my existing ones into overdrive. I could barely go outside as my urge to urinate was so frequent, my ataxia became comically bad. My short term memory stopped working. I also developed insomnia and sexual dysfunction. I was only able to stand it for 10 months before I weened myself off them. Unfortunately the new symptoms persisted at 50 or 60% of their initial levels.
Unfortunately I made the mistake of visiting another doctor for my now severe frequent urination. He tested for a UTI (as doctors had done in the past) and found nothing. However, he still prescribed me a course of antibiotics to “try just in case” – Ciprofloxacin to be exact. I only took three doses before all of my muscles and joints set on fire, and my Achilles tendons started burning. I could barely walk or sit down. Anxiety also reached a new level. Fortunately I mostly recovered from the effects of the antibiotic over the course of a year. About 80 or 90% back to previous baseline.
And then came the final insult to my body. I moved into a new apartment… with a serious mold problem. Mold which I hadn’t noticed when I toured the apartment. The overwhelming smell that the landlord had opened all the windows and doors to ventilate on that nice summer day. I moved in and was actually ok for the first two weeks as I attempted to clean it, and then it hit me. Aches all throughout my neck and shoulders, crushing fatigue, frequent urination flaring again, brain fog, all over malaise, food intolerances, weight gain, strong carb cravings, irritability, a profound apathy. As soon as I started to suspect it was the apartment, I went to go stay with my father for a week and got much better. I returned to the apartment and got sick again but it only took five days instead of two weeks this time. I was convinced and broke my lease and got out.
I look back and wonder if I have the worst luck in the world… or if normal healthy people encounter situations like all of the above too, but end up being perfectly fine.
It has been 6 years since then and I’ve been lucky to not have any more major trigger events in my life, but my symptoms persist. A few new ones have cropped up as well. Most recently are digestive issues with meat, and shortness of breath/tightness in my chest. I’ll save the story of visiting numerous doctors and being treated like dirt over the years trying to get help for another time. I’m 33 now. I’m just barely able to keep working, but “fortunately” the circumstances of this crazy year have put an end to the whole being employed situation.
Now, I believe the point of my post was to share my experience with B1, so I should probably get to that at some point! Over the years I’ve tried all sorts of promising treatments and supplements that led nowhere, as I’m sure many others reading have too. I finally stumbled across B1 and then this website and started reading. I’ve become pretty unoptimistic these days about trying new things, but the experiences and symptoms of some of the others here was too eerily similar to my own not to give it a try. I got some Allithiamine 6 weeks ago and have been taking it daily.
Surely enough, I was absolutely steamrolled by “paradox” effects. Every single symptom I had got considerably worse (but I noted that no new unrelated symptoms appeared). It seems quite apparent that Allithiamine is acting on me in a way that’s related to my existing condition and not just introducing new side effects of its own. Unfortunately after 5 weeks the paradox effects were not relenting in the slightest. I tried small 12.5mg doses, I tried large 1000mg doses, I skipped a day here and there, nothing helped, and the terrible feeling wasn’t letting up at all.
Then a few days ago I stumbled across a post on another website where someone mentioned they had tried Allithiamine. They said they did not get any benefit from it or any other form of thiamine unless they took it transdermally by opening the capsules, mixing it with body lotion, and applying it to the skin, in which case it had become a quite effective intervention for their fatigue issues. I decided what the hell I’ll try that. Well, I’m incredibly glad I did! The paradox effect is GONE. Overnight, for the first time in weeks I feel good! My fatigue is a little better than baseline instead of worse! The fog is improving instead of being worse! Instead of every symptom being much worse, I’m beginning to feel improvement!
I’ve been taking 150mg of Allithiamine from the capsules and mixing it with a liberal amount of Vaseline body lotion and rubbing it thoroughly into my belly area twice a day.
So why on earth is this helping immediately when taking it orally was exasperating the symptoms?
I have a hypothesis… mind you I have no idea what I’m talking about and I don’t mean to step on the toes of anyone that does, so please take this with a grain of salt.
Could it possibly be that taking Allithiamine orally creates a short lived initial spike in concentration that gets all sorts of thiamine dependant process started, and then the quick drop in concentration afterward causes an even greater functional deficiency when there’s not much thiamine left to sustain it? The only real difference I can imagine with taking it orally vs transdermally (aside from avoiding first pass metabolism or degradation in digestive tract) is that there would be a much longer lasting, more even concentration in the body.
Has anyone else here had experience with this?? Maybe it would be a worthwhile experiment for someone to try if they’re comfortable. I’d love to hear if this helps someone else too! I have energy for the first time in ages. I wouldn’t have been able to write something this long a few months ago, let alone a week ago. My brain fog is cut in half. That said, don’t let my enthusiasm fool you. I don’t feel anywhere near “better” or “normal”. I’ve got a long long way to go, but I’m optimistic for the first time in years.
