Modern medical practices are plagued with patients who present with chronic, complex, and seemingly treatment resistant illness; illnesses that defy most laboratory testing and abound current diagnostic categories. Some data suggest that 25-75% of symptoms experienced by these patients fall under the umbrella of ‘medically unexplained symptoms’.
What if some of those symptoms were not only explainable but treatable and the expression of these illnesses manifested not from some complicated new disease but from a simple but forgotten nutrient deficiency? What if this nutrient was uniquely critical to mitochondrial competence such that its insufficiency would derail energetic capacity, affect cellular function broadly and diversely, and produce many of the symptoms currently ascribed as medically unexplained? Wouldn’t this be worthy of investigation in your patient population?
That nutrient is thiamine or vitamin B1 and it is essential to mitochondrial energetics – the conversion of food into adenosine triphosphate (ATP). This process is the backbone of all health, and absent sufficient thiamine, it grinds to a halt producing many of the diseases processes vexing modern medicine.
Thiamine is a critical and rate-limiting cofactor to five key enzymes involved in this process, including those at the entry points for the glucose, fatty acid, and amino acid pathways. It has a very short half-life (1-12 hours), limited storage capacity, and is susceptible to depletion and degradation by a number of products that epitomize modern life.
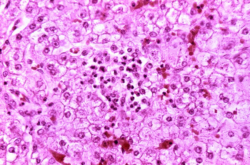
When thiamine is insufficient to overcome these variables, oxidative metabolism falters and the ability to generate molecular energy declines. Over time, aerobic respiration turns anaerobic, oxidative stress increases, and cellular, tissue, and organ function dependent upon steady state energetics deteriorates.
Anaerobic glycolysis, the telltale sign of everything from general metabolic dysfunction to cancer, is, at its root, an adaptive response to insufficient micronutrients like thiamine. Replenish thiamine, recover mitochondrial capacity, and aerobic metabolism and health improve.
Critically Ill Versus Walking Sick: Gradations of Insufficient Thiamine
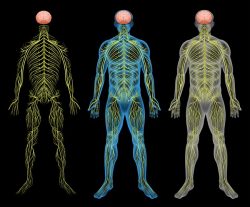
Conventionally, thiamine deficiency syndromes have been described relative to overt, and often later stage illness in the hospital setting. The most common designations include: Wernicke’s encephalopathy marked by nystagmus, ataxia, and cognitive deficits; wet beriberi or high output cardiac failure with edema and dry beriberi, central and peripheral nervous system and cardiovascular disturbances without edema. More recently, sensorimotor polyneuropathy or neuritic beriberi, gastrointestinal dysmotility syndromes, and the dysautonomias have been included in the spectrum, but recognition is lagging.
These designations give the false illusion of a disease process that happens acutely and one that can be categorized by the afflicted organ system. Neither is accurate. While overt thiamine deficiency is certainly a medical emergency and may sometimes develop acutely, the vast majority of cases represent a culmination of years, if not decades, of insufficient thiamine intake relative to need. Until fulminant, these disease processes are marked by low mortality, but high, chronic, and polysymptomatic morbidity. This suggests ample opportunity to treat and prevent more serious illness, improve the patient’s quality of life, and possibly even regain health. Even in overt and emergent cases, where symptomology is obvious, resolution is possible with thiamine repletion.
Thiamine Depleting Factors
Thiamine deficiency is most commonly associated with food insecurity and chronic alcoholism; a narrow view that risks missing early signals of accruing disease across patient populations. Contributors to this deficiency are far more prevalent in first world countries with westernized food production than is recognized. Among the key dietary contributors to insufficient thiamine:
- Alcohol
- Tobacco
- High carbohydrate, highly processed foods
- Coffee, tea, energy drinks
Additionally, the regular use of common medications and/or exposures to environmental chemicals independently and synergistically provoke thiamine deficiency. Every medication and environmental chemical depletes thiamine directly or indirectly by a number of mechanisms including blocking thiamine uptake, increasing its degradation, preventing synthesis in gut microbiota, increasing excretion and/or by inducing mitochondrial damage by other means that then necessitates a higher thiamine intake to compensate. Some of the most commonly used medications are the biggest offenders:
- Metformin
- Antibiotics
- NSAIDs, acetaminophen, and aspirin
- Proton pump inhibitors
- Psychiatric medications
- Diuretics
- Endocrine disrupting medications
- Chemotherapeutic drugs
Sadly, poor dietary habits trigger thiamine insufficiency independently, leading to the prescription of many of these medications, which then further derail thiamine status and mitochondrial capacity. It is an illness spiral that can only be resolved by addressing diet and mitochondrial nutrients like thiamine.
Genetic Contributors to Thiamine Deficiency
While thiamine deficiency diseases are predominantly attributable to diet and lifestyle variables, a number of common genetic polymorphisms in the solute carriers responsible for thiamine uptake, and in enzyme activity involved in thiamine metabolism, increase the demand for thiamine intake. In these cases, disease expression, particularly later in life, represents a latent genetic vulnerability triggered by environmental or lifestyle stressors. Many medication and vaccine reactions fall into this category.