I should also note that doing this doesn’t smell great. I don’t know if this is possible if you have to be at work or around other people who don’t appreciate you smelling like sulfur. It would be cool if it were possible to make some kind of nice clean allithiamine patch… if there is anything to this, but I’m getting a bit ahead of myself, haha. Thanks for reading.
Another speculative thought related to above; what if the reason a paradox reaction is a good predictor of positive outcome is that it indicates the body still has good capacity to utilize thiamine? That very capacity could be what makes taking intermittent, spiked doses of thiamine unpleasant. Like a well that’s been dry for years but the pump still works. As soon as there’s water again the pump runs like crazy and runs the well dry, you feel bad, but the good news it the pump still works. Maybe that makes sense? Again very vague and I have no biochemical reasoning behind any of it. Just some rambling that relates to my subjective experience.
I also wanted to add for the sake of completeness and anyone comparing symptoms, some others I have include: sensation of tightness/swelling in throat that comes and goes, uncomfortably dry eyes especially after eating, feeling incredibly out of it for the rest of the day if I awake before approx 6am (used to be able to wake up any time as long as total sleep hours were sufficient), vague uncomfortable feelings related to when/what type of food I eat, difficulty assembling thoughts and ideas verbally (but no problem in writing), premature grey hair, and lack of deep sleep – I just go from asleep to wide awake, combined with frequent awakening at night.
Another note: my initial paradox caused a gigantic increase in carb cravings, even more than was already normal. Now my appetite is reduced to the point where I have to deliberately remember to eat (it’s a choice instead of an irresistible craving)!
Hi Mike
Thank you for sharing.
Your sulfur-smell sounds like DMSO orally taken-interesting!
I recommend you, to make a bodybio-bloodtest. You will get a list of supplements, what to take when (I m a client) and do it since 2008
Check the videos from Russel Reiter, Dr. John Lieurance , and Dr. Been on Melatonin- the strongest antioxidant in the body. Helps to recycle GSH, converting peroxynitrite. Increases SOD etc.
Precursor is Serotonin-not built if inflammation is there.
5-HTP, B6 (pyridoxal-5 phosphate) and B5 (panthothenic acid) are required for Serotonin and Melatonin synthesis
Read the book diabetes epidemic from Dr. Kraft, you may have Diabetes Type 2
Check your fasting blood glucose, fasting insuline, HbA1c
Listen to Dr. Robert Lustig, Sugar-the bitter truth, and fructose 2.0 YouTube
Hey,
Really interested if this helped you in the long term Mike?
I want to take B1 but worried about my candida issues being exacerbated by taking these supplements orally.
Thanks
Thank you Elliot for this explanation. If I may add some personal observations that might be related although I don’t have The biochemical explanation. Before I use Thiamine I had a constellation of symptoms that seems to develop after taking any multivitamins especially if it is high in B complex, folate or trimethylglycine. With time I was able to negate the effect of the multivitamin or folate with either niacin or niacinamide and I have got to know all the specific symptoms of each and I can tell you that TTFD and to a far less degree Benfotiamine takes care of the multi/B complex, folate symptoms in a similar but far superior way than niacin or niacinamide. I have always thought that may be thiamine gets methylation started while niacin just suck up the excess methyl groups but honestly its just a theory with no scientific back up . Other observation I noticed is that thiamine taken with active B complex ( pyridoxal and methylfolate ) is far better than with folic acid or even food derived folate which even now while on thiamine can put me in a suboptimal state. Not sure if this is due to undiagnosed MTHFR mutation or something else. And if i may add that I had in the past tested high for B12 and I have always had signs of low b12 and folate . This last observation I think happened with Dr Derrick and a young patient too as I read in this site. And lastly , having a medical background myself, I Can’t believe I never thought of Intestinal beri beri as a cause of my severe GI symptoms ( diarrhea , achlorhydria , bloody mucous And picture of IBD with all the Inflammatory markers negative ) or thiamine as A cause of my refractory Tonsilitis ( negative throat swab ) and throat irritation or SIBO that magically disapeared on thiamine ! Also my glucose tolerance is back to normal after thiamine. God bless you all and my sincere thanks and gratitude extended to the remarkable Dr derrick and chandler.
One more observation is that although I have been on thiamine for some time And seems to be doing great on a balanced Maintenance doses I still Can generate what I Myself loosely call undermethylation symptoms from too much TTFD and overmethylation symptoms from Too much active B complex although I know its biochemically more complex than just methylation . But having just two arms to the Equation gives me reproducible results each time and In some sense reduce the confounding factors . I think Active b complex role here as opposed to folate/pyridoxine is that it can quickly control TTFD excess symptoms and due to its shorter half life stop there and my system gets balanced unless I play with doses again . Also I wanted to ask If R5P as opposed to riboflavin is any different because I have a bottle but never experimented with it.
This is fascinating! Biochemical “reasoning”, using the extensive knowledge of biochemists, is rapidly becoming the heart and soul of nutrient-based medicine and and rightly so. It is the foundation of a truly scientific medicine and should, in time, replace the treatment of symptoms using agents that are foreign to normal physiology and do more harm than good. I sincerely hope that biochemists will read this kind of information and add their expertise.
I am deeply impressed by this explanation of what I have for long called “paradox” or “refeeding syndrome”. What I have never been able to understand is why this paradox finally gives rise to benefit. I have always emphasized that thiamine is a team member of the vitamin and mineral complex. Hitherto, my explanation for paradox was that the individual had been in a state of catabolic metabolism and is suddenly making an effort to switch into anabolic metabolism However, that is not a sufficient explanation and this one by Overton makes a great deal of sense. There are mysteries surrounding TTFD but they can apparently be explained by a full understanding of the complex biochemistry surrounding oxidation. For the reader who has no knowledge of biochemistry, I would suggest that the vitamin complement is a necessity. However, the original research on garlic by Japanese investigators showed that allithiamine, the thiamine derivative had a much more potent biologic effect in animals than the thiamine from which it was derived. I am indebted to Overton for his biochemical reasoning which I think advances the principles embedded in nutrient-based medicine.
Thank you for you kind words.
Whether it can explain the reaction in its entirety or not – (I think not) – it could help to explain some of the horrible side effects.
Another set of interesting data relates to the next phases of TTFD/TFD clearance and specifically involves the depletion of SAM-e. TFD is further conjugated with MORE GSH and then methylated via SAMe to be later cleared. Hence, increasing requirement for methylation could help to explain the tendency toward low folate after months on TTFD (?). Also, the reaction of extreme anxiety or depression in some who take TTFD from the first time (?). The next article is about that set of processes.
After that secondary phase, the methylated product is run through sulfoxidation in liver microsomes (most likely the CYP450 system) to generate sulfoxide/sulfone-type molecules like you have explained in some previous papers. It also generates some inorganic sulfate.
The question I am trying to get my head around is this: HOW does molybdenum help with “sulfur/sulfite” types reactions caused by TTFD? I have seen it on too many occasions to think it as a coincidence.
Molybdenum is great for clearing sulfite to sulfate though the sulfite oxidase enzymes. The problem is, I don’t understand enough about sulfur chemistry to see how sulfoxides and sulfones can generate sulfites. Tried searching for many hours on Pubmed to find the pathway by which sulfoxide/sulfone –> sulfite, but have been unlucky so far.
Finding that link (if there is a link) will be an important piece of the puzzle, because then there will be good rationale for not only B spectrum addition, but also laying the groundwork with specific minerals (selenium and molybdenum) to improve tolerance of TTFD for beginners!
Perhaps aldehyde oxidase for the sulfoxides. This is also a molybdenum dependent enzyme.
I noticed that many drug candidates with sulfoxides are tested to see if they are vulnerable to metabolism by aldehyde oxidase which makes them ineffective due to a high clearance rate. That lead to this –
“AOX is capable of both oxidative and reductive transformations of a wide range of compounds. AOX oxidative substrates include aldehydes, aromatic heterocycles, iminium ions, and azaheterocycles; AOX reductive substrates include sulfoxides, nitro compounds, N-oxides, nitrates, nitrites, and molecular oxygen”
https://dmd.aspetjournals.org/content/47/5/473
Along the same lines xanthine oxidase, also moly dependent, can come into play
“The present study provides evidence that guinea pig and rabbit liver aldehyde oxidase (EC 1.2.3.1) in the presence of its electron donors such as aldehydes or N-heterocyclic compounds functions as a sulfoxide reductase towards sulindac and other sulfoxide compounds. In addition, the study shows that a combination of liver aldehyde oxidase and milk xanthine oxidase also exhibits sulfoxide reductase activity in the presence of xanthine, and electron donor of xanthine oxidase. Based on these facts, we propose a new electron-transfer system consisting of these two flavoenzymes.””
https://pubmed.ncbi.nlm.nih.gov/4051501/
I just had a Vibrant America Micronutrients test and the Genova ION 40 panel done at the same time. I had the results reviewed by Chris Masterjohn and funny enough I think this is exactly what is happening. My glutathione on the ION 40 panel was extremely low and this is what stuck out most, my riboflavin was low and my B6 was a little low as well. At the time of testing, I had frozen my TTFD supplementation to 100 mg every other day along with Thorne’s Basic B Complex every day. I’m thinking of switching to Thiamine HcL, adding Riboflavin and P5P, NAC and Glutathione. Will see how things develop.