Prevalence Across Patient Groups
Inasmuch as thiamine status is not regularly evaluated in clinical care, it is difficult to know how pervasive thiamine deficiency is within the general population. Moreover, there are no universally accepted cutoffs demarking the progression from suboptimal to frank deficiency. Of the data that do exist, it is likely far more common than recognized across a broad swathe of patient populations.
- 75 – 98% diabetics
- 29% of obese patients, 49% post bariatric surgery
- 20-40% of community dwelling elderly, 48% of elderly patients in acute care
- 55% of cancer patients
- 20% ER patients (random sample)
- 33% congestive heart failure patients
- 20-60% of pregnant women depending upon population tested and methods used
- 30% psychiatric patients
Strikingly, diabetes confers one of the largest risks for thiamine deficiency across patient populations. This is largely do to metabolic derangements (to be discussed in a subsequent post) initiated by the hyperglycemia. These include the increased excretion of thiamine, and interestingly, the endogenous production of the anti-thiamine molecule oxythiamine.
Thiamine Testing
Laboratory assessment of thiamine status varies in sensitivity and specificity, with some tests carrying a high false negative rate (standard serum and plasma), particularly when thiamine status is marginal and with recent intake of thiamine. The two most sensitive tests are whole blood HPLC and the erythrocyte transketolase activity/thiamine pyrophosphate effect combination, neither of which is readily available. Urinary organic acid tests, while indirect, may provide useful patterns for determining the need for thiamine and other mitochondrial nutrients.
How To Recognize Thiamine Insufficiency
In light of the difficulties associated with laboratory testing, clinical acumen is required. Given its role in energy metabolism, lack of energy, in multiple manifestations, is a cardinal indicator of insufficiency.
- Chronic fatigue, muscle weakness, or pain
- Hypersomnia or anorexia
- Dysautonomic reactions – exaggerated, ill-timed, or inadequate autonomic responses to stressors, most notably in the brain, heart and/or GI system
Office observations to support thiamine insufficiency:
- Subtle changes in gait, stability, muscle tone, speech, decrements cognitive or affective acuity or stability
- Asymmetrical pulse pressure, postural hyper- or hypotension, general tachycardia (early stage), bradycardia (later stage)
Standard labs pointing to problems with energy metabolism:
- Elevated creatine/creatinine ratio
- Elevated lactate/lactic acid
- Elevated pyruvate (early stage) or low pyruvate (later stage)
How to Treat
While clinical practice guidelines exist for overt thiamine deficiency in hospital, which include the use of IV thiamine and additional nutrients at a range of doses dependent upon severity, there are no established guidelines for out-patient thiamine deficiency or insufficiency syndromes. This is partly due to its lack of recognition and partly due to the fact that individual need for thiamine, other mitochondrial co-factors, and response to repletion, varies considerably.
There are no known toxicities to high doses, however, there can be negative reactions in the initial phases of thiamine repletion for a subset of patients. These reactions can occur at any dose. In some cases, the reaction involves the specific formulation of thiamine. In other cases, electrolyte disturbances and/or other micronutrient deficiencies unmasked by thiamine are at fault. To mitigate these reactions, thiamine should always be given with magnesium (~50% of the population consumes less than the RDA and magnesium is required to activate thiamine), a clean, lower dose multi-vitamin and a potassium rich diet. It should be noted that additional calcium may also be needed (here, here), especially when dietary calcium has been low for an extended period. Hypophosphatemia may develop as well in patients with recent or extended GI illnesses and/or have a history of low protein consumption and sodium disturbances are also common.
Consider Thiamine
Thiamine is a safe, non-toxic, essential nutrient that has become increasingly difficult to maintain in the face of modern dietary practices and chemical exposures. Thiamine sufficiency is fundamental to energy metabolism, mitochondrial capacity, and thus, health. Consider thiamine in your practice.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.











A great post answering the top questions about thiamine, thanks Dr. Marrs!
I’ve been struggling with post-exertional malaise, though have been taking high dose TTFD (with support nutrients) for about a year. Could depleted riboflavin/glutathione be the culprit? Elliot Overton’s post (https://www.hormonesmatter.com/paradoxical-reactions-with-ttfd-the-glutathione-connection/) suggests an intolerance to TTFD with depleted riboflavin (among other factors). While I am not reacting poorly to TTFD, could it be depleting/requiring high doses of riboflavin (or another nutrient)?
Do you have any suggestions what a “high dose” of riboflavin might be? Or any thoughts why daily energy may be normal, but exercise makes the whole thing go downhill for several days? (Do I simply need more time on TTFD?)
Thanks! 🙂
High dose riboflavin for me is about 100mg across the day. Others require 200+. As with the thiamine, start a lower dose, around 30mg, and see how you do. Increase over time until you find your dose. Also, I found NAD+ to be quite useful for fatigue. You might consider that as well. Finally, make sure the back end of the mitochondria are working well, coQ10 is useful there. The sweet spot for most seems to be ~200-250mg. Although of course, as with all of this, it varies.