Riboflavin requires a functioning thyroid to be converted into FMN & FAD. I believe iodine, selenium and molybdenum are important for this stage of converting plain riboflavin into the coenzymes FMN, FAD.
Glutathione cannot be recycled without FMN/FAD.
B2 has to be functional for B6 to be functional.
I wouldn’t take TTFD until you fix your glutathione and riboflavin status.
Thanks for your explanation. Does this apply to Benfotiamine also just as for TTFDs ?
No, the breakdown of TTFD is completely different to the breakdown of benfotiamine.
Benfotiamine is primarily broken down in the liver, and then transported in the blood as normal thiamine. Benfotiamine DOES deplete certain nutrients in the liver (glycine if I remember correctly, but I could be wrong about that)
The above mechanism applies specifically to TTFD
HI Doc ! i am from Nepal We have Thiamine HCL only .Can i take this too ?
All this is getting way too complicated. It starts with needing some thiamine and ends with needing to take several other supplements all at the right amounts at the right times for who knows how long. Surely there is something more simpler and easier to implement.
For many, it is quite simple.
However, for people who are chronically sick with multiple complex health conditions, simple solutions are not always sufficient. It would be great if it were the case, but it seems as though complex health conditions sometimes require complex solutions!
Which is quite unfortunate for those of us who are so chronically ill and need it’s benefits the most. I’m wondering if nebulized glutathione several times a week (just guessing on that amount), along with Selenium (to build reserves, if that’s even possible) prior to starting a regimin of TTFD would prevent the undesirable side effects? I have no training in this field, I’m just asking for your thoughts based on what’s contained in the article. Also, this is my first time here and I like what I’m reading. I read about mega doses of B1 to treat dogs with varying nerve damage to the myelin sheath, they’d lost most of the mobility in their hind legs. The B1 restored nearly all mobility and slowed progression of their disease, even if it’s not a “cure”. My issues (too lengthy to chronicle) seem to have B1 deficiency as a cause and/or are exacerbated by the deficiency. So after reading about the dogs on a site (of which I have zero affiliation) called Orthomolecular News, I did a search for more detailed info and discovered you. I realize your posting was 2 yrs ago, but I hope this thread is still active & that you’ll respond. Thank you
I tend to agree. At first I was really excited to try TTFD, as I have a multitude of physical and psychological symptoms. Now I’m almost scared of it. I’ve taken other forms of niacin before, with no problem, including benfotiamine. Will probably try the TTFD at a very low dose, and slowly titrate up
Hi Elliot,
that is so interesting, thank you for researching it and putting it together!
I wonder though why (according to Dr. Lonsdale) having a paradoxical reaction is a good sign and typically means that the person will improve with the TTFD treatment. And why this paradoxical reaction should subside after a month or so.
Anna
Good question.
I don’t think the above mechanism can explain all aspects of the paradoxical reaction. As far as I am aware, other forms of thiamine do not have this effect on glutathione, so I think it merely applies to TTFD.
In the context of TTFD – perhaps cells have ways of adapting to the changes in the antioxidant system. For example, the consistent intake of TTFD will upregulate the enzymes using thiamine as a cofactor and will eventually promote enhanced glutathione recycling. For some, however, they can never quite get to a point where they can process the molecule without doing some of the groundwork beforehand.
That does sound plausible. I was also thinking how Dr. Lonsdale always recommends taking a b-complex and multivitamin too, so it could well be that after a month of b-complex and multivitamin levels of b2, selenium, molybdenium and other contributing nutrients have reached a level that helps restore/recycle glutathione which then allows proper processing of TTFD.
This is a fascinating concept. In our metronidazole toxicity support group, we have seen patients with paradoxical reactions, either when starting general water soluble (regular) thiamine or when switching to a TTFD, typically severe and/or chronic cases. I will forward this, as it will be beneficial, especially for those who have issues with TTFD but not regular thiamine.
I have seen this too all forms of thiamine, especially in individuals with longstanding health issues that were precipitated or exacerbated by pharmaceuticals. Many folks have to microdose thiamine and other nutrients for a period of time in order to tolerate them.
Yep, ordinary thiamine in low doses built up with other B vitamins and minerals seems to set the stage for better tolerability of TTFD eventually.
Hi Elliot,
I was wondering if Allithiamine is subject to the same paradoxical effect as TTFD and if so would the glutathione issues be as likely to be the cause of the reaction as it would be with TTFD ?
Thanks,
Michael
Michael,
My understanding is that TTFD stands for “thiamine tetrahydrofurfuryl disulfide” so if your supplement has those words on the label it is also a TTFD product. This seems to currently apply to Thiamax, Lipothiamine, as well as Allithiamine.
You may have already figured this out by now but for anyone like me who is new to this and still learning, I thought I would post this.
Allithiamine is just a brand name. Thiamine inside the bottle of Allithiamine is TTFD